Abstract
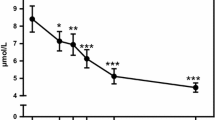
The development of assessment techniques with immediate clinical applicability is a priority for resolving the growing epidemic in metabolic disease. Many imbalances in diet-dependent metabolism are not detectable in the fasted state. Resolving the high inter-individual variability in response to diet requires the development of techniques that can detect metabolic dysfunction at the level of the individual. The intra- and inter-individual variation in lipid metabolism in response to a standardized test meal was determined. Following an overnight fast on three different days, three healthy subjects consumed a test meal containing 40% of their daily calories. Plasma samples were collected at fasting, and 1, 3, 6, and 8 h after the test meal. Plasma fatty acid (FA) concentrations within separated lipid classes and lipoprotein fractions were measured at each time point. The intra-individual variation within each subject across three days was lower than the inter-individual differences among the three subjects for over 50% of metabolites in the triacylglycerol (TG), FA, and phosphatidylcholine (PC) lipid classes at 6 h, and for 25–50% of metabolites across lipid classes at 0, 1, 3, and 8 h. The consistency of response within individuals was visualized by principal component analysis (PCA) and confirmed by ANOVA. Three representative metabolites that discriminated among the three individuals in the apolipoprotein B (ApoB) fraction, TG16:1n7, TG18:2n6, and PC18:3n3, are discussed in detail. The postprandial responses of individuals were unique within metabolites that were individual discriminators (ID) of metabolic phenotype. This study shows that the targeted metabolomic measurement of individual metabolic phenotype in response to a specially formulated lipid challenge is possible even without lead-in periods, dietary and lifestyle control, or intervention over a 3-month period in healthy free-living individuals.





Similar content being viewed by others
Abbreviations
- FA:
-
Fatty acid
- TG:
-
Triacylglycerol
- ApoB:
-
Apolipoprotein B
- ApoA:
-
Apolipoprotein A
- PC:
-
Phosphatidylcholine
- PE:
-
Phosphatidylethanolamine
- CE:
-
Cholesterol ester
- DG:
-
Diacylglycerol
- PCA:
-
Principal component analysis
- ID:
-
Individual discriminators
- BMI:
-
Body mass index
- MUFA:
-
Monounsaturated fatty acid
- PUFA:
-
Polyunsaturated fatty acid
References
Berry, S. E., Miller, G. J., & Sanders, T. A. (2007). The solid fat content of stearic acid-rich fats determines their postprandial effects. The American Journal of Clinical Nutrition, 85(6), 1486–1494.
Blackburn, P., Cote, M., Lamarche, B., et al. (2003a). Impact of postprandial variation in triglyceridemia on low-density lipoprotein particle size. Metabolism: Clinical and Experimental, 52(11), 1379–1386. doi:10.1016/S0026-0495(03)00315-9.
Blackburn, P., Lamarche, B., Couillard, C., et al. (2003b). Contribution of visceral adiposity to the exaggerated postprandial lipemia of men with impaired glucose tolerance. Diabetes Care, 26(12), 3303–3309. doi:10.2337/diacare.26.12.3303.
Burdge, G. C., Jones, A. E., Frye, S. M., Goodson, L., & Wootton, S. A. (2003). Effect of meal sequence on postprandial lipid, glucose and insulin responses in young men. European Journal of Clinical Nutrition, 57(12), 1536–1544. doi:10.1038/sj.ejcn.1601722.
Cassader, M., Gambino, R., Musso, G., et al. (2001). Postprandial triglyceride-rich lipoprotein metabolism and insulin sensitivity in nonalcoholic steatohepatitis patients. Lipids, 36(10), 1117–1124. doi:10.1007/s11745-001-0822-5.
Chong, M. F., Fielding, B. A., & Frayn, K. N. (2007). Mechanisms for the acute effect of fructose on postprandial lipemia. The American Journal of Clinical Nutrition, 85(6), 1511–1520.
Chung, B. H., Cho, B. H., Liang, P., et al. (2004). Contribution of postprandial lipemia to the dietary fat-mediated changes in endogenous lipoprotein–cholesterol concentrations in humans. The American Journal of Clinical Nutrition, 80(5), 1145–1158.
