Abstract
Hand, foot and mouth disease (HFMD) is a significant health concern in the Asia–Pacific regions for infants and young children in recent years. However, no vaccines or therapeutics are available at present. The causative agents for HFMD include human enterovirus 71 (EV71), coxsackievirus A16 (CVA16) and some other viruses. Recently, tremendous progress has been made in the development of monovalent and bivalent vaccines against HFMD. A few neutralizing monoclonal antibodies against EV71 or CVA16 have been identified and characterized. Here, we reviewed some achievements for the development of broadly protective vaccines and neutralizing antibodies against HFMD, and discussed challenges and prospects toward broadly protective multivalent vaccines and therapeutic antibodies against HFMD.
Similar content being viewed by others
1 Introduction
Hand, foot and mouth disease (HFMD) is a worldwide infectious disease in infants and young children. In recent years, numerous outbreaks of HFMD occurred in the Asia–Pacific regions, causing significant morbidity and mortality [1]. The reported fatal cases of HFMD in the mainland of China has reached to over 3000 since 2008 (www.chinacdc.cn). It is noteworthy that the number of reported fetal cases caused by HFMD is 501 in 2014. Compared with 2013, the morbidity and mortality increased by 51.86 % and 98.92 %, respectively. However, no vaccines or therapeutics are available at present.
HFMD is commonly a mild disease, but it can be associated with severe neurological symptoms, such as acute fatal encephalitis, polio-like acute flaccid paralysis and neurogenic pulmonary edema [2]. The major causative agents for HFMD are human enterovirus 71 (EV71) and coxsackievirus A16 (CVA16), both belonging to species Enterovirus A genus Enterovirus family Picornaviridae [3]. Other enteroviruses, such as CVA6 [4], A10 [4], A12 [5] and B5 [5], echovirus30 [6], are also associated with outbreaks of HFMD. Therefore, for more effective control and prevention of HFMD, a multivalent vaccine eliciting broadly neutralizing antibodies is highly desirable.
Currently, a few vaccine candidates against EV71 have entered clinical trials [7–10], and other vaccine candidates are at the preclinical study stage. Here, we summarized major achievements in the development of vaccines and therapeutic antibodies against HFMD.
2 Vaccines
2.1 Vaccine development against EV71
EV71 is the leading causative agent for HFMD. Until now, a number of approaches have been taken to develop vaccines against EV71, including inactivated whole-virus vaccines [7–10], attenuated live virus vaccines [11], virus-like particles (VLPs) [12–17] and other types of EV71 vaccine candidates [18–27] (Table 1).
2.1.1 Inactivated EV71 vaccine
The first clinical trial of formalin-inactivated EV71 vaccine containing an aluminum hydroxide adjuvant was conducted in Bulgaria in 1975, in response to the epidemic [28]. However, the results were not reported. Recently, at least five EV71-inactivated whole-virus vaccines have entered clinical trials (Table 1). Beijing Vigoo, Sinovac and the Chinese Academy of Medical Science (CAMS) in the mainland of China have independently developed C4-subgenotype-based inactivated EV71 vaccine candidates, all of which have finished phase III clinical trials with high efficacy. Health Research Institute (NHRI) in Taiwan have completed phase I clinical trial of a B4-subgenotype-based inactivated EV71 vaccine candidate using formalin for inactivation, and the study showed more than fourfold increase in the neutralizing antibody titers against the B4 vaccine strain even after a single immunization and the presence of cross-neutralizing antibodies against subgenotypes B1, B5 and C4a, but not C2 [7]. Inviragen in Singapore initiated phase I clinical trial of a B2 subgenotype inactivated EV71 vaccine from Vero cells. However, the results are still pending.
2.1.2 Attenuated EV71 vaccine
The study on EV71-attenuated live vaccine was first reported in 2005 [11]. An infectious cDNA clone of EV71 prototype BrCr (genotype A) was constructed, and an attenuated strain was generated with mutations introduced into the DNA sequences corresponding to the 5′ untranslated region, 3D polymerase and 3′ untranslated region. This EV71 mutant showed attenuated neurovirulence, resulting in limited spread of virus in the central nervous system of monkeys. However, such attenuated live vaccine has safety concerns.
2.1.3 EV71 virus-like particle vaccine
Virus-like particles (VLPs) have long been used in vaccine development, as they resemble authentic viral capsids in structure but are not infectious due to the lack of viral genetic material. The repetitive ordered arrangement of epitopes on the capsid surface makes VLPs promising candidates as potent immunogens and vaccine products. In addition, VLPs can be produced in large quantities in different recombinant expression systems without the need of virus culture, purification and inactivation.
