Abstract
Purpose
Our aim was to determine the pathway underlying the effects of continuous positive airway pressure (CPAP) adherence on intimate relationship with bed partner in men with obstructive sleep apnea (OSA). We hypothesized that CPAP with good adherence affected the intimate relationship with bed partner directly and indirectly, and it was mediated through daytime sleepiness and activity level in men with OSA.
Methods
Data were obtained from an education program for enhancing CPAP adherence. Men who were newly diagnosed of OSA and CPAP therapy naïve were recruited in a tertiary teaching hospital.
Results
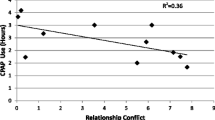
Self-reported quality of life [Functional Outcomes of Sleep Questionnaire], daytime sleepiness [Epworth Sleepiness Scale (ESS)], and negative emotion symptoms [depression, anxiety, stress scale] were assessed before and after CPAP treatment at 1-year assessment. Seventy-three men were included in the data analysis, with a mean ± SD age of 52 ± 10 years, body mass index of 29.0 ± 5.2 kg/m2, ESS of 9.5 ± 5.6, and median [interquartile range(IR)] apnea and hypopnea index of 31 (21, 56) events/h. The median (IR) CPAP daily usage was 4.3(0, 6.1) h/day. From the path analysis, CPAP therapy was shown to improve intimate relationship directly (ß = 0.185) and indirectly (ß = 0.050) by reducing daytime sleepiness and increasing activity level. However, negative emotion symptoms were not the mediators between CPAP adherence and the intimate relationship.
Conclusions
CPAP therapy with good adherence is related directly and indirectly to a better intimate relationship with bed partner in men with OSA. It was possibly attributed to reduced daytime sleepiness and increased activity level.




Similar content being viewed by others
References
McCabe MP, Althof SE, Assalian P, Chevret-Measson M, Leiblum SR, Simonelli C, Wylie K (2010) Psychological and interpersonal dimensions of sexual function and dysfunction. J Sex Med 7:327–336
Parmet S (2004) Male sexual dysfunction. JAMA 291(24):3076
Taskin U, Yigit O, Acioglu E, Aricigil M, Toktas G, Guzelhan Y (2010) Erectile dysfunction in severe sleep apnea patients and response to CPAP. Int J Impot Res 22:134–139
Santos T, Drummond M, Botelho F (2012) Erectile dysfunction in obstructive sleep apnea syndrome—prevalence and determinants. Pneumologia 18(2):64–71
Hirshkowitz M, Karacan I, Arcasoy MO, Acik G, Narter EM, Williams RL (1990) Prevalence of sleep apnea in men with erectile dysfunction. Urology 36(3):232–234
Pépin JL, Tamisier R, Godin-Ribuot D, Lévy PA (2015) Erectile dysfunction and obstructive sleep apnea: from mechanisms to a distinct phenotype and combined therapeutic strategies. Sleep Med Rev 20:1–4
Reishtein JL, Maislin G, Weaver TE, Multisite Study Group (2010) Outcome of CPAP treatment on intimate and sexual relationships in men with obstructive sleep apnea. J Clin Sleep Med 6(3):221–226
Nobre PJ (2010) Psychological determinants of erectile dysfunction: testing a cognitive-emotional model. J Sex Med 7(4 pt 1):1429–1437
Petersen M, Kristensen E, Berg S, Midgren B (2012) Sexual function in male patients with obstructive sleep apnoea after 1 year of CPAP treatment. Clin Respir J 7(2):214–219
Sánchez AI, Martínez P, Miró E, Bardwell WA, Buela-Casal G (2009) CPAP and behavioral therapies in patients with obstructive sleep apnea: effects on daytime sleepiness, mood, and cognitive function. Sleep Med Rev 13(3):223–233
Budweiser S, Luigart R, Jörres RA, Kollert F, Kleemann Y, Wieland WF, Pfeifer M (2013) Long-term changes of sexual function in men with obstructive sleep apnea after initiation of continuous positive airway pressure. J Sex Med 10(12):524–531
Luboshitzky R, Lavie L, Shen-Orr Z, Lavie P (2003) Pituitary gonadal function in men with obstructive sleep apnea: the effect of continuous positive airway pressure treatment. Neuro Endocrinol Lett 24:463–467
Weaver TE, Laizner AM, Evans LK, Maislin G, Chugh DK, Lyon K, Smith PL, Schwartz AR, Redline S, Pack AI, Dinges DF (1997) An instrument to measure functional status outcomes for disorders of excessive sleepiness. Sleep 20(10):835–843
Johns MW (1992) Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 15(4):376–381
Gloster AT, Rhoades HM, Novy D, Klotsche J, Senior AK, Kunik M, Wilson N, Stanley MA (2008) Psychometric properties of the Depression Anxiety and Stress Scale-21 in older primary care patients. J Affect Disord 110(3):248–259
Wagle KC, Carrejo MH, Tan RS (2012) The implications of increasing age on erectile dysfunction. Am J Men’s Health 6(4):273–279
Kolotkin RL, Zunker C, Østbye T (2012) Sexual functioning and obesity: A review. Obesity 20:2325–2333
Harte CB, Meston CM (2013) Association between cigarette smoking and erectile tumescence: the mediating role of heart rate variability. Int J Impot Res 25(4):155–159
Crowe LC, George WH (1989) Alcohol and human sexuality: review and integration. Psychol Bull 105(3):374–386
Stannek T, Hurny C, Schoch OD, Bucher T, Munzer T (2009) Factors affecting self-reported sexuality in men with obstructive sleep apnea syndrome. J Sex Med 6:3415–3424
Ahmed A, Alnaama A, DShams K, Salem M (2011) prevalence and risk factors of erectile dysfunction among patients attending primary health care in Qatar. East Mediterr Health J 17(7):587–592