Cohn, J. S., Johnson, E. J., Millar, J. S., et al. (1993). Contribution of apoB-48 and apoB-100 triglyceride-rich lipoproteins (TRL) to postprandial increases in the plasma concentration of TRL triglycerides and retinyl esters. Journal of Lipid Research, 34(12), 2033–2040.
Cohn, J. S., McNamara, J. R., Krasinski, S. D., Russell, R. M., & Schaefer, E. J. (1989). Role of triglyceride-rich lipoproteins from the liver and intestine in the etiology of postprandial peaks in plasma triglyceride concentration. Metabolism: Clinical and Experimental, 38(5), 484–490. doi:10.1016/0026-0495(89)90203-5.
Demacker, P. N., Hessels, M., Toenhake-Dijkstra, H., & Baadenhuijsen, H. (1997). Precipitation methods for high-density lipoprotein cholesterol measurement compared, and final evaluation under routine operating conditions of a method with a low sample-to-reagent ratio. Clinical Chemistry, 43(4), 663–668.
Diraison, F., Moulin, P., & Beylot, M. (2003). Contribution of hepatic de novo lipogenesis and reesterification of plasma non esterified fatty acids to plasma triglyceride synthesis during non-alcoholic fatty liver disease. Diabetes & Metabolism, 29(5), 478–485. doi:10.1016/S1262-3636(07)70061-7.
Fielding, B. A., Callow, J., Owen, R. M., Samra, J. S., Matthews, D. R., & Frayn, K. N. (1996). Postprandial lipemia: The origin of an early peak studied by specific dietary fatty acid intake during sequential meals. The American Journal of Clinical Nutrition, 63(1), 36–41.
Folch, J., Lees, M., & Sloane Stanley, G. H. (1957). A simple method for the isolation and purification of total lipides from animal tissues. The Journal of Biological Chemistry, 226(1), 497–509.
Fuentes, F., Lopez-Miranda, J., Perez-Martinez, P., et al. (2008). Chronic effects of a high-fat diet enriched with virgin olive oil and a low-fat diet enriched with alpha-linolenic acid on postprandial endothelial function in healthy men. The British Journal of Nutrition, 100(1), 159–165. doi:10.1017/S0007114508888708.
Fusconi, E., Pala, V., Riboli, E., et al. (2003). Relationship between plasma fatty acid composition and diet over previous years in the Italian centers of the European Prospective Investigation into Cancer and Nutrition (EPIC). Tumori, 89(6), 624–635.
German, J. B., Bauman, D. E., Burrin, D. G., et al. (2004). Metabolomics in the opening decade of the 21st century: Building the roads to individualized health. The Journal of Nutrition, 134(10), 2729–2732.
German, J. B., Roberts, M. A., & Watkins, S. M. (2003). Personal metabolomics as a next generation nutritional assessment. The Journal of Nutrition, 133(12), 4260–4266.
Hennig, B., Toborek, M., & McClain, C. J. (2001). High-energy diets, fatty acids and endothelial cell function: Implications for atherosclerosis. Journal of the American College of Nutrition, 20(2, Suppl), 97–105.
Higashi, K., Shige, H., Ito, T., et al. (2001). Effect of a low-fat diet enriched with oleic acid on postprandial lipemia in patients with type 2 diabetes mellitus. Lipids, 36(1), 1–6. doi:10.1007/s11745-001-0660-5.
Hyson, D. A., Paglieroni, T. G., Wun, T., & Rutledge, J. C. (2002). Postprandial lipemia is associated with platelet and monocyte activation and increased monocyte cytokine expression in normolipemic men. Clinical and Applied Thrombosis/Hemostasis, 8(2), 147–155. doi:10.1177/107602960200800211.
Karpe, F. (1997). Postprandial lipid metabolism in relation to coronary heart disease. The Proceedings of the Nutrition Society, 56(2), 671–678. doi:10.1079/PNS19970067.
Katan, M. B., Deslypere, J. P., van Birgelen, A. P., Penders, M., & Zegwaard, M. (1997). Kinetics of the incorporation of dietary fatty acids into serum cholesteryl esters, erythrocyte membranes, and adipose tissue: An 18-month controlled study. Journal of Lipid Research, 38(10), 2012–2022.
Keith, D. S., Nichols, G. A., Gullion, C. M., Brown, J. B., & Smith, D. H. (2004). Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Archives of Internal Medicine, 164(6), 659–663. doi:10.1001/archinte.164.6.659.