The use of insect cells to generate EV71 VLPs was first reported in 2003 [12]. Coexpression of P1 and 3CD of the EV71 neu strain (subgenotype C2) led to the cleavage of P1 by 3CD into VP0, VP1 and VP3 and the assembly of VLPs with morphology similar to that of the native EV71 virus particles. Later, a higher expression level of EV71 VLPs was achieved by a single recombinant baculovirus coexpressing P1 and 3CD with a yield of approximately 10 mg of VLPs per 109 Bac-P1-3CD-infected cells at a MOI = 10 [13]. Two years later, the same group reported that EV71 VLPs could elicit neutralizing antibodies in mice and protected mice against a lethal viral challenge [14]. They also found that the neutralizing antibody titers induced by VLPs were significantly higher than those elicited by the heat-inactivated EV71. In 2010, Chung et al. [29] reported insect cell-produced VLPs can reach a yield of approximately 64.4 mg/L under optimal conditions. In 2012, Lin et al. [30] first validated the immunogenicity of EV71 VLPs in macaque monkeys. This group found that the monkeys developed both specific humoral and cellular immune responses against EV71. Despite lower EV71-neutralizing antibodies found in the sera of VLP-immunized monkeys compared with monkeys vaccinated with the inactivated EV71, the VLP-based vaccine generated a memory immune response to EV71. Another observation was that VLPs of the C2 subgenotype elicited cross-reactive neutralizing antibodies against EV71 of the subgenotypes B4, B5, C4 and C5.
Furthermore, in 2013, Ku et al. [31] reported that the neutralizing anti-VLP antisera were able to efficiently inhibit virus binding to target cells, and the neutralizing antibodies were found to target mainly an extremely conserved epitope (aa 211–225) located at the GH loop of VP1.
The use of yeast to generate EV71 VLPs was reported recently. In 2013, it was first reported the generation of EV71 VLPs (subgenotype C4) from Saccharomyces cerevisiae by the coexpression of P1 and 3CD [15]. These VLPs are structurally similar to naturally occurring empty particles of EV71 (Fig. 1). The VLPs elicited robust neutralizing antibody response in mice, and in vivo challenge experiments showed that the immune sera induced by VLPs conferred protection in neonatal mice against a lethal EV71 challenge. In 2015, Zhang et al. [16] generated high levels of EV71 VLPs in Pichia pastoris by coexpressing P1 and 3CD of up to 4.9 % total soluble protein (or 150 mg VLP per liter of yeast culture). The VLPs potently induced neutralizing antibodies against homologous and heterologous EV71 strains in mice. More importantly, maternal immunization with VLPs protected neonatal mice in both intraperitoneal and oral challenge experiments. Compared to the baculovirus expression system, yeast has certain advantages making them ideal for EV71 VLP production, including high potential yield, low cost, high scalability and ease of manipulation.
EV71 VLP structure. Capsid proteins VP1, VP0, VP3 and the neutralization epitope SP70 (residues 208–222 in VP1) are colored in magenta, yellow, cyan and blue, respectively. (a) A cartoon representation of EV71 VLP protomer. (b) A surface representation of EV71 VLP viewed along the twofold axis. The 60 copies of EV71–SP70 peptides were uniformly displayed on the surface of EV71 VLP
The use of a recombinant adenovirus to produce EV71 VLPs was also reported [17]. The EV71 P1 and 3CD coding sequences were inserted into the E1/E3-deleted adenoviral genome, and the resulting recombinant adenovirus pAd-EVVLP was used to infect HEK-293A cells to produce EV71 VLPs in addition to Ad-EVVLP particles. Mouse immunogenicity studies showed that Ad-EVVLP-immunized antisera neutralized the EV71 B4 and C2 genotypes. In addition, Ad-EVVLP-vaccinated mice were 100 % protected from EV71 infection and demonstrated reduced viral load in both the CNS and muscle tissues in a hSCARB2 transgenic (hSCARB2-Tg) mouse challenge model. This study also showed that Ad-EVVLP successfully induced anti-CVA16 immunities, although no neutralizing activity against CVA16.
2.1.4 EV71 P1 or VP1 as the immunogen
There are also other types of EV71 vaccine candidates. The precursor of EV71 capsid proteins P1, expressed in P. pastoris, was shown to be immunogenic and capable of eliciting improved humoral and cellular immune responses while also providing good cross-protection with different EV71 strains compared with the heat-inactivated EV71 [18].
The VP1 capsid protein contains a number of identified neutralization epitopes and has been expressed and delivered by a variety of systems, including the attenuated Salmonella enterica serovar Typhimurium strains [19], Bifidobacterium longum [20], transgenic tomato [21] and milk [22]. The VP1 capsid has been shown to be capable of inducing neutralizing antibodies; however, this process occurs at a much lower titer than those induced by inactivated vaccines or VLPs.
2.1.5 Synthetic peptide-based vaccine
Synthetic peptide vaccines based on defined epitopes have also been tested as EV71 vaccine candidates. The synthetic peptides SP55 and SP70, corresponding to the identified neutralization linear epitopes in VP1 (amino acid 163–177 and 208–222, respectively), are both capable of eliciting neutralizing antibodies against EV71 in a microneutralization assay [23]. Immunization of mice with either SP55 or SP70 triggered an EV71-specific IgG response as high as that obtained with the whole virion used as an immunogen. In addition, EV71-neutralizing antibodies elicited by the synthetic peptide SP70 were able to confer good in vivo passive protection against homologous and heterologous EV71 strains in suckling BALB/c mice. Another synthetic peptide VP2-28 (residues 136–150 in VP2) was found to bind to mAb979 and showed cross-neutralizing activity against different genotypes of EV71 virus [24], and this binding inhibited the binding of mAb979 to EV71.
