Abstract
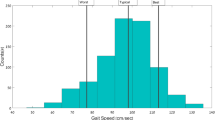
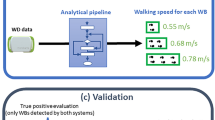
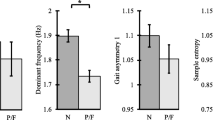
Morbidity and falls are problematic for older people. Wearable devices are increasingly used to monitor daily activities. However, sensors often require rigid attachment to specific locations and shuffling or quiet standing may be confused with walking. Furthermore, it is unclear whether clinical gait assessments are correlated with how older people usually walk during daily life. Wavelet transformations of accelerometer and barometer data from a pendant device worn inside or outside clothing were used to identify walking (excluding shuffling or standing) by 51 older people (83 ± 4 years) during 25 min of ‘free-living’ activities. Accuracy was validated against annotated video. Training and testing were separated. Activities were only loosely structured including noisy data preceding pendant wearing. An electronic walkway was used for laboratory comparisons. Walking was classified (accuracy ≥97 %) with low false-positive errors (≤1.9 %, κ ≥ 0.90). Median free-living cadence was lower than laboratory-assessed cadence (101 vs. 110 steps/min, p < 0.001) but correlated (r = 0.69). Free-living step time variability was significantly higher and uncorrelated with laboratory-assessed variability unless detrended. Remote gait impairment monitoring using wearable devices is feasible providing new ways to investigate morbidity and falls risk. Laboratory-assessed gait performances are correlated with free-living walks, but likely reflect the individual’s ‘best’ performance.





Similar content being viewed by others
References
Aminian K, Robert P, Buchser EE, Rutschmann B, Hayoz D, Depairon M (1999) Physical activity monitoring based on accelerometry: validation and comparison with video observation. Med Biol Eng Comput 37(3):304–308
Ayrulu-Erdem B, Barshan B (2011) Leg motion classification with artificial neural networks using wavelet-based features of gyroscope signals. Sensors (Basel, Switzerland) 11(2):1721–1743. doi:10.3390/s110201721
Balasundaram K, Masse S, Nair K, Umapathy K (2013) A classification scheme for ventricular arrhythmias using wavelets analysis. Med Biol Eng Comput 51(1–2):153–164. doi:10.1007/s11517-012-0980-y
Barralon P, Vuillerme N, Noury N (2006) Walk detection with a kinematic sensor: frequency and wavelet comparison. Conf Proc Ann Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Conf 1:1711–1714. doi:10.1109/iembs.2006.260770
Brodie MA, Beijer TR, Canning CG, Lord SR (2015) Head and pelvis stride-to-stride oscillations in gait: validation and interpretation of measurements from wearable accelerometers. Physiol Meas 36(5):857–872. doi:10.1088/0967-3334/36/5/857
Brodie MA, Lord SR, Coopens MJ, Annegarn J, Delbaere K (2015) Eight weeks of remote monitoring using a freely worn device reveals unstable gait patterns in older fallers. Aheadofprint, IEEE Trans Bio-med Eng. doi:10.1109/TBME.2015.2433935
Brodie MA, Lovell NH, Redmond SJ, Lord SR (2015) Bottom-up subspace clustering suggests a paradigm shift to prevent fall injuries. Med Hypotheses 84(4):356–362. doi:10.1016/j.mehy.2015.01.017
Brodie MA, Menz HB, Lord SR (2014) Age-associated changes in head jerk while walking reveal altered dynamic stability in older people. Exp Brain Res 232(1):51–60. doi:10.1007/s00221-013-3719-6
Del Rosario MB, Wang K, Wang J, Liu Y, Brodie M, Delbaere K, Lovell NH, Lord SR, Redmond SJ (2014) A comparison of activity classification in younger and older cohorts using a smartphone. Physiol Meas 35(11):2269
Delbaere K, Sherrington C, Lord SR (2013) Chapter 70—falls prevention interventions. In: Marcus R, Feldman D, Dempster DW, Luckey M, Cauley JA (eds) Osteoporosis (4th edn). Academic Press, San Diego, pp 1649–1666. doi:10.1016/B978-0-12-415853-5.00070-4
Dijkstra B, Kamsma Y, Zijlstra W (2010) Detection of gait and postures using a miniaturised triaxial accelerometer-based system: accuracy in community-dwelling older adults. Age Ageing 39(2):259–262. doi:10.1093/ageing/afp249
Godfrey A, Bourke AK, Olaighin GM, van de Ven P, Nelson J (2011) Activity classification using a single chest mounted tri-axial accelerometer. Med Eng Phys 33(9):1127–1135. doi:10.1016/j.medengphy.2011.05.002
Godfrey A, Conway R, Meagher D, OL G (2008) Direct measurement of human movement by accelerometry. Med Eng Phys 30(10):1364–1386. doi:10.1016/j.medengphy.2008.09.005
Haggard P, Cockburn J, Cock J, Fordham C, Wade D (2000) Interference between gait and cognitive tasks in a rehabilitating neurological population. J Neurol Neurosurg Psychiatry 69(4):479–486
Karel JM, Senden R, Janssen JE, Savelberg HM, Grimm B, Heyligers IC, Peeters R, Meijer K (2010) Towards unobtrusive in vivo monitoring of patients prone to falling. Conf Proc Ann Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Conf 2010:5018–5021. doi:10.1109/iembs.2010.5626232
Kaymak U, Ben-David A, Potharst R (2012) The AUK: a simple alternative to the AUC. Eng Appl Artif Intell. doi:10.1016/j.engappai.2012.02.012
