Abstract
Background
Many surgeons feel comfortable performing antireflux surgery (ARS) on the basis of symptomatic evaluation, endoscopy, and barium esophagography. While esophageal manometry is often obtained to assess esophageal peristalsis, pH monitoring is rarely considered necessary to confirm the diagnosis of gastroesophageal reflux disease (GERD).
Aims
The aim of this study was to analyze the sensitivity and specificity of symptoms, endoscopy, barium esophagography, and manometry as compared to pH monitoring in the preoperative evaluation of patients for ARS.
Patients and Methods
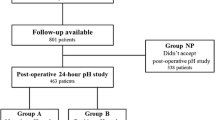
One hundred and thirty-eight patients were referred for ARS with a diagnosis of GERD based on symptoms, endoscopy, and/or barium esophagography. Barium esophagography, esophageal manometry, and ambulatory 24-h pH monitoring were performed preoperatively in every patient.
Results
Four patients were found to have achalasia and were excluded from the analysis. Based on the presence or absence of gastroesophageal reflux on pH monitoring, the remaining 134 patients were divided into two groups: GERD+ (n = 78, 58 %) and GERD− (n = 56, 42 %). The groups were compared with respect to the incidence of symptoms, presence of reflux and hiatal hernia on esophagogram, endoscopic findings, and esophageal motility. There was no difference in the incidence of symptoms between the two groups. Within the GERD+ group, 37 patients (47 %) had reflux at the esophagogram and 41 (53 %) had no reflux. Among the GERD− patients, 17 (30 %) had reflux and 39 (70 %) had no reflux. A hiatal hernia was present in 40 and 32 % of patients, respectively. Esophagitis was found at endoscopy in 16 % of GERD+ patients and in 20 % of GERD− patients. Esophageal manometry showed no difference in the pressure of the lower esophageal sphincter or quality of peristalsis between the two groups.
Conclusions
The results of this study showed that (a) symptoms were unreliable in diagnosing GERD, (b) the presence of reflux or hiatal hernia on esophagogram did not correlate with reflux on pH monitoring, (c) esophagitis on endoscopy had low sensitivity and specificity, and (d) manometry was mostly useful for positioning the pH probe and rule out achalasia. Ambulatory 24-h pH monitoring should be routinely performed in the preoperative work-up of patients suspected of having GERD in order to avoid unnecessary ARS.
Similar content being viewed by others
References
Dent J, El Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2005;54:710–717.
Campos GM, Peters JH, DeMeester TR, Oberg S, Crookes PF, Tan S, DeMeester SR, Hagen J, Bremner CG. Multivariate analysis of factors predicting outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg 1999;3:292–300.
Waring JP, Hunter JG, Oddsdottir M, Wo J, Katz E. The preoperative evaluation of patients considered for laparoscopic surgery. Am J Gastroenterol 1995;90:35–38.
Khajanchee YS, Hong D, Hansen PD, Swanstrom LL. Outcomes of antireflux surgery in patients with normal preoperative 24-hour pH test results. Am J Surg 2004;187:599–603.
Armstrong D, Monnier P, Nicolet M, Blum Al, Savary M. The “MUSE” system. In: R. Giuli, GNJ Tyagt, TR DeMeester, JP Galmiche (eds) The Esophageal mucosa. New York, Elsevier, 1994.
Jamieson JR, Stein HJ, DeMeester TR, Bonavina L, Schwizer W, Hinder RA, Albertucci M. Ambulatory 24-h esophageal pH monitoring: normal values, optimal thresholds, specificity, sensitivity and reproducibility. Am J Gastroenterol 1992;87:1102–1111.
Patti MG, Arcerito M, Tong J, de Pinto M, de Bellis M, Wang A, Feo CV, Mulvhill SJ, Way LW. Importance of preoperative and postoperative pH monitoring in patients with esophageal achalasia. J Gastrointest Surg 1997;1:505–510.
Patti MG, Diener U, Tamburini A, Molena D, Way LW. Role of esophageal function tests in the diagnosis of gastroesophageal reflux disease. Dig Dis Sci 2001;46:597–602.
Csendes A, Rencoret G, Beltran M, Smok G, Henriquez A. Relationship between gastroesophageal reflux symptoms and 24 h esophageal pH measurements in patients with normal or minimally abnormal upper endoscopies. Rev Med Chil 2004;132:19–25.
Chan K, Liu G, Miller L, Ma C, Xu W, Schlachia CM, Darling G. Lack of correlation between a self-administered subjective GERD questionnaire and pathologic GERD diagnosed by esophageal pH monitoring. J Gastrointest Surg 2010;14:427–436.
Fisichella PM, Raz D, Palazzo F, Niponmick I, Patti MG. Clinical, radiological, and manometric profile in 145 patients with untreated achalasia. World J Surg 2008;32:1974–1979.
Streets CG, DeMeester TR. Ambulatory 24-hour pH monitoring: why, when, and what to do. J Clin Gastroenterol 2003;37:14–22.
Ott DJ. Gastroesophageal reflux. What is the role of barium studies? Am J Roentgenol 1994;162:627–629.
Chen MY, Ott DJ, Sinclair JW, Wu WC, Gelfand DW. Gastroesophageal reflux disease: correlation of esophageal pH testing and radiographic findings. Radiology 1992;185:483–486.
