Abstract
Introduction
In-hospital biliary complications (BCs) after liver transplantation (LT) are reported in up to 20 % of patients and contribute to poor outcomes and increased costs. Existing single-center outcome and cost analyses studies are limited in scope.
Methods
This is a cross-sectional analysis of national data involving 7,967 patients transplanted between 2011 and 2012 with the primary aim of determining the association between BCs and clinical outcomes and costs. Age, race, diagnosis, and severity of illness are associated with the development of BCs.
Results
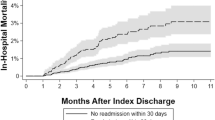
BCs develop in 14.6 % of LT recipients and have substantial implications for perioperative outcomes, including length of hospital and ICU stay (27.9 vs 19.6 mean days, p < 0.001 and 12.0 vs 8.3 mean days, p < 0.001, respectively), in-hospital morbidity (39 vs 27 %, p < 0.001), 30-day readmissions (14.8 vs 11.2 %, p < 0.001), and in-hospital mortality (5.8 vs 4.0 %, p < 0.001). BCs contributed to a mean increase in in-hospital costs of $36,212 (p < 0.001), due to increases in accommodations ($9,539, p < 0.001), surgical services ($3,988, p < 0.001), and pharmacy services ($8,445, p < 0.001).
Discussion
BCs are a predominant etiology for in-hospital morbidity and mortality, while contributing significantly to the high cost of LT. Efforts should be focused on understanding salient and modifiable risk factors, while developing innovative strategies to reduce BCs.


Similar content being viewed by others
Abbreviations
- BCs:
-
Biliary complications
- LT:
-
Liver transplantation
- DCD:
-
Donation after cardiac death
- UHC:
-
University HealthSystem Consortium
- ICU:
-
Intensive care unit
- LOS:
-
Length of stay
- GI:
-
Gastrointestinal
- NEC:
-
Not elsewhere classified
- NOS:
-
Not otherwise specified
- ICD-9:
-
International Statistical Classification of Diseases and Related Health Problems
- US:
-
United States
References
Colonna JO, 2nd, Shaked A, Gomes AS, Colquhoun SD, Jurim O, McDiarmid SV, et al. Biliary strictures complicating liver transplantation. Incidence, pathogenesis, management, and outcome. Ann Surg. 1992;216(3):344–50; discussion 50–2.
Heidenhain C, Heise M, Jonas S, Ben-Asseur M, Puhl G, Mittler J, et al. Retrograde reperfusion via vena cava lowers the risk of initial nonfunction but increases the risk of ischemic-type biliary lesions in liver transplantation—a randomized clinical trial. Transpl Int. 2006;19(9):738–48.
Neuhaus P, Blumhardt G, Bechstein WO, Steffen R, Platz KP, Keck H. Technique and results of biliary reconstruction using side-to-side choledochocholedochostomy in 300 orthotopic liver transplants. Ann Surg. 1994;219(4):426–34.
Sanchez-Urdazpal L, Gores GJ, Ward EM, Maus TP, Wahlstrom HE, Moore SB, et al. Ischemic-type biliary complications after orthotopic liver transplantation. Hepatology. 1992;16(1):49–53.
Adam R, Bismuth H, Diamond T, Ducot B, Morino M, Astarcioglu I, et al. Effect of extended cold ischaemia with UW solution on graft function after liver transplantation. Lancet. 1992;340(8832):1373–6.
Qian YB, Liu CL, Lo CM, Fan ST. Risk factors for biliary complications after liver transplantation. Arch Surg. 2004;139(10):1101–5.
Azoulay D, Castaing D, Adam R, Savier E, Delvart V, Karam V, et al. Split-liver transplantation for two adult recipients: feasibility and long-term outcomes. Ann Surg. 2001;233(4):565–74.
Lallier M, St-Vil D, Luks FI, Laberge JM, Bensoussan AL, Guttman FM, et al. Biliary tract complications in pediatric orthotopic liver transplantation. J Pediatr Surg. 1993;28(9):1102–5.
Martelius T, Krogerus L, Hockerstedt K, Bruggeman C, Lautenschlager I. Cytomegalovirus infection is associated with increased inflammation and severe bile duct damage in rat liver allografts. Hepatology. 1998;27(4):996–1002.
Moser MA, Wall WJ. Management of biliary problems after liver transplantation. Liver Transpl. 2001;7(11 Suppl 1):S46-52.