Krajcovicova-Kudlackova, M., Simoncic, R., Bederova, A., Grancicova, E., & Magalova, T. (1997a). Influence of vegetarian and mixed nutrition on selected haematological and biochemical parameters in children. Die Nahrung, 41(5), 311–314. doi:10.1002/food.19970410513.
Krajcovicova-Kudlackova, M., Simoncic, R., Klvanova, J., Bederova, A., Babinska, K., & Grancicova, E. (1997b). The plasma profile of fatty acids in vegetarians. Bratislavské Lekárske Listy (Tlacené Vydanie), 98(1), 23–27.
Lemay, D., Zivkovic, A. M., & German, J. B. (2007). Building the bridges to bioinformatics in nutrition research. The American Journal of Clinical Nutrition, 86, 1261–1269.
Li, Z., Otvos, J. D., Lamon-Fava, S., et al. (2003). Men and women differ in lipoprotein response to dietary saturated fat and cholesterol restriction. The Journal of Nutrition, 133(11), 3428–3433.
Lichtenstein, A. H., Ausman, L. M., Carrasco, W., et al. (1993). Effects of canola, corn, and olive oils on fasting and postprandial plasma lipoproteins in humans as part of a National Cholesterol Education Program Step 2 diet. Arteriosclerosis and Thrombosis, 13(10), 1533–1542.
Murphy, M. C., Chapman, C., Lovegrove, J. A., et al. (1996). Meal frequency; does it determine postprandial lipaemia? European Journal of Clinical Nutrition, 50(8), 491–497.
Nicolaiew, N., Lemort, N., Adorni, L., et al. (1998). Comparison between extra virgin olive oil and oleic acid rich sunflower oil: Effects on postprandial lipemia and LDL susceptibility to oxidation. Annals of Nutrition and Metabolism, 42(5), 251–260. doi:10.1159/000012741.
Ordovas, J. M., Corella, D., Cupples, L. A., et al. (2002). Polyunsaturated fatty acids modulate the effects of the APOA1 G-A polymorphism on HDL–cholesterol concentrations in a sex-specific manner: The Framingham Study. The American Journal of Clinical Nutrition, 75(1), 38–46.
Ordovas, J. M., & Shen, J. (2008). Gene-environment interactions and susceptibility to metabolic syndrome and other chronic diseases. Journal of Periodontology, 79(8, Suppl), 1508–1513. doi:10.1902/jop.2008.080232.
Papamichael, C. M., Karatzi, K. N., Papaioannou, T. G., et al. (2008). Acute combined effects of olive oil and wine on pressure wave reflections: Another beneficial influence of the Mediterranean diet antioxidants? Journal of Hypertension, 26(2), 223–229.
Paton, C. M., Brandauer, J., Weiss, E. P., et al. (2006). Hemostatic response to postprandial lipemia before and after exercise training. Journal of Applied Physiology, 101(1), 316–321. doi:10.1152/japplphysiol.01363.2005.
Potts, J. L., Coppack, S. W., Fisher, R. M., Humphreys, S. M., Gibbons, G. F., & Frayn, K. N. (1995). Impaired postprandial clearance of triacylglycerol-rich lipoproteins in adipose tissue in obese subjects. The American Journal of Physiology, 268(4 Pt 1), E588–E594.
Rivellese, A. A., Giacco, R., Annuzzi, G., et al. (2008). Effects of monounsaturated vs. saturated fat on postprandial lipemia and adipose tissue lipases in type 2 diabetes. Clinical Nutrition (Edinburgh, Lothian), 27(1), 133–141. doi:10.1016/j.clnu.2007.07.005.
Scaglioni, S., Veduci, E., Agostoni, C., et al. (2004). Dietary habits and plasma fatty acids levels in a population of Italian children: Is there any relationship? Prostaglandins Leukotrienes and Essential Fatty Acids, 71(2), 91–95. doi:10.1016/j.plefa.2004.01.002.
Schaefer, E. J., Audelin, M. C., McNamara, J. R., et al. (2001). Comparison of fasting and postprandial plasma lipoproteins in subjects with and without coronary heart disease. The American Journal of Cardiology, 88(10), 1129–1133. doi:10.1016/S0002-9149(01)02047-1.
