Abstract
Purpose
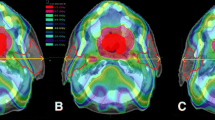
Whole-brain radiotherapy is performed as standard therapy in patients with multiple brain metastases and in patients with more favourable prognosis such as lymphoma and small-cell lung carcinoma in the prophylactic setting. Because of the prognosis and the total prescribed dose, the parotid glands are not usually regarded as an organ at risk in whole-brain radiotherapy. Long-term survival can be expected in some of these patients and late toxicity can be observed, becoming essential to evaluate organs at risk, particularly the parotid glands even in metastatic patients. We compared the 2D with 3D technique to evaluate parotid glands involvement and received dose, and coverage of the clinical target volume.
Materials and methods
Seven patients were considered. The prescribed dose was 30 Gy in ten fractions. On the same day and with the same set-up, all the treatment planning were performed using a 2D and 3D technique. A treatment plan was performed following same technical characteristics as the 2D technique. The parotid glands and whole brain were delineated. Dose–volume statistics were analysed.
Results
Dose–volume histograms of the parotid glands showed that 2/7 patients (28 %) received a mean dose >20 Gy. We found a lack of coverage of the clinical target volume in 6/7 patients.
Conclusions
Planning whole-brain radiotherapy with only the 2D technique involves a risk of including parotid glands in the field and not covering the clinical target volume. The 3D technique should be systematically performed and the parotid glands should be regarded as an organ at risk in whole-brain radiotherapy.



Similar content being viewed by others
References
Aupérin A, Arriagada R, Pignon JP et al (1999) Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. N Engl J Med 341:476–484
Slotman B, Faivre-Finn C, Kramer G et al (2007) EORTC radiation oncology group and lung cancer group. Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med 357:664–672
Coia LR (1992) The role of radiation therapy in the treatment of brain metastases. Int J Radiat Oncol Biol Phys 23:229–238
Gaspar LE, Mehta MP, Patchell RA et al (2010) The role of whole brain radiation therapy in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neuro-Oncol 96:17–32
Golden DW, Lamborn KR, McDermott MW et al (2008) Prognostic factors and grading systems for overall survival in patients treated with radiosurgery for brain metastases: variation by primary site. J Neurosurg 109(Suppl):77–86
Tsao MN, Lloyd N, Wong R et al (2006) Whole brain radiotherapy for the treatment of multiple brain metastases. Cochrane Database Syst Rev 3:CD003869
Shibamoto Y, Ogino H, Hasegawa M et al (2005) Results of radiation monotherapy for primary central nervous system lymphoma in the 1990s. Int J Radiat Oncol Biol Phys 62:809–813
Doucet S, Kumthekar P, Raizer J (2013) Primary central nervous system lymphoma. Curr Treat Options Oncol 14:185–197
Buglione M, Bandera L, Grisanti S et al (2012) The impact of tumour histology and recursive partitioning analysis classification on the prognosis of patients treated with whole-brain hypofractionated radiotherapy for brain metastases: analysis of 382 patients. Radiol Med 117:133–147
(2010) International commission on radiation units and measurements. ICRU Report 83. J ICRU 10:1
Deasy JO, Moiseenko V, Marks L et al (2010) Radiotherapy dose-volume effects on salivary gland function. Int J Radiat Oncol Biol Phys 76:S58–S63
Khanfir A, Lahiani F, Bouzguenda R et al (2013) Prognostic factors and survival in metastatic breast cancer: a single institution experience. Rep Pract Oncol Radiother 14:127–132
Noh OK, Chun M, Nam SS et al (2011) Parotid gland as a risk organ in whole brain radiotherapy. Radiother Oncol 98:223–226
Roesink JM, Terhaard CH, Moerland MA et al (2000) CT-based parotid gland location: implications for preservation of parotid function. Radiother Oncol 55:131–133
Deasy JO, Moiseenko V, Marks L et al (2010) Radiotherapy dose–volume effects on salivary gland function. Int J Radiat Oncol Biol Phys 76:S58–S63
Eisbruch A, Haken RKT, Kim HM et al (1999) Dose, volume and function relationship in parotid salivary glands following conformal and intensity modulated irradiation of head and neck cancer. Int J Radiat Oncol Biol Phys 45:577–587
Fiorentino A, Chiumento C, Caivano R et al (2012) Whole brain radiotherapy: are parotid glands organs at risk? Radiother Oncol 103:130–131
Loos G, Paulon R, Verrelle P, Lapeyre M (2012) Whole brain radiotherapy for brain metastases: the technique of irradiation influences the dose to parotid glands. Cancer Radiother 16:136–139
Mendenhall WM, Mancuso AA (2009) Radiotherapy for head and neck cancer–is the “next level” down? Int J Radiat Oncol Biol Phys 73:645–646
Nutting CM, Morden JP, Harrington KJ, Urbano TG, Bhide SA, Clark C, Miles EA, Miah AB, Newbold K, Tanay M, Adab F, Jefferies SJ, Scrase C, Yap BK, A’Hern RP, Sydenham MA, Emson M, Hall E, PARSPORT trial management group (2011) Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial. Lancet Oncol 12:127–136
Lambrecht M, Nevens D, Nuyts S (2013) Intensity-modulated radiotherapy vs. parotid-sparing 3D conformal radiotherapy. Effect on outcome and toxicity in locally advanced head and neck cancer. Strahlenther Onkol 189:223–229
Conflict of interest
Marianna Trignani, Domenico Genovesi, Annamaria Vinciguerra, Angelo Di Pilla, Antonietta Augurio, Monica Di Tommaso, Giampiero Ausili Cèfaro, Marta Di Nicola declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trignani, M., Genovesi, D., Vinciguerra, A. et al. Parotid glands in whole-brain radiotherapy: 2D versus 3D technique for no sparing or sparing. Radiol med 120, 324–328 (2015). https://doi.org/10.1007/s11547-014-0436-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-014-0436-6