Baccarani U, Isola M, Adani GL, Avellini C, Lorenzin D, Rossetto A, et al. Steatosis of the hepatic graft as a risk factor for post-transplant biliary complications. Clin Transplant. 2010;24(5):631–5.
Evans RW, Manninen DL, Dong FB. An economic analysis of liver transplantation. Costs, insurance coverage, and reimbursement. Gastroenterol Clin North Am. 1993;22(2):451–73.
Engelhardt HT, Jr. Shattuck lecture—allocating scarce medical resources and the availability of organ transplantation. Some moral presuppositions. N Engl J Med. 1984;311(1):66–71.
Sanchez-Urdazpal L, Gores GJ, Ward EM, Maus TP, Buckel EG, Steers JL, et al. Diagnostic features and clinical outcome of ischemic-type biliary complications after liver transplantation. Hepatology. 1993;17(4):605–9.
Kiuchi T, Ishiko T, Nakamura T, Egawa H, Uemoto S, Inomata Y, et al. Duct-to-duct biliary reconstruction in living donor liver transplantation. Transplant Proc. 2001;33(1–2):1320–1.
Englesbe MJ, Dimick J, Mathur A, Ads Y, Welling TH, Pelletier SJ, et al. Who pays for biliary complications following liver transplant? A business case for quality improvement. Am J Transplant. 2006;6(12):2978–82.
Kling K, Lau H, Colombani P. Biliary complications of living related pediatric liver transplant patients. Pediatr Transplant. 2004;8(2):178–84.
Gunawansa N, McCall JL, Holden A, Plank L, Munn SR. Biliary complications following orthotopic liver transplantation: a 10-year audit. HPB (Oxford). 2011;13(6):391–9.
Fan ST, Lo CM, Liu CL, Tso WK, Wong J. Biliary reconstruction and complications of right lobe live donor liver transplantation. Ann Surg. 2002;236(5):676–83.
Heidenhain C, Pratschke J, Puhl G, Neumann U, Pascher A, Veltzke-Schlieker W, et al. Incidence of and risk factors for ischemic-type biliary lesions following orthotopic liver transplantation. Transpl Int. 2010;23(1):14–22.
Moench C, Moench K, Lohse AW, Thies J, Otto G. Prevention of ischemic-type biliary lesions by arterial back-table pressure perfusion. Liver Transpl. 2003;9(3):285–9.
Theruvath TP, Zhong Z, Pediaditakis P, Ramshesh VK, Currin RT, Tikunov A, et al. Minocycline and N-methyl-4-isoleucine cyclosporin (NIM811) mitigate storage/reperfusion injury after rat liver transplantation through suppression of the mitochondrial permeability transition. Hepatology. 2008;47(1):236–46.
Kato H, Amersi F, Buelow R, Melinek J, Coito AJ, Ke B, et al. Heme oxygenase-1 overexpression protects rat livers from ischemia/reperfusion injury with extended cold preservation. Am J Transplant. 2001;1(2):121–8.
Chavin KD, Taber DJ, Norcross M, Pilch NA, Crego H, McGillicuddy JW, et al. Safe use of highly steatotic livers by utilizing a donor/recipient clinical algorithm. Clin Transplant. 2013;27(5):732–41.
Nativ NI, Maguire TJ, Yarmush G, Brasaemle DL, Henry SD, Guarrera JV, et al. Liver defatting: an alternative approach to enable steatotic liver transplantation. Am J Transplant. 2012;12(12):3176–83.
Marty FM, Winston DJ, Rowley SD, Vance E, Papanicolaou GA, Mullane KM, et al. CMX001 to prevent cytomegalovirus disease in hematopoietic-cell transplantation. N Engl J Med. 2013;369(13):1227–36.
Acknowledgments
No extramural funding source associated with this study.
Conflict of Interest
No authors have any competing interests. An ethics statement was not required for this work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Arun P. Palanisamy and D. J. Taber contributed equally to this work.
Rights and permissions
About this article
Cite this article
Palanisamy, A.P., Taber, D.J., Sutter, A.G. et al. Clinical Outcomes and Costs Associated with In-hospital Biliary Complications After Liver Transplantation: a Cross-Sectional Analysis. J Gastrointest Surg 19, 282–289 (2015). https://doi.org/10.1007/s11605-014-2675-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2675-1