Abstract
Introduction
Obstructive sleep apnea (OSA) is influenced by sleep architecture with rapid eye movement (REM) sleep having the most adverse influence, especially in women. There is little data defining the influence of slow-wave sleep (SWS) on OSA. We wished to study the influence of SWS on OSA and identify differences attributable to gender and/or age, if any.
Methods
Retrospective study of polysomnography (PSG) records of adult patients referred for diagnostic PSG. Records were excluded if they underwent split night or positive airway pressure titration studies, had <180 min of total sleep time (TST) and/or <40% sleep efficiency, or had SWS <5 min and/or <1% of TST. The apnea–hypopnea index (AHI) recorded during SWS was compared with that measured during other non-rapid eye movement (NREM) sleep and during REM sleep. The REM–SWS difference in AHI was measured, and compared between genders.
Results
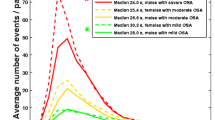
Records from 239 patients were included. The mean AHI in all subjects was 17.7 ± 22.6. The SWS AHI was 6.8 ± 18.9, compared to the REM AHI of 24.9 ± 25.8, and NREM AHI of 15.8 ± 22.8. Females had significantly higher SWS by percentage, and lower NREM AHI (P < 0.0001) and SWS AHI (P = 0.03). Among patients with OSA (AHI ≥5), the difference between REM AHI and SWS AHI was greater in women than in men (34.2 ± 27.4 vs. 21.6 ± 26.0, P = 0.006).
Conclusions
The upper airway appears to be less susceptible to OSA during SWS than during REM and other NREM sleep. This may be related to phase-specific influences on both dynamic upper airway control as well as loop gain. Gender and age appear to modify this effect.



Similar content being viewed by others
References
Remmers JE, de Groot WJ, Sauerland EK, Anch AM (1978) Pathogenesis of upper airway occlusion during sleep. J Appl Physiol 44:931–938
Guilleminault C, Partinen M, Quera-Salva M, Hayes B, Dement WC, Nino-Murcia G (1988) Determinants of daytime sleepiness in obstructive sleep apnea. Chest 94:32–37
White DP (2005) Pathogenesis of obstructive and central sleep apnea. Am J Respir Crit Care Med 172:1363–1370
Krieger J, Kurtz D (1978) EEG changes before and after apnea. In: Guilleminault C, Dement WC (eds) Sleep apneas syndromes. Alan R. Liss, New York, pp 161–176
Guchu R, Findlay LJ, Woodson H, Fabrizio M, Suratt PM (1991) Upper airway stability is increased during slow wave sleep in obstructive sleep apnea [abstract]. Am Rev Respir Dis 143:A796
Pickett CK, Regensteiner JG, Woodard WD, Hagerman DD, Weil JV, Moore LG (1989) Progesterone and estrogen reduce sleep-disordered breathing in postmenopausal women. J Appl Physiol 66:1656–1661
Polo-Kantola P, Rauhala E, Helenius H, Erkkola R, Irjala K, Polo O (2003) Breathing during sleep in menopause: a randomized, controlled, crossover trial with estrogen therapy. Obstet Gynecol 102:68–75
Rechschaffen A, Kales A (1968) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Washington Public Health Service, US Government Printing Office, Washington, DC
AASM Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22:667–689
Ratnavadivel R, Chau N, Stadler D, Yeo A, McEvoy RD, Catcheside PG (2009) Marked reduction in obstructive sleep apnea severity in slow wave sleep. J Clin Sleep Med 5:519–524
Goh DY, Galster P, Marcus CL (2000) Sleep architecture and respiratory disturbances in children with obstructive sleep apnea. Am J Respir Crit Care Med 162:682–686
Basner RC, Ringler J, Schwartzstein RM, Weinberger SE, Weiss JW (1991) Phasic electromyographic activity of the genioglossus increases in normals during slow-wave sleep. Respir Physiol 83:189–200
Le Bon O, Hoffmann G, Tecco J, Staner L, Noseda A, Pelc I, Linkowski P (2000) Mild to moderate sleep respiratory events: one negative night may not be enough. Chest 118:353–359
Boudewyns A, Van de Heyning PH, De Backer WA (1997) Site of upper airway obstruction in obstructive apnoea and influence of sleep stage. Eur Respir J 10:2566–2572
Horner RL (1996) Motor control of the pharyngeal musculature and implications for the pathogenesis of obstructive sleep apnea. Sleep 19:827–853
Penzel T, Möller M, Becker HF, Knaack L, Peter JH (2001) Effect of sleep position and sleep stage on the collapsibility of the upper airways in patients with sleep apnea. Sleep 24:90–95
Ratnavadivel R, Stadler D, Windler S, Bradley J, Paul D, McEvoy RD, Catcheside PG (2010) Upper airway function and arousability to ventilatory challenge in slow wave sleep versus stage 2 sleep in obstructive sleep apnoea. Thorax 65:107–112
Saboisky J, Eckert D, Malhotra A (2010) Stable breathing though deeper sleeping. Thorax 65:95–96
Eckert DJ, Owens RL, Kehlmann GB, Wellman A, Rahangdale S, Yim-Yeh S, White DP, Malhotra A (2011) Eszopiclone increases the respiratory arousal threshold and lowers the apnoea/hypopnea index in obstructive sleep apnea patients with a low arousal threshold. Clin Sci 120:505–514
Wellman A, Jordan AS, Malhotra A, Fogel RB, Katz ES, Schory K, Edwards JK, White DP (2004) Ventilatory control and airway anatomy in obstructive sleep apnea. Am J Respir Crit Care Med 170:1225–1232
Fukuda N, Honma H, Kohsaka M, Kobayashi R, Sakakibara S, Kohsaka S, Koyama T (1999) Gender differences of slow wave sleep in middle aged and elderly subjects. Psychiatry Clin Neurosci 53:151–153
Ehlers CL, Kupfer DJ (1997) Slow-wave sleep: do young adult men and women age differently? J Sleep Res 6:211–215
Koo BB, Dostal J, Ioachimescu O, Budur K (2008) The effects of gender and age on REM-related sleep-disordered breathing. Sleep Breath 12:259–264
Van Cauter E, Leproult R, Plat L (2000) Age-related changes in slow-wave sleep and REM sleep and relationship with growth hormone and cortisol levels in healthy men. JAMA 284:861–868
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Subramanian, S., Hesselbacher, S., Mattewal, A. et al. Gender and age influence the effects of slow-wave sleep on respiration in patients with obstructive sleep apnea. Sleep Breath 17, 51–56 (2013). https://doi.org/10.1007/s11325-011-0644-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-011-0644-4