Abstract
Background
The post-hospitalization period is a precarious time for patients. Post-discharge nurse telephone call programs aiming to prevent unnecessary readmissions have had mixed results.
Objective
Describe a primary-care based program to identify and address problems arising after hospital discharge.
Design
A quality improvement program embedding registered nurses in a primary care practice to call patients within 72 h of hospital discharge and route problems within the practice for real-time resolution.
Participants
Adult patients with a primary care provider in the general internal medicine practice at the University of California San Francisco who were discharged home from the Medicine service.
Main Measures
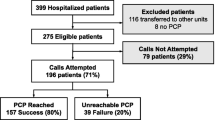
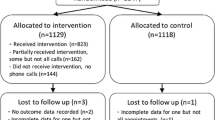
Patients reached directly by phone had a ‘full-scripted encounter;’ those reached only by voice-mail had a ‘message-scripted encounter;’ those not reached despite multiple attempts had a ‘missed encounter.’ Among patients with full-scripted encounters, we identified and cataloged problems arising after hospital discharge and measured the proportion of calls in which a problem was uncovered. For the different encounter types, we compared follow-up appointment attendance and 30-day readmission rates.
Key Results
Of 790 eligible discharges, 486 had a full-scripted, 229 a message-scripted and 75 a missed encounter. Among the 486 full-scripted encounters, nurses uncovered at least one problem in 371 (76 %) discharges, 25 % of which (n = 94) included new symptoms, and 47 % (n = 173) included medication issues. Discharges with full-scripted and message-scripted encounters were associated with higher follow-up appointment attendance rates compared with those with missed encounters (60.1 %, 58.5 %, 38.5 % respectively p = 0.004). There was no significant difference in 30-day readmission rates (12.8 %, 14.8 %, 14.7 %; p = 0.72).
Conclusions
Our results suggest that centering a post-discharge phone call program within the primary care practice improves post-hospital care by identifying clinical and care-coordination problems early. With the new Medicare transitional care payment, such programs could become an important, self-sustaining part of the patient-centered medical home.


Similar content being viewed by others
References
Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141(7):533–536. PubMed PMID: 15466770.
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi:10.1056/NEJMsa0803563. PubMed PMID: 19339721.
Moore C, Wisnivesky J, Williams S, McGinn T. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18(8):646–651. PubMed PMID: 12911647; PubMed Central PMCID: PMC1494907.
Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528. doi:10.7326/0003-4819-155-8-201110180-00008. PubMed PMID: 22007045.
Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;4, CD004510. doi:10.1002/14651858.CD004510.pub3. PubMed PMID: 17054207.
Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;23(8):1228–1233. doi:10.1007/s11606-008-0618-9. PubMed PMID: 18452048; PubMed Central PMCID: PMC2517968.
Crocker JB, Crocker JT, Greenwald JL. Telephone follow-up as a primary care intervention for postdischarge outcomes improvement: a systematic review. Am J Med. 2012;125(9):915–921. doi:10.1016/j.amjmed.2012.01.035. PubMed PMID: 22938927.
Costantino ME, Frey B, Hall B, Painter P. The Influence of a Postdischarge Intervention on Reducing Hospital Readmissions in a Medicare Population. Popul Health Manag. 2013. doi:10.1089/pop.2012.0084. PubMed PMID: 23537154.
Graham J, Tomcavage J, Salek D, Sciandra J, Davis DE, Stewart WF. Postdischarge monitoring using interactive voice response system reduces 30-day readmission rates in a case-managed Medicare population. Med Care. 2012;50(1):50–57. doi:10.1097/MLR.0b013e318229433e. PubMed PMID: 21822152.
Bindman AB, Blum JD, Kronick R. Medicare’s transitional care payment–a step toward the medical home. N Engl J Med. 2013;368(8):692–694. doi:10.1056/NEJMp1214122. PubMed PMID: 23425161.
Tang N. A primary care physician’s ideal transitions of care–where’s the evidence? J Hosp Med Official Publ Soc Hosp Med. 2013;8(8):472–477. doi:10.1002/jhm.2060. PubMed PMID: 23873732.
Acknowledgements
Contributors
We would like to thank Rosemary Lam for administrative and analytic support, Angela Sherwood and Kelly Flannery for their outstanding nursing and communication skills, and Kathie Buchanan and Eva Turner for their support of the DGIM nurse follow-up phone call program.
Funders
This study was funded by a grant from the Mount Zion Health Fund at UCSF.
Prior Presentations
Presented as a poster at the 2013 Society of General Internal Medicine Annual Meeting on April 26, 2012 and at the 2013 AcademyHealth Annual Research Meeting on June 23, 2013.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tang, N., Fujimoto, J. & Karliner, L. Evaluation of a Primary Care-Based Post-Discharge Phone Call Program: Keeping the Primary Care Practice at the Center of Post-hospitalization Care Transition. J GEN INTERN MED 29, 1513–1518 (2014). https://doi.org/10.1007/s11606-014-2942-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-2942-6