Abstract
BACKGROUND
Hospitals face increased pressure to improve their quality of care in an environment of dwindling hospital payments. It is unclear whether lower hospital margins are associated with worse quality of care or closure.
OBJECTIVE
To determine the association of hospital margins with quality of care and changes in operating status.
DESIGN, SUBJECTS, AND MAIN MEASURES
We conducted an observational cross-sectional study analyzing hospitals’ margin, quality of care (process quality, risk-adjusted readmission rates, and risk-adjusted mortality rates), and changes in operating status (rates of closure, merger and acquisition, and conversion to a critical access hospital) for 3,262 non-public U.S. hospitals with data from the Hospital Quality Alliance and Medicare Cost Reports.
KEY RESULTS
Compared to those in the bottom 10% of operating margin, those in the top 10% had higher process quality (e.g. 95.3 vs. 93.7, p = 0.002 for acute myocardial infarction [AMI]) and lower readmission rates (e.g. 19.7% vs. 22.4%, p < 0.001 for AMI). We found no association between margins and mortality rates. Hospitals in the bottom 10% were more likely than those in the top 10% to close (5.7% vs. 2.0%), merge or become acquired (4.0% vs. 0.3%), or convert to a Critical Access Hospital (5.4% vs. 0.6%). Over 15% of hospitals in the lowest decile of hospital margin changed operating status in the subsequent year.
CONCLUSIONS
Low hospital margins are associated with worse processes of care and readmission rates and with changes in operating status. We should monitor low-margin hospitals closely for declining quality of care.

Similar content being viewed by others
References
Medicare Payment Advisory Commission (MedPAC). A data book: Healthcare spending and the Medicare program. Washington: MedPAC; 2005.
Medicare Payment Advisory Commission (MedPAC). Report to the Congress: Medicare payment policy. Available at: http://www.medpac.gov/documents/Mar10_EntireReport.pdf. Accessed July 20, 2011.
Hibbard JH, Stockard J, Tusler M. Hospital performance reports: impact on quality, market share, and reputation. Health Aff (Millwood). 2005;24:1150–60.
Encinosa WE, Bernard DM. Hospital finances and patient safety outcomes. Inquiry. 2005;42:60–72.
Bazzoli GJ, Chen HF, Zhao M, et al. Hospital financial condition and the quality of patient care. Health Econ. 2008;17:977–95.
Volpp KG, Konetzka RT, Zhu J, et al. Effect of cuts in Medicare reimbursement on process and outcome of care for acute myocardial infarction patients. Circulation. 2005;112:2268–75.
Williams D, Hadley J, Pettengill J. Profits, community role, and hospital closure: an urban and rural analysis. Med Care. 1992;30:174–87.
Duffy SQ, Friedman B. Hospitals with chronic financial losses: what came next? Health Aff (Millwood). 1993;12:151–63.
Pink GH, Howard A, Holmes GM, et al. Differences in measurement of operating margin. Available at: http://flexmonitoring.org/documents/BriefingPaper17_OperatingMargin.pdf. Accessed July 20, 2011.
Hackbarth GM. Report to the Congress: Medicare payment policy. Available at: http://www.medpac.gov/documents/Mar09_March%20report%20testimony_WM%20FINAL.pdf. Accessed July 20, 2011.
Angrist JD, Krueger AB. Empirical strategies in labor economics. In: Card D, Ashenfelter O, eds. Handbook of labor economics: Elsevier Science; 2000.
Pink GH, Holmes GM, D'Alpe C, et al. Financial indicators for Critical Access Hospitals. Available at: http://www.flexmonitoring.org/documents/BriefingPaper7_FinancialIndicators.pdf. Accessed July 20, 2011.
Anderson RJ, Boumbulian PJ, Pickens SS. The role of U.S. public hospitals in urban health. Acad Med. 2004;79:1162–8.
Kahn CN 3rd, Ault T, Isenstein H, et al. Snapshot of hospital quality reporting and pay-for-performance under Medicare. Health Aff (Millwood). 2006;25:148–62.
Bernheim SM, Lin Z, Bhat KR, et al. 2010 measures maintenance technical report: Acute myocardial infarction, heart failure, and pneumonia 30-Day risk-standardized readmission measures. Available at: http://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1219069855841. Accessed July 20, 2011.
The Joint Commission. Population and sampling specifications. Available at: http://manual.jointcommission.org/releases/TJC2010A/SamplingChapterTJC.html. Accessed July 20, 2011.
Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Rural Assistance Center. CAH frequently asked questions. Available at: http://www.raconline.org/info_guides/hospitals/cahfaq.php#whatis. Accessed July 20, 2011.
Schoenman JA, Sutton JP. Impact of CAH conversion on hospital finances and mix of inpatient services. Available at: http://www.norc.org/NR/rdonlyres/A91D9471-49FD-4881-994F-51DACEBC7577/0/ImpactofCAHConversion_FinalReport_NORC.pdf. Accessed July 20, 2011.
Sheikh K, Bullock C. Urban-rural differences in the quality of care for Medicare patients with acute myocardial infarction. Arch Intern Med. 2001;161:737–43.
Baldwin LM, MacLehose RF, Hart LG, et al. Quality of care for acute myocardial infarction in rural and urban US hospitals. J Rural Health. 2004;20:99–108.
Smedley BD, Stith AY, Nelson AR. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington: National Academy Press; 2003.
Jha AK, Epstein AM. The predictive accuracy of the New York State coronary artery bypass surgery report-card system. Health Aff (Millwood). 2006;25:844–55.
Acknowledgments
We would like to acknowledge George H. Pink for his help with calculating the hospital margins.
Funding
None disclosed.
Conflicts of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Online Appendix
Below is the link to the electronic supplementary material.
Appendix Table 1
Hospital Quality Alliance Performance Measures for Acute Myocardial Infarction, Congestive Heart Failure, and Pneumonia in 2007 (DOC 31 kb)
Appendix Table 2
The Association of Operating Margin and Performance on Process Indicators, Risk Adjusted Readmissions, and Risk Adjusted Mortality Rates: Coefficients on Operating Margin (DOC 34 kb)
Appendix Table 3
The Association of Total Margin and Quality Performance Measured by Process Indicators, Risk Adjusted 30-day Readmissions, and Risk Adjusted 30-day Mortality (DOC 21.0 kb)
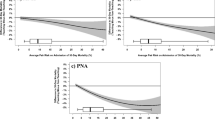
Appendix Figure 1
The Association of Total Margin and Rates of Closure, Merger/Acquisition, or Conversion to a Critical Access Hospital in 2005 (DOC 52 kb)
Rights and permissions
About this article
Cite this article
Ly, D.P., Jha, A.K. & Epstein, A.M. The Association Between Hospital Margins, Quality of Care, and Closure or Other Change in Operating Status. J GEN INTERN MED 26, 1291–1296 (2011). https://doi.org/10.1007/s11606-011-1815-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1815-5