2.1.6 EV71 neutralization epitopes presented in heterologous systems
Another strategy is to incorporate the polypeptide sequences corresponding to the identified linear neutralization epitopes into a heterologous expression system.
In one study, immunization with a recombinant adenovirus type 3 (Ad3) with SP70 incorporated into the surface-exposed domains HVR1 or HVR2 of the capsid protein hexon elicited higher SP70-specific IgG titers, higher neutralization titers, and conferred more effective protection to neonatal mice [25].
In the second study, fusions of hepatitis B core antigen (HBc) with the SP55 or SP70 epitope of EV71 led to self-assembly of VLPs with the epitopes displayed on the surface [26]. Immunization with these chimeric VLPs induced carrier- and epitope-specific antibody responses in mice [26].
In the third study, a novel EV71 vaccine candidate based on recombinant multiple tandem linear neutralizing epitopes (mTLNE) was expressed in E. coli [27]. Passive transfer with anti-mTLNE sera conferred full protection against a lethal EV71 challenge in neonatal mice.
In summary, among all the vaccine candidates mentioned above, EV71-inactivated vaccine has come into clinical trials with high efficacy; EV71-attenuated live vaccine has safety concerns; EV71 VLPs can elicit high neutralization titers, and it is another promising vaccine candidate for EV71; other types of EV71 vaccine candidates still need further preclinical investigation.
2.2 Vaccine development against CVA16
CVA16 is another major causative agent for HFMD. HFMD caused by CVA16 is generally thought to be mild and self-limiting. However, several severe and fatal cases involving CVA16 infection were reported recently [32, 33]. Furthermore, coinfection with CVA16 and EV71 can cause serious complications in the central nervous system and increase the chance of genetic recombination [34]. Therefore, it is necessary to develop vaccines against CVA16.
2.2.1 Inactivated CVA16 vaccine
Several groups have worked on inactivated CVA16 vaccines (Table 2). In one study, immunization with a CVA16-inactivated vaccine (B1b subgenotype) induced neutralizing antibodies and protected mice against a lethal challenge [35]. The resulting anti-CVA16 mouse sera neutralized both homologous and heterologous CVA16 clinical isolates. Passive transfer of anti-CVA16 neutralizing sera partially protected neonatal mice from a CVA16 lethal challenge.
In the second study, the β-propiolactone (BPL)-inactivated CVA16 vaccine [419/CVA16 (C1 subgenotype)] could protect mouse pups from a lethal challenge with the CVA16 virus [1131/CVA16 (C3 subgenotype)] [36].
In the third study, the inactivated CVA16 vaccine formulated with an alum adjuvant protected neonatal mice born to immunized female mice from homologous and heterologous lethal viral challenges [37].
In the fourth study, an inactivated CVA16 vaccine was prepared using human diploid cells, and the vaccine’s immunogenicity was analyzed in mice and rhesus monkeys [38]. The neutralizing antibody had cross-neutralizing activity against different viral strains (genotype A and B). These results demonstrated that the inactivated vaccine can provide broad protection against heterologous CVA16 strains.
2.2.2 CVA16 virus-like particle vaccine
Other than the inactivated vaccine, CVA16 VLPs are vaccine candidates also under development (Table 2). In one study, Liu et al. [39] first reported the generation of CVA16 VLPs by coexpression of P1 and 3CD in a baculovirus expression system. Immunization with CVA16 VLPs induced high-titer neutralizing antibodies in mice, and the anti-VLP mouse sera conferred passive protection against a lethal challenge with either homologous or heterologous CVA16 strains. These results demonstrated that neutralizing antibodies constitute the major protective immunity against CVA16 infection and that CVA16 VLPs are a promising vaccine candidate. This is the first successful step toward the development of a safe and effective vaccine against CVA16 infection. In another study, the insect cell-produced CVA16 VLPs were also shown to be able to efficiently elicit cross-reactive neutralizing antibodies against diverse CVA16 strains [40].
Moreover, our studies showed that the coexpression of CVA16–P1 and CVA16–3CD led to self-assembly of CVA16 VLPs in S. cerevisiae and that these VLPs could elicit protective immunity against CVA16 in mice [41].
2.2.3 Peptide-based vaccine
In 2013, Shi et al. [42] reported the identification of six neutralizing linear epitopes of CVA16. Mice immunized with these six peptides generated peptide-specific serum antibodies, which can neutralize both homologous and heterologous CVA16 strains. Sequence alignment showed that these epitopes are extremely conserved among CVA16 strains of different genotypes. These findings have important implications for the development of broadly protective peptide-based CVA16 vaccines. However, peptides are typically weak immunogenic. Future efforts should focus on enhancing the immunogenicity of the epitopes using novel presentation platforms or formulations with novel adjuvants.
Collectively, CVA16-inactivated vaccine and VLPs had promising results against CVA16, while other types of vaccines still need further investigation.