Khan AM, Lee YK, Lee S, Kim TS (2010) Accelerometer’s position independent physical activity recognition system for long-term activity monitoring in the elderly. Med Biol Eng Comput 48(12):1271–1279. doi:10.1007/s11517-010-0701-3
Kirtley C (2006) Clinical gait analysis. Elsevier, London
Kressig RW, Beauchet O (2006) Guidelines for clinical applications of spatio-temporal gait analysis in older adults. Aging Clin Exp Res 18(2):174–176
Lord SR, Menz HB, Tiedemann A (2003) A physiological profile approach to falls risk assessment and prevention. Phys Ther 83(3):237–252
Mannini A et al (2011) Healthcare and accelerometry: applications for activity monitoring, recognition, and functional assessment. In: Lai DTH, Palaniswami M, Begg R (eds) Healthcare sensor networks: challenges toward practical implementation. CRC Press, New York, pp 21–46
Mathie MJ, Celler BG, Lovell NH, Coster AC (2004) Classification of basic daily movements using a triaxial accelerometer. Med Biol Eng Comput 42(5):679–687
Moe-Nilssen R (1998) A new method for evaluating motor control in gait under real-life environmental conditions. Part 2: gait analysis. Clin Biomech 13(4–5):328–335
Montero-Odasso M, Verghese J, Beauchet O, Hausdorff JM (2012) Gait and cognition: a complementary approach to understanding brain function and the risk of falling. J Am Geriatr Soc 60(11):2127–2136. doi:10.1111/j.1532-5415.2012.04209.x
Najafi B, Aminian K, Paraschiv-Ionescu A, Loew F, Bula CJ, Robert P (2003) Ambulatory system for human motion analysis using a kinematic sensor: monitoring of daily physical activity in the elderly. IEEE Trans Bio Med Eng 50(6):711–723. doi:10.1109/TBME.2003.812189
Rispens SM, van Schooten KS, Pijnappels M, Daffertshofer A, Beek PJ, van Dieen JH (2015) Identification of fall risk predictors in daily life measurements: gait characteristics’ reliability and association with self-reported fall history. Neurorehabilitation Neural Repair 29(1):54–61. doi:10.1177/1545968314532031
Runyi Y (2012) Shift-variance analysis of generalized sampling processes. IEEE Trans Signal Process 60(6):2840–2850. doi:10.1109/tsp.2012.2190062
Sachdev PS, Brodaty H, Reppermund S, Kochan NA, Trollor JN, Draper B, Slavin MJ, Crawford J, Kang K, Broe GA, Mather KA, Lux O, Memory, Ageing Study T (2010) The Sydney memory and ageing study (MAS): methodology and baseline medical and neuropsychiatric characteristics of an elderly epidemiological non-demented cohort of Australians aged 70–90 years. Int Psychogeriatr 22(8):1248–1264. doi:10.1017/S1041610210001067
Sekine M, Tamura T, Akay M, Fujimoto T, Togawa T, Fukui Y (2002) Discrimination of walking patterns using wavelet-based fractal analysis. IEEE Trans Neural Syst Rehabil Eng Publ IEEE Eng Med Biol Soc 10(3):188–196. doi:10.1109/tnsre.2002.802879
Senden R, Grimm B, Heyligers IC, Savelberg HH, Meijer K (2009) Acceleration-based gait test for healthy subjects: reliability and reference data. Gait Posture 30(2):192–196. doi:10.1016/j.gaitpost.2009.04.008
Serbes G, Aydin N (2014) Denoising performance of modified dual-tree complex wavelet transform for processing quadrature embolic Doppler signals. Med Biol Eng Comput 52(1):29–43. doi:10.1007/s11517-013-1114-x
Sims J (2012) Advancing physical activity in older Australians: missed opportunities? Australas J Ageing 31(4):206–207. doi:10.1111/ajag.12002
Tolkiehn M, Atallah L, Lo B, Yang GZ (2011) Direction sensitive fall detection using a triaxial accelerometer and a barometric pressure sensor. Conf Proc Ann Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Conf 2011:369–372. doi:10.1109/IEMBS.2011.6090120
Wang K, Lovell NH, Del Rosario MB, Ying L, Jingjing W, Narayanan MR, Brodie MAD, Delbaere K, Menant J, Lord SR, Redmond SJ (2014) Inertial measurements of free-living activities: assessing mobility to predict falls. In: Engineering in medicine and biology society (EMBC), 36th annual international conference of the IEEE, 26–30 Aug 2014, pp 6892–6895. doi:10.1109/embc.2014.6945212
Yang S, Laudanski A, Li Q (2012) Inertial sensors in estimating walking speed and inclination: an evaluation of sensor error models. Med Biol Eng Comput 50(4):383–393. doi:10.1007/s11517-012-0887-7
Zijlstra W, Aminian K (2007) Mobility assessment in older people: new possibilities and challenges. Eur J Ageing 4(1):3–12. doi:10.1007/s10433-007-0041-9
Acknowledgments
We gratefully acknowledge support which made this research possible. Devices were lent from Philips Research Europe, Netherlands. M.B., S.L., and K.D. were NHMRC Fellows, Australia. Y.G. was supported by the Margarete and Walter Lichtenstein Foundation, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brodie, M.A.D., Coppens, M.J.M., Lord, S.R. et al. Wearable pendant device monitoring using new wavelet-based methods shows daily life and laboratory gaits are different. Med Biol Eng Comput 54, 663–674 (2016). https://doi.org/10.1007/s11517-015-1357-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-015-1357-9