Abstract
Background
Laryngopharyngeal reflux (LPR) can cause atypical symptoms, asthma, and pulmonary fibrosis. The aim of this study was to establish the normative data for LPR using hypopharyngeal multichannel intraluminal impedance-pH (HMII).
Methods
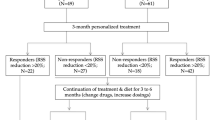
Asymptomatic subjects underwent endoscopy followed by 24-h HMII using a specialized impedance catheter configured to detect LPR before and after a 2-week course of proton pump inhibitors (PPI). Subjects were excluded if they had esophageal pathology or a positive DeMeester score. A cohort of 24 LPR patients who had a complete response to treatment was used for comparison with the normative data.
Results
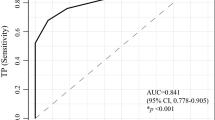
Forty subjects were enrolled. Thirty-four subjects completed one, and 25 completed both HMII testing periods off and on PPI. There was no difference in the total number of reflux events between off and on PPI [22 (8–32) and 24 (10–28), respectively, p = 0.89]. The 95th percentiles of LPR off and on PPI were 0 and 1, respectively. All patients with treatment responsive LPR had pre-treatment HMII values of LPR greater than the 95th percentile.
Conclusion
LPR events are rare in an asymptomatic population. One or more LPR events should be considered abnormal in patients with LPR symptoms regardless of whether there is a positive DeMeester score.




Similar content being viewed by others
References
Koufman JA. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. Apr 1991;101(4 Pt 2 Suppl 53):1–78.
Lang IM, Haworth ST, Medda BK, Roerig DL, Forster HV, Shaker R. Airway responses to esophageal acidification. Am J Physiol Regul Integr Comp Physiol. Jan 2008;294(1):R211–219.
Barry DW, Vaezi MF. Laryngopharyngeal reflux: More questions than answers. Cleve Clin J Med. May 2010;77(5):327–334.
Vaezi MF, Qadeer MA, Lopez R, Colabianchi N. Laryngeal cancer and gastroesophageal reflux disease: a case–control study. Am J Med. Sep 2006;119(9):768–776.
Carrau RL, Khidr A, Crawley JA, Hillson EM, Davis JK, Pashos CL. The impact of laryngopharyngeal reflux on patient-reported quality of life. Laryngoscope. Apr 2004;114(4):670–674.
Book DT, Rhee JS, Toohill RJ, Smith TL. Perspectives in laryngopharyngeal reflux: an international survey. Laryngoscope. Aug 2002;112(8 Pt 1):1399–1406.
Hicks DM, Ours TM, Abelson TI, Vaezi MF, Richter JE. The prevalence of hypopharynx findings associated with gastroesophageal reflux in normal volunteers. J Voice. Dec 2002;16(4):564–579.
Koufman JA, Aviv JE, Casiano RR, Shaw GY. Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg. Jul 2002;127(1):32–35.
Lee BE, Kim GH, Ryu DY, et al. Combined Dual Channel Impedance/pH-metry in Patients With Suspected Laryngopharyngeal Reflux. J Neurogastroenterol Motil. Apr 2010;16(2):157–165.
Hirano I, Richter JE. ACG practice guidelines: esophageal reflux testing. Am J Gastroenterol. Mar 2007;102(3):668–685.
Vela MF. Non-acid reflux: detection by multichannel intraluminal impedance and pH, clinical significance and management. Am J Gastroenterol. Feb 2009;104(2):277–280.
Agrawal A, Castell DO. Clinical importance of impedance measurements. J Clin Gastroenterol. May–Jun 2008;42(5):579–583.
Velanovich V. The development of the GERD-HRQL symptom severity instrument. Dis Esophagus. 2007;20(2):130–134.
Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI). J Voice. Jun 2002;16(2):274–277.
Hatlebakk JG, Katz PO, Camacho-Lobato L, Castell DO. Proton pump inhibitors: better acid suppression when taken before a meal than without a meal. Aliment Pharmacol Ther. Oct 2000;14(10):1267–1272.
Hill LD, Kozarek RA, Kraemer SJ, et al. The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointest Endosc. Nov 1996;44(5):541–547.
Johnson LF, DeMeester TR. Development of the 24-hour intraesophageal pH monitoring composite scoring system. J Clin Gastroenterol. 1986;8 Suppl 1:52–58.
Koufman JA, Amin MR, Panetti M. Prevalence of reflux in 113 consecutive patients with laryngeal and voice disorders. Otolaryngol Head Neck Surg. Oct 2000;123(4):385–388.
Ford CN. Evaluation and management of laryngopharyngeal reflux. Jama. Sep 28 2005;294(12):1534–1540.
Fass R, Noelck N, Willis MR, et al. The effect of esomeprazole 20 mg twice daily on acoustic and perception parameters of the voice in laryngopharyngeal reflux. Neurogastroenterol Motil. Feb 2010;22(2):134–141, e144–135.
Vaezi MF, Richter JE, Stasney CR, et al. Treatment of chronic posterior laryngitis with esomeprazole. Laryngoscope. Feb 2006;116(2):254–260.
Gatta L, Vaira D, Sorrenti G, Zucchini S, Sama C, Vakil N. Meta-analysis: the efficacy of proton pump inhibitors for laryngeal symptoms attributed to gastro-oesophageal reflux disease. Aliment Pharmacol Ther. Feb 15 2007;25(4):385–392.
Qadeer MA, Phillips CO, Lopez AR, et al. Proton pump inhibitor therapy for suspected GERD-related chronic laryngitis: a meta-analysis of randomized controlled trials. Am J Gastroenterol. Nov 2006;101(11):2646–2654.