2.3 Multivalent vaccine development against HFMD
2.3.1 Necessity
Although EV71 and CVA16 are recognized as the major causative agents responsible for HFMD, an epidemiology study indicated that it is necessary to take other viruses into consideration for improved prevention and control of HFMD. For example, the Finnish HFMD outbreak in 2008 was caused by two infrequently detected, cocirculating coxsackie A viruses: CVA6 and CVA10 [4]. Analysis of samples from a total of 1182 patients who presented with the symptoms of HFMD (67.3 %) or herpangina (HA) (16.7 %) in Thailand during 2008–2013 showed that 59.7 % of those patients were pan-enterovirus positive, comprising 9.1 % EV71 and 31.2 % coxsackie A viruses (CVA) including 70.5 % CVA6, 27.6 % CVA16, 1.1 % CVA10 and 0.8 % CVA5 [43]. Another study on the samples from HFMD patients in Thailand in 2012 [5] identified CAV6 (33.5 %) followed by CAV16 (9.4 %) and EV71 (8.8 %) as the most frequent genotypes in HFMD. Collectively, recent data have indicated that CVA6 has emerged as the predominant causative agent in Southern China and Thailand since 2012 [44]. They have also shown that 8.3 % of CVA6-infected patients developed meningo encephalitis and presented with a high fever. In addition, human enterovirus 30 has been detected cocirculating with EV71 in a large outbreak of HFMD in Guangxi, China, during March–April of 2010 [6]. Thus, the causative agents for HFMD include EV71, CVA16, CVA6 and other viruses, and it is important to take this observation into consideration when developing an effective vaccine against HFMD.
Although EV71-inactivated vaccines have proven efficacious in preventing EV71-associated HFMD in clinical trials, the data from preclinical and clinical studies indicate that monovalent EV71 vaccines do not provide sufficient protection against infection by CVA16 and other enteroviruses [10, 45, 46]. Therefore, it is necessary to develop a multivalent vaccine for broad protection against HFMD.
Recently, bivalent EV71/CVA16 vaccine candidates, including both inactivated viruses and VLPs, have been developed and observed to efficiently protect against EV71 and CVA16 infection in mice (Table 3). These studies represent the first step toward multivalent vaccines for broad protection against HFMD.
2.3.2 Bivalent EV71-/CVA16-inactivated whole-virus vaccine
2.3.2.1 Combination
In one study, Cai et al. [46] reported that a combination vaccine composed of inactivated EV71 and CVA16 immunized sera efficiently neutralized both EV71 and CVA16. More importantly, passive immunization with this bivalent vaccine protected mice from both an EV71 and a CVA16 lethal challenge. In another study, Lin et al. [48] reported that a PELC-/CpG-formulated formalin-inactivated EV71/CVA16 bivalent vaccine could elicit the highest IgG antibody titers against both EV71 and CVA16 in mice. Together, these data demonstrated that the combination approach could be extended to the development of future multivalent vaccines against HFMD.
2.3.2.2 Recombinant viruses
In 2013, it was demonstrated that the VP1 BC loop in EV71 could be subjected to the insertion of foreign polypeptides of various lengths while preserving both the function of the inserted polypeptide and viral replication [49]. Successful rescue of these recombinant viruses demonstrated that the VP1 BC loop exposed on the surface of EV71 is able to accommodate a broad range of sequences, leading to the hypothesis that recombinant EV71 may be developed as novel vaccines.
Later, we reported the crystal structures of an empty particle from a clinical C4 strain EV71 and one EV71 recombinant virus, showing that such insertions into the VP1 BC loop do not affect the overall capsid assembly and structure [50]. Moreover, we presented the crystal structure of an uncoating intermediate of another EV71 recombinant virus, demonstrating that such insertions do not seem to affect the viral uncoating process and thus virus replication. Therefore, the generation of inactivated recombinant EV71 viruses containing neutralization epitopes of other HFMD causative agents can be another approach toward multivalent vaccine development.
2.3.3 Bivalent EV71/CVA16 VLPs
2.3.3.1 Combination
In 2014, Gong et al. [40] reported that the combination of EV71 VLPs and CVA16 VLPs can elicit a neutralizing antibody response to both viruses. In addition, Ku et al. [45] reported that a bivalent vaccine composed of EV71- and CVA16 VLPs induced a balanced neutralizing antibody response in mice. The bivalent vaccine passively protected mice against EV71 and CVA16 infections. These data indicated that bivalent EV71/CVA16 VLP vaccine candidates are capable of eliciting balanced protective immunity against both viruses and thus warrant further development.
2.3.3.2 Chimeric VLPs
Recently, Zhao et al. [47] reported a novel strategy to produce EV71/CVA16 chimeric VLPs in which the neutralizing epitope SP70 within VP1 of EV71 VLPs was replaced with that of CVA16. Immunization with the chimeric VLPs in mice elicited robust Th1-/Th2-dependent immune responses against EV71 and CVA16. Furthermore, passive immunization with anti-chimeric VLP sera conferred full protection against a lethal challenge of both EV71 and CVA16 infection in neonatal mice.
Structural analysis revealed that the overall structure of the chimeric VLPs was rather similar to that of EV71 VLPs [51]. The replaced CVA16–SP70 epitope is well exposed on the surface of chimeric VLPs. The substitution of only four residues in the VP1 GH loop converted strongly negative charged surface patches formed by portions of the SP70 epitope in EV71 VLPs into a relatively neutral surface in the chimeric VLPs, which likely accounted for the additional neutralization capability of the chimeric VLPs against CVA16 infection. These results suggested that chimeric VLPs have the potential for further development as a future multivalent HFMD vaccine.
