Abstract
Introduction
To induce rapid hepatic hypertrophy and to reduce post-hepatectomy liver failure (PHLF), associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) has been recently developed for patients with a limited future liver remnant. The aim of this study was to further assess the perioperative risk of this procedure and its specific indications.
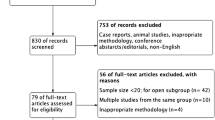
Patients and Methods
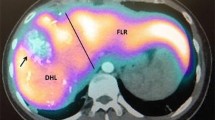
The study was performed between November 2010 and April 2012 for patients undergoing right trisectionectomy by the ALPPS approach. Liver volume, intra- and postoperative complications, including PHLF, and residual tumour status were compared for patients with different diagnoses.
Results
The interval between two operations in nine patients undergoing ALPPS was 13 days (median). Sufficient hepatic hypertrophy was achieved with a volume gain of 87.2 % (median). All patients underwent right trisectionectomy without residual tumours. In contrast to six patients with uneventful intra- and postoperative course, bile leak, vancomycin-resistant enterococcus infection, PHLF and sepsis developed in two of three patients with hilar cholangiocarcinoma as the preoperative diagnosis.
Conclusion
ALPPS leads to sufficient hepatic hypertrophy within 2 weeks, avoiding PHLF in most patients. In patients with hilar cholangiocarcinoma, ALPPS should be applied with extreme caution due to high morbidity and mortality.


Similar content being viewed by others
References
Clavien PA, Oberkofler CE, Raptis DA, Lehmann K, Rickenbacher A, El-Badry AM. What is critical for liver surgery and partial liver transplantation: size or quality? Hepatology 2010;52:715–729.
Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunvén P et al. Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery 1990;107:521–527.
Nagino M, Kamiya J, Nishio H, Ebata T, Arai T, Nimura Y. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg 2006;243:364–372.
Adam R, Laurent A, Azoulay D, Castaing D, Bismuth H. Two-stage hepatectomy: A planned strategy to treat irresectable liver tumors. Ann Surg 2000;232:777–785.
Jaeck D, Oussoultzoglou E, Rosso E, Greget M, Weber JC, Bachellier P. A two-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple and bilobar colorectal liver metastases. Ann Surg 2004;240:1037–1049
Clavien PA, Petrowsky H, DeOliveira ML, Graf R. Strategies for safer liver surgery and partial liver transplantation. N Engl J Med 2007;356:1545–1559.
Abulkhir A, Limongelli P, Healey AJ, Damrah O, Tait P, Jackson J, Habib N, Jiao LR. Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg 2008; 247: 49–57.
Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 2012;255:405–414.
de Santibañes E, Clavien PA. Playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg 2012;255:415–417.
Radtke A, Sotiropoulos GC, Nadalin S, Molmenti EP, Schroeder T, Lang H et al. Preoperative volume prediction in adult living donor liver transplantation: how much can we rely on it? Am J Transplant 2007;7:672–679.
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011;149:713–724.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–213.
Clavien PA, de Santibañes E. The ALPPS: Time to Explore! Ann Surg 2012;25:e18-9.
Imamura H, Makuuchi M, Sakamoto Y, Sugawara Y, Sano K, Nakayama A et al. Anatomical keys and pitfalls in living donor liver transplantation. J Hepatobiliary Pancreat Surg 2000;7:380–94.
Deshpande RR, Heaton ND, Rela M. Surgical anatomy of segmental liver transplantation. Br J Surg 2002;89:1078–1088.
de Santibañes E, Alvarez FA, Ardiles V. How to avoid postoperative liver failure: a novel method. World J Surg 2012;36:125–128.
Shigeta H, Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H et al. Bacteremia after hepatectomy: an analysis of a single-center, 10-year experience with 407 patients. Langenbecks Arch Surg 2002;387:117–124.
Hochwald SN, Burke EC, Jarnagin WR, Fong Y, Blumgart LH. Association of preoperative biliary stenting with increased postoperative infectious complications in proximal cholangiocarcinoma. Arch Surg 1999;134:261–266.
Kawarada Y, Das BC, Taoka H. (2000) Anatomy of the hepatic hilar area: the plate system. J Hepatobiliary Pancreat Surg 7:580–586.
Nagino M, Kamiya J, Arai T, Nishio H, Ebata T, Nimura Y. “Anatomic” right hepatic trisectionectomy (extended right hepatectomy) with caudate lobectomy for hilar cholangiocarcinoma. Ann Surg 2006;243:28–32.
Palavecino M, Abdalla EK, Madoff DC, Vauthey JN. Portal vein embolization in hilar cholangiocarcinoma. Surg Oncol Clin N Am 2009;18:257–267.
Author information
Authors and Affiliations
Corresponding author
Additional information
This manuscript was selected and presented at the “Best Oral Session” at the 10th World Congress of the IHPBA in Paris on 4 July, 2012.
Rights and permissions
About this article
Cite this article
Li, J., Girotti, P., Königsrainer, I. et al. ALPPS in Right Trisectionectomy: a Safe Procedure to Avoid Postoperative Liver Failure?. J Gastrointest Surg 17, 956–961 (2013). https://doi.org/10.1007/s11605-012-2132-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-012-2132-y