Johnson F, Joelsson B, Gudmundsson K, Greiff L. Symptoms and endoscopic findings in the diagnosis of gastroesophageal reflux disease. Scan J Gastroenterol 1987;22:714–718.
Richter JE. Typical and atypical presentation s of gastroesophageal reflux disease. The role of esophageal testing in diagnosis and management. Gastroenterol Clin North Am 1996;25:75–102.
Amano Y, Ishimura N, Furuta K, Okita K, Masaharu M, Azumi T, Ose T, Kshino K, Ishihara S, Adachi K, Kinoshita Y. Interobserver agreement on classifying endoscopic diagnoses of nonerosive esophagitis. Endoscopy2006;38:1032–1035.
Bytzer P, Havelund T, Moller Hansen J. Interobserver variation in the endoscopic diagnosis of reflux esophagitis. Scan J Gastroenterol 1993;28:119–125.
Patti MG, Arcerito M, Feo CV, De Pinto M, Tong J, Gantert W, Tyrrell D, Way LW. An analysis of operations for gastroesophageal reflux disease. Identifying the important technical elements. Arch Surg 1998;133:600–607.
Horvath KD, Jobe BA, Herron Dm, Swanstrom LL. Laparoscopic Toupet fundoplication is an inadequate procedure for patients with severe reflux disease. J Gastrointest Surg 1999;3:583–591.
Patti MG, Robinson T, Galvani C, Gorodner MV, Fisichella PM, Way LW. Total fundoplication is superior to partial fundoplication even when esophageal peristalsis is weak. J Am Coll Surg 2004;198:863–870.
Khajanchee YS, Hong D, Hansen PD, Swanstrom LL. Outcomes of antireflux surgery in patients with normal preoperative 24-hour pH test results. Am J Surg 2004;187:599–603.
Patti MG, Arcerito M, Tamburini A, Diener U, Feo CV, Safadi B, Fisichella P, Way LW. Effect of laparoscopic fundoplication on gastroesophageal reflux disease-induced respiratory symptoms. J Gastrointest Surg 2000;4:143–149.
Patti MG, Molena D, Fisichella PM, Perretta S, Way LW. Gastroesophageal reflux disease and chest pain. Results of laparoscopic antireflux surgery. Surg Endosc 2002;16:563–566.
Roman S, Pandolfino JE, Woodland P, Sifrim D. Testing for gastroesophageal reflux in the 21st century. Ann N Y Acad Sci 2011;1232:358–364.
Mainie I, Tutuian R, Agrawal A, Adams D, Castell DO. Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication. Br J Surg 2006;93:1483–1487.
Hirano I, Richter JE, and the Practice Parameters Committee of the American College of Gastroenterology. ACG practice guidelines: esophageal reflux testing. Am J Gastroenterol 2007;102:668–685.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. Steven Bowers (Jacksonville, FL): Dr. Patti was the primary author of a similar but substantially larger study published over 10 years ago. This very important prior work established the diagnostic inaccuracy of reflux symptoms and highlighted the finding of erosive esophagitis in approximately 10 % of the patients with normal esophageal acid exposure.
Question 1: This study is somewhat a reiteration of Dr. Patti’s prior work. How does this work improve upon the senior author’s previously published work?
Question 2: With the availability of multichannel esophageal impedance and 48-h esophageal pH testing, is 24-h pH testing still the diagnostic gold standard?
Question 3: If erosive esophagitis is not caused by reflux of gastroduodenal contents, what do the authors suspect in the etiology of the erosive disease in patients negative to 24-h pH testing?
Question 4: Did the authors perform Nissen fundoplication in all GERD-positive patients, and do they discount the finding of hypoperistalsis or spastic motor disorder on high-resolution motility in patients with GERD diagnosis?
Question 5: Do the authors consider laryngopharyngeal reflux (LPR) as an entity separate from GERD, as it does not appear that any LPR patients were included in analysis?
Closing Discussant
Dr. Brian L. Bello:
1. Patients in the previous study were referred to our Esophageal Center to complete their work-up and to confirm a diagnosis of GERD that had been based on symptoms and endoscopy. The current study consists of patients who were referred for antireflux surgery with a presumed diagnosis of GERD. The implications are different, as we have now shown that symptoms, endoscopy, and a barium swallow are not sufficient as preoperative work-up before antireflux surgery and that pH monitoring should always be performed as it helps avoiding unnecessary surgery.
2. Yes, we feel that in most patients, the 24-h ambulatory pH monitoring test is still the gold standard. In selected patients, both impedance pH testing and a 48-h test have a role.
3. We did not distinguish between erosive and nonerosive esophagitis in our study. Many patients were referred from outside of University of Chicago and had endoscopy reports not making that distinction.
4. We also use manometry to help guide the type of fundoplication. For example, we will perform a partial fundoplication if there is documented aperistalsis. We do favor a Dor fundoplication over a Toupet fundoplication as it is an easier operation to perform with no need for a posterior dissection.
5. We did not separate this group apart for analysis.
Rights and permissions
About this article
Cite this article
Bello, B., Zoccali, M., Gullo, R. et al. Gastroesophageal Reflux Disease and Antireflux Surgery—What Is the Proper Preoperative Work-up?. J Gastrointest Surg 17, 14–20 (2013). https://doi.org/10.1007/s11605-012-2057-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-012-2057-5