3 Neutralizing antibodies
Neutralizing monoclonal antibodies are specific antiviral agents that can be used for the passive immunization of patients with acute viral infections. Human monoclonal antibodies are a promising and rapidly growing category of targeted therapeutic agents, with 7 approved in the USA, 3 under review by the FDA, 7 in late-stage development and 81 in early-stage development [52].
3.1 Neutralizing antibodies against EV71
While no specific treatment options exist yet to treat HFMD patients, several neutralizing antibodies of therapeutic potential against EV71 have been identified and characterized (Fig. 2).
Footprints of neutralizing antibodies on the EV71 surface. Surface representation of the EV71 pentamer is colored in gray. The footprints of mAb22A12 (residues 215, 217, 218 and 219 in VP1), mAb979 (residues 136–150 in VP2), mAb28-7 (residues 98, 145, 242 and 244 in VP1), mAbE18 (residue 149 in VP2 and residues between VP4–VP2–VP3–VP1 protomers), mAbBB1A5 (residues 141–155 in VP2) and mAb10D3 (residues 59, 62, 67 in VP3) are colored in red, cyan, yellow, green, magenta and blue, respectively. The footprints of mAb979, mAbE18, and mAbBB1A5 have overlap regions
3.1.1 mAb22A12
Purified murine monoclonal antibody 22A12 was raised against the SP70 peptide of EV71 and shows strong neutralizing activity against EV71 in vitro [53]. It is likely that mAb22A12 neutralizes EV71 infections predominantly by cross-linking capsids [54] (Table 4). However, the EV71 procapsid contains a more favorable mAb22A12 binding site (the canyon in the region of the VP1 GH loop) than does the virus [54]. It was hypothesized that the procapsid can act in vitro as an antibody “sink”, effectively sequestering antibodies and consequently allowing viral infection. These findings suggested a revised strategy for the design and evaluation of therapeutics against EV71 infection.
3.1.2 mAb979
The mAb979 antibody (IgG1 subclass) was obtained from Chemicon International (lot#LV1412938). It has cross-neutralizing activity against different genotypes of EV71, neutralizing isolates of the B4, B5 and C4 subgenotypes with titers of 128, 64 and 32, respectively [24]. It recognizes the cross-genotype neutralization epitope VP2-28 (residues 136–150) of EV71.
3.1.3 mAb28-7
The mAb28-7 antibody can only neutralize specific strains of EV71 [55]. It showed weak binding to SK-EV006 (B3), C7/Osaka (B4) and 1095/Shiga (C2), with a lack of binding to strains BrCr/tr (A), Nagoya (B1) and Bulgaria (B1). The footprint of the Fab includes VP1-145 and residues that map to the positively charged patches (VP1-98, VP1-242, and VP1-244) around the fivefold axis, overlapping with the binding sites of P-selectin glycoprotein ligand-1 and heparan sulfate.
3.1.4 mAb22 and mAb24
A live EV71 isolate Tainan/4643/98 (subgenotype C2) was used as the immunogen to sensitize BALB/c (H-2(d)) mice and generate EV71-specific murine monoclonal antibodies [56]. mAb22 and mAb24 exhibited potent neutralizing activities against EV71 and protected cells from infection. mAb22 could react with the EV71 subgenotypes B5, C2 and C4, while mAb24 could react with the EV71 subgenotypes B4, B5, C2 and C4. Western blot analysis revealed that both of these mAbs reacted with EV71 VP1.
3.1.5 mAbE18
The mAbE18 antibody was prepared by immunizing mice with empty immature EV71 (MY104 (B3)) particles [57]. It could neutralize the virus as intact antibodies or as Fab fragments. The binding sites on the virus capsids are located between the VP4–VP2–VP3–VP1 protomers, including Lys-149 of VP2 that has been implicated to play a role in the attachment of EV71 to the P-selectin glycoprotein ligand-1. Binding of this antibody to EV71 causes the virus to change its conformation to that of an A-particle, followed by the ejection of much of its genome. Thus, E18 has potential as an anti-EV71 therapy.
3.1.6 mAbBB1A5
The mAbBB1A5 antibody was generated by immunization with an activated whole EV71 virus of strain 52–3 (subgenotype C4) [58]. It showed a cross-genotype neutralizing ability against EV71 strains of the B3, B4, C2 and C5 subgenotypes with titers of 1:32. It recognizes the epitope spanning amino acids 141–155 within the VP2 of EV71.
3.1.7 mAb10D3
The mAb10D3 was able to neutralize representative strains of all EV71 subgenotypes without cross-reaction to CVA16 [59]. It recognizes the “knob” of VP3, a conserved conformational epitope of EV71. This antibody (administered at a dose of 10 mg/g of body weight) was able to achieve 100 % protection against the lethal EV71 challenge. Thus, it is an ideal candidate for treatment against EV71 infection.
3.2 Neutralizing antibodies against CVA16
3.2.1 mAb979
In 2011, Liu et al. [24] reported that mAb979 is also able to recognize and neutralize CVA16 (data not shown). Alignment of the corresponding VP2-28 amino acid sequence derived from CVA16 revealed a high degree of homology (Fig. 3b).
