Abstract
Objective(s)
Higher-volume centers demonstrate better perioperative outcomes for complex surgical interventions, though resource utilization implications of this hospital-level variation are unclear. We hypothesized that for hepatic lobectomy, higher operative volume correlates with better outcomes and lower costs.
Methods
From 2009 to 2011, 4163 patients undergoing hepatic lobectomy were identified from the University HealthSystems Consortium database. Univariate, multivariate logistic regression, and decision analytic models were constructed to identify differences in hospital utilization and cost. Cost included both index and readmission hospitalizations, when applicable.
Results
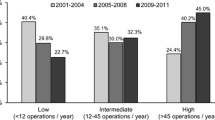
The annual number of hepatic lobectomies performed by the institutions within the study ranged from 1 to 86. The median age of the 4163 patients was 58 years with a roughly equal gender split (M/F 49 %:51 %) and a racial breakdown which reflected that of the general US population. For all patients, the overall perioperative mortality rate was 2.3 % and the 30-day readmission rate was 13.4 %. Hospitals performing >30 hepatic lobectomies per year had significantly lower mortality and readmission rates than those hospitals performing ≤15 lobectomies annually (both p < 0.05). On multivariate analysis, higher severity of illness (odd ratio (OR) 2.13, 95 % confidence interval (CI) [1.48–3.07], p < 0.001), discharge to rehab (OR 1.84, [1.28–2.64], p < 0.001), home with home health care (OR 1.38, [1.08–1.76], p = 0.01), and surgery at a low-volume hospital (OR 1.49, [1.18–1.88], p < 0.001) were significant predictors of readmission. Conversely, surgical intervention at high-volume centers was associated with decreased risk of readmission (OR 0.67, [0.53–0.85], p < 0.001). When both index and readmission costs were considered, per-patient cost at low-volume centers was 21.9 % higher than at high-volume centers ($19,669 vs. $16,137). Sensitivity analyses adjusting for perioperative mortality and readmission at all centers did not significantly change the analysis.
Conclusions
These data, for the first time, demonstrate that hospital volume in hepatic lobectomy is an important, modifiable risk factor for readmission and cost. To optimize resource utilization, patients undergoing complex hepatic surgery should be directed to higher-volume surgical institutions.



Similar content being viewed by others
References
Glick, H.A., et al., Comparative effectiveness and cost-effectiveness analyses frequently agree on value. Health Aff (Millwood), 2015. 34(5): p. 805–11.
Naylor, M.D., et al., Unintended consequences of steps to cut readmissions and reform payment may threaten care of vulnerable older adults. Health Aff (Millwood), 2012. 31(7): p. 1623–32.
Goozner, M., Readmissions penalties at work. Effort pushed most hospitals to reduce or eliminate penalties in second year. Mod Healthc, 2013. 43(33): p. 25.
Zigmond, J., Avoiding the penalty box. New rules on readmissions push hospitals, post-acute providers into closer collaboration. Mod Healthc, 2012. 42(5): p. 38–9.
Jweinat, J.J., Hospital readmissions under the spotlight. J Healthc Manag, 2010. 55(4): p. 252–64.
Hunter, T., J.R. Nelson, and J. Birmingham, Preventing readmissions through comprehensive discharge planning. Prof Case Manag, 2013. 18(2): p. 56–63; quiz 64–5.
Kagedan, D.J., et al., Enhanced recovery after pancreatic surgery: a systematic review of the evidence. HPB (Oxford), 2015. 17(1): p. 11–6.
Hall, T.C., et al., Enhanced recovery programmes in hepatobiliary and pancreatic surgery: a systematic review. Ann R Coll Surg Engl, 2012. 94(5): p. 318–26.
Thiele, R.H., et al., Standardization of care: impact of an enhanced recovery protocol on length of stay, complications, and direct costs after colorectal surgery. J Am Coll Surg, 2015. 220(4): p. 430–43.
Abbott, A.M., et al., Short-term outcomes after combined colon and liver resection for synchronous colon cancer liver metastases: a population study. Ann Surg Oncol, 2013. 20(1): p. 139–47.
Wicherts, D.A., et al., Short- and long-term results of extended left hepatectomy for colorectal metastases. HPB (Oxford), 2011. 13(8): p. 536–43.
Paik, K.Y., et al., Improved survival following right trisectionectomy with caudate lobectomy without operative mortality: surgical treatment for hilar cholangiocarcinoma. J Gastrointest Surg, 2008. 12(7): p. 1268–74.
Birkmeyer, J.D., et al., Hospital volume and surgical mortality in the United States. N Engl J Med, 2002. 346(15): p. 1128–37.
Wilson, G.C., et al., Cost-effectiveness of total pancreatectomy and islet cell autotransplantation for the treatment of minimal change chronic pancreatitis. J Gastrointest Surg, 2015. 19(1): p. 46–54; discussion 54–5.
