Abstract
Purpose
The aim of this study was to determine an appropriate cutoff value and the number of nights of sleep with the portable single-channel EMG device (GrindCare) necessary for a valid sleep bruxism (SB) diagnosis.
Methods
Twenty consecutive post-graduate students and staff at Bauru School of Dentistry composed the sample. Each participant underwent the GrindCare for five consecutive nights and the polysomnography (PSG). The discrimination between bruxers and non-bruxers was based only on the PSG analysis. Data about electromyography per hour with GrindCare (EMG/h) and PSG (bursts/h) were scored.
Results
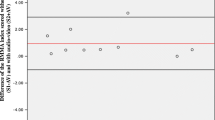
There were positive correlations between the two devices for EMG/h and bursts/h in three and five consecutive nights. Bland-Altman analysis of the EMG bursts/h showed positive agreement between the methods. The receiver operating characteristic (ROC) analyses also showed that using a minimum of 18 EMG/h for three nights and 19 EMG/h for five nights in GrindCare as cutoffs resulted in a 90 % specificity and positive likelihood ratio equal to 5.
Conclusions
GrindCare is able to discriminate SB diagnosed by PSG and gold standard criteria, when used for three or five consecutive nights, and it may be a valid choice in clinical practice for SB assessment.


Similar content being viewed by others
References
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd edn. American Academy of Sleep Disorders, Darien
Lobbezoo F, Ahlberg J, Glaros AG et al (2013) Bruxism defined and graded: an international consensus. J Oral Rehabil 40:2–4. doi:10.1111/joor.12011
Lavigne GJ, Khoury S, Abe S et al (2008) Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil 35:476–494. doi:10.1111/j.1365-2842.2008.01881.x
Rompré PH, Daigle-Landry D, Guitard F et al (2007) Identification of a sleep bruxism subgroup with a higher risk of pain. J Dent Res 86:837–842
Lavigne GJ, Rompré PH, Montplaisir JY (1996) Sleep bruxism: validity of clinical research diagnostic criteria in a controlled polysomnographic study. J Dent Res 75:546–552
Kato T, Dal-Fabbro C, Lavigne GJ (2003) Current knowledge on awake and sleep bruxism: overview. Alpha Omegan 96:24–32
Koyano K, Tsukiyama Y, Ichiki R, Kuwata T (2008) Assessment of bruxism in the clinic. J Oral Rehabil 35:495–508. doi:10.1111/j.1365-2842.2008.01880.x
Carra MC, Huynh N, Lavigne G (2012) Sleep bruxism: a comprehensive overview for the dental clinician interested in sleep medicine. Dent Clin North Am 56:387–413. doi:10.1016/j.cden.2012.01.003
Jadidi F, Castrillon E, Svensson P (2008) Effect of conditioning electrical stimuli on temporalis electromyographic activity during sleep. J Oral Rehabil 35:171–183. doi:10.1111/j.1365-2842.2007.01781.x
Conti PCR, Stuginski-Barbosa J, Bonjardim LR et al (2014) Contingent electrical stimulation inhibits jaw muscle activity during sleep but not pain intensity or masticatory muscle pressure pain threshold in self-reported bruxers: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol 117:45–52. doi:10.1016/j.oooo.2013.08.015
Haugland MS, Huynh N, Lavigne G (2011) Single-channel EMG versus PSG scoring of RMMA in sleep bruxers
Dworkin SF, LeResche L (1992) Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 6:301–355
Raphael KG, Janal MN, Sirois DA, Svensson P (2013) Effect of contingent electrical stimulation on masticatory muscle activity and pain in patients with a myofascial temporomandibular disorder and sleep bruxism. J Orofac Pain 27:21–31
Iber C, Anacoli-Israel S, Chesson A, Quen S (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, 1st edn. American Academy of Sleep Medicine, Westchester
Carra MC, Huynh N, Lavigne GJ (2015) Diagnostic accuracy of sleep bruxism scoring in absence of audio-video recording: a pilot study. Sleep Breath 19:183–190. doi:10.1007/s11325-014-0986-9
Yachida W, Castrillon EE, Baad-Hansen L et al (2012) Craniofacial pain and jaw-muscle activity during sleep. J Dent Res 91:562–567. doi:10.1177/0022034512446340
Van Der Zaag J, Lobbezoo F, Visscher CM et al (2008) Time-variant nature of sleep bruxism outcome variables using ambulatory polysomnography: implications for recognition and therapy evaluation. J Oral Rehabil 35:577–584. doi:10.1111/j.1365-2842.2008.01893.x
Bland JM, Altman DG (2010) Statistical methods for assessing agreement between two methods of clinical measurement. Int J Nurs Stud 47:931–936. doi:10.1016/j.ijnurstu.2009.10.001
Zou KH, O’Malley AJ, Mauri L (2007) Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation 115:654–657. doi:10.1161/CIRCULATIONAHA.105.594929
Deeks JJ, Altman DG (2004) Diagnostic tests 4: likelihood ratios. BMJ 329:168–169. doi:10.1136/bmj.329.7458.168
Grimes DA, Schulz KF (2005) Refining clinical diagnosis with likelihood ratios. Lancet 365:1500–1505. doi:10.1016/S0140-6736(05)66422-7
Widmer CG, Lund JP, Feine JS (1990) Evaluation of diagnostic tests for TMD. J Calif Dent Assoc 18:53–60
Minakuchi H, Sakaguchi C, Hara ES et al (2012) Multiple sleep bruxism data collected using a self-contained EMG detector/analyzer system in asymptomatic healthy subjects. Sleep Breath 16:1069–1072. doi:10.1007/s11325-011-0602-1
Lavigne GJ, Guitard F, Rompré PH, Montplaisir JY (2001) Variability in sleep bruxism activity over time. J Sleep Res 10:237–244
Bernhardt O, Hawali S, Sümnig W, Meyer G (2012) Electrical stimulation of the temporalis muscle during sleep of myofascial pain—a pilot study. J Craniomandib Funct 4:197–210
Arima T, Tomonaga A, Yachida W et al (2012) Site-to-site variation of muscle activity and sensitivity in the human anterior temporalis muscle: implications for contingent stimulation. Acta Odontol Scand 70:89–95. doi:10.3109/00016357.2011.597778
Acknowledgments
This work was supported by FAPESP—Sao Paulo Research Foundation. The authors thank Maria Rita de Cássia Morateli Costa for scoring the PSG signals.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
National Counsel of Technological and Scientific Development—Brazil (142840/2011-4) and Sao Paulo Research Foundation (2012/01396-2) provided financial support in the form of researcher funding. The sponsor had no role in the design or conduct of this research.
Conflict of interest
P. Svensson is a paid consultant for Medotech A/S. Other authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Stuginski-Barbosa, J., Porporatti, A.L., Costa, Y.M. et al. Diagnostic validity of the use of a portable single-channel electromyography device for sleep bruxism. Sleep Breath 20, 695–702 (2016). https://doi.org/10.1007/s11325-015-1283-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-015-1283-y