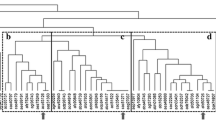
A multiple sequence alignment of VP1–SP70 and VP2-28 regions in different enteroviruses. Both VP1–SP70 and VP2-28 are neutralization epitopes identified in EV71. Capsid protein sequences of VP1 used for the alignment include EV71 subgenotypes A–C5, CVA16 genotypes A–C, CVA6, CVA10, CVA8 and EC30. Capsid protein sequences of VP2 used for the alignment include EV71 subgenotypes A, B2, B4, C2, C4, CVA16 genotypes A–B, CVA6, CVA10, CVA8 and EC30. The residue numbers correspond to those in EV71. Conserved residues are shown in white with a red background. This figure was produced using ESPript 3.0 [60]
3.3 Broadly neutralizing antibodies against HFMD
As mentioned above, mAb979 (IgG1 subclass) has cross-neutralizing activity against different genotypes of EV71, including B4, B5 and C4 [24], by the recognition of a cross-genotype neutralization epitope VP2-28 (residues 136–150) of EV71. In addition, it can neutralize CVA16 (data not shown) [24]. Alignment of the corresponding VP2-28 amino acid sequence derived from different strains of EV71 and CVA16 revealed a high degree of homology (Fig. 3b). Thus, mAb979 has a potential to be developed into a broadly neutralizing antibody.
In addition, multiple sequence alignment revealed high sequence similarity in the SP70 region in different EV71 and CVA16 subgenogroups (Fig. 3a). Thus, by targeting the SP70 region, broadly neutralizing antibodies against different EV71 and CVA16 strains may be developed.
4 Conclusions and perspectives
HFMD has become a serious health threat to the children of the Asia–Pacific regions. A number of enteroviruses, including EV71, CVA16, CVA6 and others, have been found to be the causative agents for the recent HFMD outbreaks. To better prevent and control HFMD, development of multivalent vaccines and broadly neutralizing therapeutic antibodies are urgently needed. The completion of phase III clinical trials of EV71-inactivated whole-virus vaccines represents the first step toward this goal. The generation of bivalent EV71/CVA16 vaccine candidates composed of EV71- and CVA16-inactivated viruses or EV71 and CVA16 VLPs has paved the way for the development of multivalent vaccines. Particularly, the production of EV71 recombinant viruses by the insertion into the VP1 BC loop and the chimeric EV71/CVA16 VLPs by the substitution of amino acids in the VP1 GH loop have provided insights into novel multivalent vaccine design.
Neutralization antibodies deserve more attention for therapeutic development against HFMD. For example, mAb979 has the potential to be further developed for clinical use. Structural determination of the complexes formed between mAb979 and EV71 or CVA16 may lead to the engineering of a more potent and broadly neutralizing antibody against HFMD. In addition, understanding the working mechanism during enterovirus infection, uncoating and replication may lead to better strategies for the development of broad-spectrum therapeutics against HFMD.
References
McMinn PC (2012) Recent advances in the molecular epidemiology and control of human enterovirus 71 infection. Curr Opin Virol 2:199–205
Chan LG, Parashar UD, Lye MS et al (2000) Deaths of children during an outbreak of hand, foot, and mouth disease in Sarawak, Malaysia: clinical and pathological characteristics of the disease. For the outbreak study group. Clin Infect Dis 31:678–683
Racaniello VR (2007) Picornaviridae: the viruses and their replication. In: Knipe DM, Howley PM, Lamb RA et al (eds) Fields virology, 5th edn. Lippincott Williams & Wilkins, Philadephia, pp 795–838
Blomqvist S, Klemola P, Kaijalainen S et al (2010) Co-circulation of coxsackie viruses A6 and A10 in hand, foot and mouth disease outbreak in Finland. J Clin Virol 48:49–54
Puenpa J, Mauleekoonphairoj J, Linsuwanon P et al (2014) Prevalence and characterization of enterovirus infections among pediatric patients with hand foot mouth disease, herpangina and influenza like illness in Thailand, 2012. PLoS One 9:e98888
Han JF, Cao RY, Jiang T et al (2011) Echovirus 30 in EV71-associated hand, foot and mouth disease outbreak, Guangxi, China. J Clin Virol 50:348–349
Chou AH, Liu CC, Chang CP et al (2012) Pilot scale production of highly efficacious and stable enterovirus 71 vaccine candidates. PLoS One 7:e34834
Zhu FC, Meng FY, Li JX et al (2013) Efficacy, safety, and immunology of an inactivated alum-adjuvant enterovirus 71 vaccine in children in China: a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 381:2024–2032
Zhu F, Xu W, Xia J et al (2014) Efficacy, safety, and immunogenicity of an enterovirus 71 vaccine in China. N Engl J Med 370:818–828
Li R, Liu L, Mo Z et al (2014) An inactivated enterovirus 71 vaccine in healthy children. N Engl J Med 370:829–837