Sutton, J.M., et al., Cost effectiveness after a pancreaticoduodenectomy: bolstering the volume argument. HPB (Oxford), 2014. 16(12): p. 1056–61.
Abbott, D.E., et al., Cost-effectiveness of simultaneous resection and RFA versus 2-stage hepatectomy for bilobar colorectal liver metastases. J Surg Oncol, 2014. 109(6): p. 516–20.
Tzeng, C.W., et al., Frequency and intensity of postoperative surveillance after curative treatment of pancreatic cancer: a cost-effectiveness analysis. Ann Surg Oncol, 2013. 20(7): p. 2197–203.
Sutton, J.M., et al., Readmission After Pancreaticoduodenectomy: The Influence of the Volume Effect Beyond Mortality. Ann Surg Oncol, 2015.
Heisler, M., et al., Medicaid managed care: are academic medical centers penalized by attracting patients with high-cost conditions? Am J Manag Care, 2003. 9(1): p. 19–29.
Neuhausen, K., et al., Disproportionate-share hospital payment reductions may threaten the financial stability of safety-net hospitals. Health Aff (Millwood), 2014. 33(6): p. 988–96.
Author information
Authors and Affiliations
Corresponding author
Additional information
Primary Discussant
Pierpaolo Sileri, M.D., Ph.D (Rome, Italy)
I congratulate the authors on a well-written and executed study evaluating the volume effect on hospital cost.
As the authors indicate, this an important topic on hospital quality that is increasingly gaining the attention of insurance companies and policy makers.
I have the follow two questions regarding the data presented.
1. The procedure selected for analysis was hepatic lobectotomy should be clarified. Do the authors mean ICD 9 code 50.3 lobectomy of liver? ICD 9 50.2 includes a variety of liver directed procedures including ablation, partial hepatectomy, and wedge resections. Since this cohort of patients would lead to a wide variation in perioperative outcomes, I suspect the data collected was indeed specific to ICD 9 50.3 and not 50.2?
In any case, assuming the data was derived by using the ICD 9, 50. 3—specifying hepatic lobectomy, there still exists significant variation in nomenclature for hepatectomies in the US and not all hepatic lobectomies are the same in terms of the procedure (level of difficulty, or method; lap vs. open), and associated morbidity and perioperative outcomes—including cost. There are documented differences in outcomes between patients undergoing “Right hepatectomy” vs “Left hepatectomy.” Especially if the data collected under “lobectomy” included patients who underwent a left lobectomy (Left lateral -sectionectomy) erroneously coded as a “hepatic lobectomy.” Regardless, I do think that separating “hepatic lobectomy into two groups: Left-sided vs. Right sided would be important to support the authors’ important findings.
2. The authors mention that the hospital variable, length of stay was combined to include overall and surgical ICU stay. I think it is important to separate the overall hospital stay from the ICU stay because very likely, the use of ICU or length of ICU stay might be the most important variable in identifying the main reason for difference in cost between high volume centers from low volume centers. It is my belief that high volume center providers (not only the surgeons, but also the anesthesiologists and ward nursing staff) are more accustomed and comfortable caring this type of patient population and as a result less commonly admit patients immediately postoperatively to the ICU. Certainly, this would lower the overall hospital cost significantly. This type of granular data would certainly strengthen the authors’ findings and support their conclusions from a cost/quality prospective that these procedures should be referred to high volume centers.
Again, I would like to complement the authors on an important and well executed study.
Closing Discussant
Dr. Hoehn
1. Response: For this manuscript we analyzed patients with the ICD-9 procedure code 50.3 which represents hepatic lobectomy. We agree that this is a collection of both right and left hepatectomies, which are indeed different procedures. While this is undoubtedly a heterogeneous group—as so many retrospective cohorts are—all procedures represent complex hepatobiliary surgery, which was the focus of this analysis. Future modeling for procedures of varying complexity will benefit from more homogenous procedure cohorts.
Response: This is an excellent point. Undoubtedly, ICU utilization will affect overall cost, and differences in ICU length of stay may very well contribute to our findings. Both ICU and overall length of stay were included in our multivariate analysis of readmission, but were not specifically included in the cost-effectiveness model, as there was little variability between the hospital volume tertiles. However, to address your point, our group is currently investigating specific differences in resource utilization between these groups of hospitals (including ICU care, the use of imaging and labs, administration of blood products, etc.) as we attempt a more granular explanation to our findings. Thank you for this suggestion.
Rights and permissions
About this article
Cite this article
Sutton, J.M., Hoehn, R.S., Ertel, A.E. et al. Cost-Effectiveness in Hepatic Lobectomy: the Effect of Case Volume on Mortality, Readmission, and Cost of Care. J Gastrointest Surg 20, 253–261 (2016). https://doi.org/10.1007/s11605-015-2964-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2964-3