Abstract
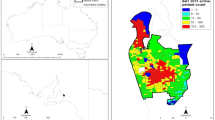
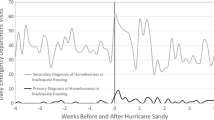
Urban contexts introduce unique challenges that must be addressed to ensure that areas of high population density can function when disasters occur. The ability to generate useful data to guide decision-making is critical in this context. Widespread adoption of electronic health record (EHR) systems in recent years has created electronic data sources and networks that may play an important role in public health surveillance efforts, including in post-disaster situations. The Primary Care Information Project (PCIP) at the New York City Department of Health and Mental Hygiene has partnered with local clinicians to establish an electronic data system, and this network provides infrastructure to support primary care surveillance activities in New York City. After Hurricane Sandy, PCIP generated several sets of data to contribute to the city’s efforts to assess the impact of the storm, including daily connectivity data to establish practice operations, data to examine patterns of primary care utilization in severely affected and less affected areas, and data on the frequency of respiratory infection diagnosis in the primary care setting. Daily patient visit data from three heavily affected neighborhoods showed the health department where primary care capacity was most affected in the weeks following Sandy. Overall transmission data showed that practices in less affected areas were quicker to return to normal reporting patterns, while those in more affected areas did not resume normal data transmissions for a few months. Rates of bronchitis increased after Sandy compared to the two prior years; while this was most likely attributable to a more severe flu season, it demonstrates the capacity of primary care networks to pick up on these types of post-emergency trends. Hurricane Sandy was the first disaster situation where PCIP was asked to assess public health impact, generating information that could contribute to aid and recovery efforts. This experience allowed us to explore the strengths and weaknesses of ambulatory EHR data in post-disaster settings. Data from ambulatory EHR networks can augment existing surveillance streams by providing sentinel population snapshots on clinically available indicators in near real time.


Similar content being viewed by others
References
USAID Cred Crunch Issue No 31: disaster data: a balanced perspective. http://cred01.epid.ucl.ac.be/f/CredCrunch31.pdf. Accessed May 9, 2013.
US Environmental Protection Agency. Future climate change. http://www.epa.gov/climatechange/science/future.html#Precipitation. Accessed June 22, 2013.
Institute of Medicine and the New York Academy of Medicine. Identifying disaster medical and public health research priorities: data needs arising in response to Hurricane Sandy. http://www.nyam.org/news/docs/pdf/NYAM-Disaster-Research-Priorities-Meeting-Summary.pdf. Accessed May 20, 2013.
Lister SA. Public health and medical emergency management: issues in the 112th Congress report. http://www.fas.org/sgp/crs/misc/R41646.pdf. Published February 18, 2011. Accessed May 9, 2013.
Norris FH. Disasters in urban context. J Urban Health. 2002; 79(3): 308–314.
Cochrane D, Allegra J, Rothman J. Real-time biosurveillance using an existing emergency department electronic medical record database. J Urban Health. 2003; 80(Suppl 1): i120–i121.
Hsiao CJ, Hing E. Use and Characteristics of Electronic Health Record Systems Among Office-based Physician Practices: United States, 2001–2012. Atlanta: CDC; 2010; http://www.cdc.gov/nchs/data/databriefs/db111.htm. Accessed October 12, 2013.
Lombardo J, Burkom H, Elbert E, et al. A systems overview of the Electronic Surveillance System for the Early Notification of Community-Based Epidemics (ESSENCE II). J Urban Health. 2003; 80(2 Suppl 1): i32–i42.
Townes JM, Kohn MA, Southwick KL, et al. Investigation of an electronic emergency department information system as a data source for respiratory syndrome surveillance. J Public Health Manag Pract. 2004; 10(4): 299–307.
Redwood-Campbell L, Abrahams J. Primary health care and disasters—the current state of the literature: what we know, gaps and next steps. Prehosp Disaster Med. 2011; 26(3): 184–191.
Centers for Disease Control and Prevention. Ambulatory care use and physician visits. http://www.cdc.gov/nchs/fastats/docvisit.htm. Published 2010. Accessed June 28, 2013.
Lurio J, Morrison FP, Pichardo M, Berg R, Buck MD, Wu W, et al. Using electronic health record alerts to provide public health situational awareness to clinicians. J Am Med Inform Assoc. 2010; 17(2): 217–219.
Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood). 2010; 29(5): 799–805.
Carrier E, Yee T, Cross D, Samuel D. HSC Research Brief No. 24: emergency preparedness and community coalitions: opportunities and challenges. Center for Studying Health System Change. http://www.hschange.com/CONTENT/1323/. Accessed March 4, 2014.
Mostashari F, Tripathi M, Kendall M. A tale of two large community electronic health record extension projects. Health Aff (Millwood). 2009; 28(2): 345–356.
HealthIT.gov. Regional Extension Centers. http://www.healthit.gov/providers-professionals/regional-extension-centers-recs. Accessed March 3, 2014.
Buck MD, Anane S, Taverna J, Amirfar S, Stubbs-Dame R, Singer J. The Hub Population Health System: distributed ad hoc queries and alerts. J Am Med Inform Assoc. 2012; 19(e1): e46–e50.
Newton-Dame R, Greene C, Thorpe L, et al. From clinical practice to population monitoring: harnessing EHR data for public health in New York City. Paper presented at: the Electronic Data Methods Forum 2013 Annual Symposium; June 22, 2013; Baltimore, Maryland, USA.
Centers for Disease Control and Prevention. Influenza Activity—United States, 2012–13 Season and Composition of the 2013–14 Influenza Vaccine. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6223a5.htm?s_cid=mm6223a5_e. Published 2013. Accessed October 28, 2013.
Plagianos MG, Wu WY, McCullough C, Paladini M, Lurio J, Buck MD, et al. Syndromic surveillance during pandemic (H1N1) 2009 outbreak, New York, New York. USA Emerg Infect Dis. 2011; 17(9): 1724–1726.
Hoffman S, Podgurski A. Big bad data: law, public health, and biomedical databases. J Law Med Ethics. 2013; 41(Suppl 1): 56–60.
Gregory K, Santora M. Bloomberg outlines $20 billion storm protection plan. The New York Times. June 11, 2013. http://www.nytimes.com/2013/06/12/nyregion/bloomberg-outlines-20-billion-plan-to-protect-city-from-future-storms.html?pagewanted=all&_r=0. Accessed June 23, 2013.
Acknowledgments
We would like to acknowledge Dr. Winfred Wu for his thoughtful input on this manuscript, Dr. Sam Amirfar for his assistance in determining relevant RID diagnoses, Xiaoliang Wang for her assistance with the RID data, and Aurora Amoah for summarizing Rockaways care-seeking data. We also wish to acknowledge our colleagues in the Bureau of Primary Care Access and Planning for their work in tracking the operational status of primary care facilities in areas significantly affected by Sandy and their communications with the Mayor’s office. This study is partially supported through a Centers for Disease Control and Prevention Community Transformation Grant (no. 5U58DP003689-02).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sebek, K., Jacobson, L., Wang, J. et al. Assessing Capacity and Disease Burden in a Virtual Network of New York City Primary Care Providers Following Hurricane Sandy. J Urban Health 91, 615–622 (2014). https://doi.org/10.1007/s11524-014-9874-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-014-9874-7