Arita M, Shimizu H, Nagata N et al (2005) Temperature-sensitive mutants of enterovirus 71 show attenuation in cynomolgus monkeys. J Gen Virol 86:1391–1401
Hu YC, Hsu JT, Huang JH et al (2003) Formation of enterovirus-like particle aggregates by recombinant baculoviruses co-expressing P1 and 3CD in insect cells. Biotechnol Lett 25:919–925
Chung YC, Huang JH, Lai CW et al (2006) Expression, purification and characterization of enterovirus-71 virus-like particles. World J Gastroenterol 12:921–927
Chung YC, Ho MS, Wu JC et al (2008) Immunization with virus-like particles of enterovirus 71 elicits potent immune responses and protects mice against lethal challenge. Vaccine 26:1855–1862
Li HY, Han JF, Qin CF et al (2013) Virus-like particles for enterovirus 71 produced from Saccharomyces cerevisiae potently elicits protective immune responses in mice. Vaccine 31:3281–3287
Zhang C, Ku Z, Liu Q et al (2015) High-yield production of recombinant virus-like particles of enterovirus 71 in Pichia pastoris and their protective efficacy against oral viral challenge in mice. Vaccine 33:2335–2341
Tsou YL, Lin YW, Shao HY et al (2015) Recombinant adeno-vaccine expressing enterovirus 71-Like particles against hand, foot, and mouth disease. PLoS Negl Trop Dis 9:e0003692
Han X, Ying XL, Zhou SL et al (2014) Characterization of the enterovirus 71 P1 polyprotein expressed in Pichia pastor as a candidate vaccine. Hum Vaccin Immunother 10:2220–2226
Chiu CH, Chu C, He CC et al (2006) Protection of neonatal mice from lethal enterovirus 71 infection by maternal immunization with attenuated Salmonella enterica serovar Typhimurium expressing VP1 of enterovirus 71. Microbes Infect 8:1671–1678
Yu Z, Huang Z, Sao C et al (2013) Oral immunization of mice using Bifidobacterium longum expressing VP1 protein from enterovirus 71. Arch Virol 158:1071–1077
Chen HF, Chang MH, Chiang BL et al (2006) Oral immunization of mice using transgenic tomato fruit expressing VP1 protein from enterovirus 71. Vaccine 24:2944–2951
Chen HL, Huang JY, Chu TW et al (2008) Expression of VP1 protein in the milk of transgenic mice: a potential oral vaccine protects against enterovirus 71 infection. Vaccine 26:2882–2889
Foo DG, Alonso S, Phoon MC et al (2007) Identification of neutralizing linear epitopes from the VP1 capsid protein of enterovirus 71 using synthetic peptides. Virus Res 125:61–68
Liu CC, Chou AH, Lien SP et al (2011) Identification and characterization of a cross-neutralization epitope of enterovirus 71. Vaccine 29:4362–4372
Tian X, Su X, Li X et al (2012) Protection against enterovirus 71 with neutralizing epitope incorporation within adenovirus type 3 hexon. PLoS One 7:e41381
Ye X, Ku Z, Liu Q et al (2014) Chimeric virus-like particle vaccines displaying conserved enterovirus 71 epitopes elicit protective neutralizing antibodies in mice through divergent mechanisms. J Virol 88:72–81
Li YX, Zhao H, Cao RY et al (2014) Recombinant tandem multi-linear neutralizing epitopes of human enterovirus 71 elicited protective immunity in mice. Virol J 11:79
Lee MS, Chang LY (2010) Development of enterovirus 71 vaccines. Expert Rev Vaccines 9:149–156
Chung CY, Chen CY, Lin SY et al (2010) Enterovirus 71 virus-like particle vaccine: improved production conditions for enhanced yield. Vaccine 28:6951–6957
Lin YL, Yu CI, Hu YC et al (2012) Enterovirus type 71 neutralizing antibodies in the serum of macaque monkeys immunized with EV71 virus-like particles. Vaccine 30:1305–1312
Ku Z, Ye X, Huang X et al (2013) Neutralizing antibodies induced by recombinant virus-like particles of enterovirus 71 genotype C4 inhibit infection at pre- and post-attachment steps. PLoS One 8:e57601
Mao Q, Wang Y, Yao X et al (2014) Coxsackievirus A16: epidemiology, diagnosis, and vaccine. Hum Vaccin Immunother 10:360–367
Xu W, Liu CF, Yan L et al (2012) Distribution of enteroviruses in hospitalized children with hand, foot and mouth disease and relationship between pathogens and nervous system complications. Virol J 9:8
Liu W, Wu S, Xiong Y et al (2014) Co-circulation and genomic recombination of coxsackievirus A16 and enterovirus 71 during a large outbreak of hand, foot, and mouth disease in central China. PLoS One 9:e96051
Cai Y, Liu Q, Huang X et al (2013) Active immunization with a coxsackievirus A16 experimental inactivated vaccine induces neutralizing antibodies and protects mice against lethal infection. Vaccine 31:2215–2221
Qi AW, Guo SZ, Wen PR et al (2014) The immunogenicity and protection effect of the BPL-inactivated CA16 vaccine in different animal systems. Hum Vaccin Immunother 10:628–639
Li J, Chang J, Liu X et al (2014) Protection from lethal challenge in a neonatal mouse model by circulating recombinant form coxsackievirus A16 vaccine candidates. J Gen Virol 95:1083–1093