Mainie I, Tutuian R, Agrawal A, Adams D, Castell DO. Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication. Br J Surg. Dec 2006;93(12):1483–1487.
So JB, Zeitels SM, Rattner DW. Outcomes of atypical symptoms attributed to gastroesophageal reflux treated by laparoscopic fundoplication. Surgery. Jul 1998;124(1):28–32.
Swoger J, Ponsky J, Hicks DM, et al. Surgical fundoplication in laryngopharyngeal reflux unresponsive to aggressive acid suppression: a controlled study. Clin Gastroenterol Hepatol. Apr 2006;4(4):433–441.
Westcott CJ, Hopkins MB, Bach K, Postma GN, Belafsky PC, Koufman JA. Fundoplication for laryngopharyngeal reflux disease. J Am Coll Surg. Jul 2004;199(1):23–30.
Lindstrom DR, Wallace J, Loehrl TA, Merati AL, Toohill RJ. Nissen fundoplication surgery for extraesophageal manifestations of gastroesophageal reflux (EER). Laryngoscope. Oct 2002;112(10):1762–1765.
Anandasabapathy S, Jaffin BW. Multichannel intraluminal impedance in the evaluation of patients with persistent globus on proton pump inhibitor therapy. Ann Otol Rhinol Laryngol. Aug 2006;115(8):563–570.
Wu JC. Combined Multichannel Intraluminal Impedance and pH Monitoring for Patients With Suspected Laryngopharyngeal Reflux: Is It Ready to Use? J Neurogastroenterol Motil. Apr 2010;16(2):108–109.
Oelschlager BK, Quiroga E, Isch JA, Cuenca-Abente F. Gastroesophageal and pharyngeal reflux detection using impedance and 24-hour pH monitoring in asymptomatic subjects: defining the normal environment. J Gastrointest Surg. Jan 2006;10(1):54–62.
Shay S, Tutuian R, Sifrim D, et al. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol. Jun 2004;99(6):1037–1043.
Xiao YL, Lin JK, Cheung TK, et al. Normal values of 24-hour combined esophageal multichannel intraluminal impedance and pH monitoring in the Chinese population. Digestion. 2009;79(2):109–114.
Zentilin P, Iiritano E, Dulbecco P, et al. Normal values of 24-h ambulatory intraluminal impedance combined with pH-metry in subjects eating a Mediterranean diet. Dig Liver Dis. Apr 2006;38(4):226–232.
Zerbib F, des Varannes SB, Roman S, et al. Normal values and day-to-day variability of 24-h ambulatory oesophageal impedance-pH monitoring in a Belgian–French cohort of healthy subjects. Aliment Pharmacol Ther. Nov 15 2005;22(10):1011–1021.
Sun G, Muddana S, Slaughter JC, et al. A new pH catheter for laryngopharyngeal reflux: Normal values. Laryngoscope. Aug 2009;119(8):1639–1643.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. John F. Sweeney (Atlanta, GA): Good morning and Happy Mother’s Day. My name is John Sweeney and I am Chief of General and Gastrointestinal Surgery at Emory University in Atlanta. I would like to take the opportunity to thank the Society for the opportunity to discuss this manuscript. Before I begin, I would like to congratulate Dr. Hoppo on a fine presentation. In addition I would like to thank the authors for providing me a copy of their manuscript for review well in advance of the meeting. It is clearly and concisely written. I have three questions:
1. The manuscript states that healthy subjects were recruited through community advertising. How did you incentivize their participation? Were they paid? If so, when did this occur? After each completed test? At the end of the entire experiment? What happened if they completed the tests but the data were not felt to be usable? Were they still paid?
2. The next question is regarding the LPR treatment responsive group. The manuscript states that subjects were selected from a group of patients with atypical symptoms of LPR that had a complete response to medical or surgical therapy. Were there any differences in impedance results for each subgroup of patients?
3. As you clearly state in the discussion of your manuscript, the outcomes for either medical or surgical management of LPR can vary significantly. How will the results of this study lead to better stratification of patients with LPR to the modality that they are most likely to respond? More importantly, do you envision that this modality will help us identify patients that will not respond to a fundoplication and therefore in whom surgery should therefore be avoided?
Again, I would like to thank the Society for the privilege of discussing this paper and congratulate the authors on a well-designed and well-executed study.
Closing Discussant
Dr. Toshitaka Hoppo: Thank you very much for your great comments and questions, Dr. Sweeney.
1. The first question was regarding incentive for participants. All participants were paid twice after each impedance testing. They were paid $125 after the placement of the first impedance catheter and $75 after the placement of the second impedance catheter. They were still paid if the data were not usable.
2. The second question was regarding difference in LPR events in patients who responded to medical therapy and surgical therapy. When looked at the difference in the number of LPR events on impedance testing, there was a trend towards more LPR events observed in surgical therapy responsive patients compared to medical therapy responsive patients (3 vs. 1.2/day). This may be explained by that more LPR events cannot be controlled well by medical therapy.
3. The last question was regarding the stratification with impedance testing. This is a good question. It is important to determine who would benefit from the treatment and what treatment would be the best. The impedance testing can make a diagnosis of LPR but cannot tell us what the best treatment would be for each patient. However, making an accurate diagnosis of LPR should contribute to the better outcomes of treatments.
Rights and permissions
About this article
Cite this article
Hoppo, T., Sanz, A.F., Nason, K.S. et al. How Much Pharyngeal Exposure Is “Normal”? Normative Data for Laryngopharyngeal Reflux Events Using Hypopharyngeal Multichannel Intraluminal Impedance (HMII). J Gastrointest Surg 16, 16–25 (2012). https://doi.org/10.1007/s11605-011-1741-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1741-1