Cohen J (1977) Statistical power analysis for the behavioral sciences, 2nd edn. Academic, New York
Bryman A, Cramer D (2005) Quantitative data analysis with SPSS12 and 13. A guide for social scientists, East Sussex
Kline RB (2010) Principles and practice of structural equation modeling, 3rd edn: Guilford press
Hu LT, Benlter PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Eq Model 6(1):1–55
Sobel ME (1982) Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol 13:290–312
Lindgren KP, Parkhill MR, George WH, Hendershot CS (2008) Gender difference in perceptions of sexual intent: a qualitative review and integration. Psychol Women Q 32(4):423–439
Budweiser S, Enderlein S, Jörres RA, Hitzl AP, Wieland WF, Pfeifer M, Arzt M (2009) Sleep apnea is an independent correlate of erectile and sexual dysfunction. J Sex Med 6:3147–3157
Teloken PE, Smith EB, Lodowsky C, Freedom T, Mulhall JP (2006) Defining association between sleep apnea syndrome and erectile dysfunction. Urology 67(5):1033–1037
Waite LJ, Joyner K (2001) Emotional satisfaction and physical pleasure in sexual unions: time horizon, sexual behaviour, and sexual exclusivity. J Marriage Fam 63(1):247–264
Sajkov D, Wang T, Saunders NA, Bune AJ, Mcevoy RD (2002) Continuous positive airway pressure treatment improves pulmonary hemodynamics in patients with obstructive sleep apnea. Am J Respir Crit Care Med 165(2):152–158
Fletcher EC (2003) Sympathetic over activity in etiology of hypertension of obstructive sleep apnea. Sleep 26(1):15–19
Fanfulla F, Malaguti S, Montaga T, Salvini S, Bruschi C, Crotti P, Casale R, Rampulla C (2000) Erectile dysfunction in men with obstructive sleep apnea: an early sign of nerve involvement. Sleep 23:775–781
Mayer P, Dematteis M, Pepin JL, Wuyam B, Veale D, Vila A, Levy P (1999) Peripheral neuropathy in sleep apnea: a tissue marker o the severity of nocturnal desaturation. Am J Respir Crit Care Med 159(1):213–219
Ye L, Pack AI, Maislin G, Dinges D, Hurley S, Mccloskey S, Weaver TE (2012) Predictors of continuous positive airway pressure use during the first week of treatment. J Sleep Res 21:419–426
Lai AY, Fong DY, Lam JC, Weaver TE, Ip MS (2014) The efficacy of a brief motivational enhancement education program on continuous positive airway pressure adherence in obstructive sleep apnea: a randomized controlled trial. Chest 146(3):600–610
Acknowledgments
The authors would like to give special thanks to Ms. Michelle Cheong for her technical support in CPAP mask fitting and machine issuing and to Ms. Kaiser Sung, Ms. Eppie Sin, Ms. Po-Yee Chu, and the staff of Ho Ting Sik Sleep Disorders Centre, Queen Mary Hospital, for data collection. This study was supported by a grant award from the Health Services Research Committee, Hong Kong.
Conflict of interest
This was not an industry-supported study. Dr. Ip has received honoraria from Philips Respironics, Inc. for a lecture in Worldsleep 2011 and a lecture at Kyoto University in 2011. Dr. Weaver is the member of the board of directors of ViMedicus, Inc. She has received research support from TEVA, Inc. and has received equipment for her research from Philips Respironics, Inc. She has been a consultant for Apnex Medical, Inc, and has received royalty fees for use of the Functional Outcomes of Sleep Questionnaire from Nova Som, Apnex Medical, Inc., GlaxoSmithKline, Philips Respironics, Inc., Cephalon, Inc., and Nova Nordsk. Dr. Lam has been sponsored to attend Worldsleep conference 2011, World Congress of Sleep Apnea 2012, Sleep and Breathing conference 2013 by ResMed, Philips Respironics, Inc., and Homecare Medical Ltd., respectively. Dr Lai has been sponsored to attend the Sleep and Breathing conference 2013 and 18th Congress of the Asian Pacific Society of Respirology by ResMed and Philips Respironics, Inc., respectively. Dr. Fong indicated no financial conflicts of interests.
Compliance with ethical standards
All procedures performed in this study involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards
Author contributions
Dr. Lai has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Lai contributed to the study concept and design; acquisition, analysis, and interpretation of data; and drafting and critical revision of the manuscript for important intellectual content. Dr Ip contributed to the study concept and design, interpretation of data, critical revision of the manuscript for important intellectual content, and administrative support. Dr. Weaver contributed to the interpretation of data and critical revision of the manuscript for important intellectual content. Dr. Lam contributed to the study concept and design, interpretation of data, critical revision of the manuscript for important intellectual content, and administrative support. Dr. Fong contributed to the study concept and design, interpretation of data, and critical revision of the manuscript for important intellectual content.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lai, A.Y.K., Ip, M.S.M., Lam, J.C.M. et al. A pathway underlying the impact of CPAP adherence on intimate relationship with bed partner in men with obstructive sleep apnea. Sleep Breath 20, 543–551 (2016). https://doi.org/10.1007/s11325-015-1235-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-015-1235-6