Sharrett, A. R., Heiss, G., Chambless, L. E., et al. (2001). Metabolic and lifestyle determinants of postprandial lipemia differ from those of fasting triglycerides: The Atherosclerosis Risk In Communities (ARIC) study. Arteriosclerosis, Thrombosis, and Vascular Biology, 21(2), 275–281.
Siepi, D., Marchesi, S., Lupattelli, G., et al. (2002). Postprandial endothelial impairment and reduced glutathione levels in postmenopausal women. Annals of Nutrition and Metabolism, 46(1), 32–37. doi:10.1159/000046750.
Silveira, A., Karpe, F., Johnsson, H., Bauer, K. A., & Hamsten, A. (1996). In vivo demonstration in humans that large postprandial triglyceride-rich lipoproteins activate coagulation factor VII through the intrinsic coagulation pathway. Arteriosclerosis, Thrombosis, and Vascular Biology, 16(11), 1333–1339.
Silvestre, R., Kraemer, W. J., Quann, E. E., et al. (2008). Effects of exercise at different times on postprandial lipemia and endothelial function. Medicine and Science in Sports and Exercise, 40(2), 264–274.
Stampfer, M. J., Krauss, R. M., Ma, J., et al. (1996). A prospective study of triglyceride level, low-density lipoprotein particle diameter, and risk of myocardial infarction. Journal of the American Medical Association, 276(11), 882–888. doi:10.1001/jama.276.11.882.
Tegner, J., Skogsberg, J., & Bjorkegren, J. (2007). Thematic review series: Systems biology approaches to metabolic and cardiovascular disorders. Multi-organ whole-genome measurements and reverse engineering to uncover gene networks underlying complex traits. Journal of Lipid Research, 48(2), 267–277. doi:10.1194/jlr.R600030-JLR200.
Urquiaga, I., Guasch, V., Marshall, G., et al. (2004). Effect of Mediterranean and Occidental diets, and red wine, on plasma fatty acids in humans. An intervention study. Biological Research, 37(2), 253–261.
van Oostrom, A. J., Sijmonsma, T. P., Verseyden, C., et al. (2003). Postprandial recruitment of neutrophils may contribute to endothelial dysfunction. Journal of Lipid Research, 44(3), 576–583. doi:10.1194/jlr.M200419-JLR200.
Watkins, S. M., Hammock, B. D., Newman, J. W., & German, J. B. (2001). Individual metabolism should guide agriculture toward foods for improved health and nutrition. The American Journal of Clinical Nutrition, 74(3), 283–286.
Watkins, S. M., Reifsnyder, P. R., Pan, H. J., German, J. B., & Leiter, E. H. (2002). Lipid metabolome-wide effects of the PPARgamma agonist rosiglitazone. Journal of Lipid Research, 43(11), 1809–1817. doi:10.1194/jlr.M200169-JLR200.
Weiss, E. P., Arif, H., Villareal, D. T., Marzetti, E., & Holloszy, J. O. (2008). Endothelial function after high-sugar-food ingestion improves with endurance exercise performed on the previous day. The American Journal of Clinical Nutrition, 88(1), 51–57.
Westphal, S., Taneva, E., Kastner, S., et al. (2006). Endothelial dysfunction induced by postprandial lipemia is neutralized by addition of proteins to the fatty meal. Atherosclerosis, 185(2), 313–319. doi:10.1016/j.atherosclerosis.2005.06.004.
Zilversmit, D. B. (1979). Atherogenesis: A postprandial phenomenon. Circulation, 60(3), 473–485.
Acknowledgments
This work was supported by University of California at Davis Graduate Group in Nutrition Block Grant, Jastro Shields Scholarship, and Superfund Training Fellowship to A. M. Zivkovic; supported in part by the National Institute of Environmental Health Sciences (NIEHS) grant R37 ES02710, the NIEHS Superfund Basic Research Program P42 ES04699, the University of California Davis CHARGE Study, Center for Children’s Environmental Health, NIEHS grant P01 ES11269, and the University of California Discovery Program.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zivkovic, A.M., Wiest, M.M., Nguyen, U. et al. Assessing individual metabolic responsiveness to a lipid challenge using a targeted metabolomic approach. Metabolomics 5, 209–218 (2009). https://doi.org/10.1007/s11306-008-0136-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11306-008-0136-0