Yang E, Cheng C, Zhang Y et al (2014) Comparative study of the immunogenicity in mice and monkeys of an inactivated CA16 vaccine made from a human diploid cell line. Hum Vaccin Immunother 10:1266–1273
Liu Q, Yan K, Feng Y et al (2012) A virus-like particle vaccine for coxsackievirus A16 potently elicits neutralizing antibodies that protect mice against lethal challenge. Vaccine 30:6642–6648
Gong M, Zhu H, Zhou J et al (2014) Cryo-electron microscopy study of insect cell-expressed enterovirus 71 and coxsackievirus a16 virus-like particles provides a structural basis for vaccine development. J Virol 88:6444–6452
Zhao H, Li HY, Han JF et al (2013) Virus-like particles produced in Saccharomyces cerevisiae elicit protective immunity against coxsackievirus A16 in mice. Appl Microbiol Biotechnol 97:10445–10452
Shi J, Huang X, Liu Q et al (2013) Identification of conserved neutralizing linear epitopes within the VP1 protein of coxsackievirus A16. Vaccine 31:2130–2136
Linsuwanon P, Puenpa J, Huang SW et al (2014) Epidemiology and seroepidemiology of human enterovirus 71 among Thai populations. J Biomed Sci 21:16
Chen YJ, Chang SC, Tsao KC et al (2012) Comparative genomic analysis of coxsackievirus A6 strains of different clinical disease entities. PLoS One 7:e52432
Ku Z, Liu Q, Ye X et al (2014) A virus-like particle based bivalent vaccine confers dual protection against enterovirus 71 and coxsackievirus A16 infections in mice. Vaccine 32:4296–4303
Cai Y, Ku Z, Liu Q et al (2014) A combination vaccine comprising of inactivated enterovirus 71 and coxsackievirus A16 elicits balanced protective immunity against both viruses. Vaccine 32:2406–2412
Zhao H, Li HY, Han JF et al (2015) Novel recombinant chimeric virus-like particle is immunogenic and protective against both enterovirus 71 and coxsackievirus A16 in mice. Sci Rep 5:7878
Lin CW, Liu CC, Lu TC et al (2014) Immunogenicity studies of bivalent inactivated virions of EV71/CVA16 formulated with submicron emulsion systems. Biomed Res Int 2014:670506
Wang G, Cao RY, Chen R et al (2013) Rational design of thermostable vaccines by engineered peptide-induced virus self-biomineralization under physiological conditions. Proc Natl Acad Sci USA 110:7619–7624
Lyu K, Wang GC, He YL et al (2015) Crystal structures of enterovirus 71 (EV71) recombinant virus particles provide insights into vaccine design. J Biol Chem 290:3198–3208
Lyu K, He YL, Li HY et al (2015) Crystal structures of yeast-produced enterovirus 71 and enterovirus 71/coxsackievirus A16 chimeric virus-like particles provide the structural basis for novel vaccine design against hand-foot-and-mouth disease. J Virol 89:6196–6208
Nelson AL, Dhimolea E, Reichert JM (2010) Development trends for human monoclonal antibody therapeutics. Nat Rev Drug Discov 9:767–774
Li X, Mao C, Ma S et al (2009) Generation of neutralizing monoclonal antibodies against enterovirus 71 using synthetic peptides. Biochem Biophys Res Commun 390:1126–1128
Shingler KL, Cifuente JO, Ashley RE et al (2015) The enterovirus 71 procapsid binds neutralizing antibodies and rescues virus infection in vitro. J Virol 89:1900–1908
Lee H, Cifuente JO, Ashley RE et al (2013) A strain-specific epitope of enterovirus 71 identified by cryo-electron microscopy of the complex with fab from neutralizing antibody. J Virol 87:11363–11370
Xu L, Huang KJ, Ho TS et al (2013) Monoclonal antibodies for diagnosis of enterovirus 71. Monoclon Antib Immunodiagn Immunother 32:386–394
Plevka P, Lim PY, Perera R et al (2014) Neutralizing antibodies can initiate genome release from human enterovirus 71. Proc Natl Acad Sci USA 111:2134–2139
Xu L, He D, Li Z et al (2014) Protection against lethal enterovirus 71 challenge in mice by a recombinant vaccine candidate containing a broadly cross-neutralizing epitope within the VP2 EF loop. Theranostics 4:498–513
Kiener TK, Jia Q, Meng T et al (2014) A novel universal neutralizing monoclonal antibody against enterovirus 71 that targets the highly conserved “knob” region of VP3 protein. PLoS Negl Trop Dis 8:e2895
Robert X, Gouet P (2014) Deciphering key features in protein structures with the new ENDscript server. Nucleic Acids Res 42:W320–W324
Acknowledgments
This work was supported by the National Basic Research Program of China (2010CB912403) and the National Natural Science Foundation of China (31370730 and 31070144). We would like to thank all our laboratory members and apologize to colleagues whose work cannot be cited in this review due to space constraints.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Lyu, K., Chen, R. Achievements, challenges and prospects for the development of broadly protective multivalent vaccines and therapeutic antibodies against hand, foot and mouth disease. Sci. Bull. 60, 1305–1315 (2015). https://doi.org/10.1007/s11434-015-0847-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11434-015-0847-3