Abstract
Purpose
We aimed to investigate the incidence of spina bifida occulta (SBO) in patients with nocturnal enuresis (NE) and its effect on the success of behavioral interventions. We also aimed to identify predictive factors related to success of behavioral interventions.
Methods
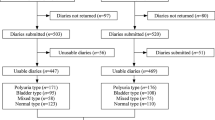
A total of 163 patients with NE and 160 patients without NE were enrolled to study. Urinalysis, urine culture, biochemical evaluation, plain radiography and urinary system ultrasonography were performed before treatment. Patients with NE received behavioral interventions for 3 months. Response to behavioral interventions was analyzed according to the presence and absence of SBO. Possible predictive factors for treatment success were also evaluated.
Results
Spina bifida occulta was detected in 47 (28.8 %) children at NE group and 24 (15.0 %) at control group (p = 0.138). Non-monosymptomatic NE was more prevalent in patients with SBO (p < 0.001), and response to the treatment was significantly lower (p = 0.037). Presence of SBO (OR 8.8, 95 % CI 3.1–25.6), NE severity (OR 7.2, 95 % CI 2.4–21.7) and NE frequency on 3-day voiding diary (OR 9.4, 95 % CI 3.7–24.3) were significantly related to the success.
Conclusions
The presence of SBO, severe NE and higher frequency of NE in voiding diary affect the response to behavioral interventions. Other treatment options such as medical treatment or enuresis alarm may be recommended for those patients.
Similar content being viewed by others
References
Nevéus T, von Gontard A, Hoebeke P et al (2006) The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children’s Continence Society. J Urol 176(1):314–324
Yazici CM, Nalbantoglu B, Topcu B, Dogan C (2012) Prevalence of nocturnal enuresis and associated factors in schoolchildren in Western Turkey. Can J Urol 19(4):6383–6388
Oge O, Koçak I, Gemalmaz H (2001) Enuresis: point prevalence and associated factors among Turkish children. Turk J Pediatr 43(1):38–43
Serel TA, Akhan G, Koyuncuoglu HR et al (1997) Epidemiology of enuresis in Turkish children. Scand J Urol Nephrol 31(6):537–539
Eubanks JD, Cheruvu VK (2009) Prevalence of sacral spina bifida occulta and its relationship to age, sex, race, and the sacral table angle: an anatomic, osteologic study of three thousand one hundred specimens. Spine (Phila Pa 1976) 34(15):1539–1543
Fidas A, MacDonald HL, Elton RA, Wild SR, Chisholm GD, Scott R (1987) Prevalence and patterns of spina bifida occulta in 2707 normal adults. Clin Radiol 38(5):537–542
Solomon LB, Rühli FJ, Lee YC, Henneberg M (2009) Secular trend in the opening of the sacral canal: an Australian study. Spine (Phila Pa 1976) 34(3):244–248
Gregerson DM (1997) Clinical consequences of spina bifida occulta. J Manipulative Physiol Ther 20(8):546–550
Miyazato M, Sugaya K, Nishijima S, Owan T, Ogawa Y (2007) Location of spina bifida occulta and ultrasonographic bladder abnormalities predict the outcome of treatment for primary nocturnal enuresis in children. Int J Urol 14(1):33–38
Ritchey ML, Sinha A, DiPietro MA, Huang C, Flood H, Bloom DA (1994) Significance of spina bifida occulta in children with diurnal enuresis. J Urol 152(2 Pt 2):815–818
Galloway NT, Tainsh J (1985) Minor defects of the sacrum and neurogenic bladder dysfunction. Br J Urol 57(2):154–155
Morison MJ (1998) Parents’ and young people’s attitudes towards bedwetting and their influence on behaviour, including readiness to engage in and persist with treatment. Br J Urol 81(Suppl 3):56–66
Redsell SA, Collier J (2001) Bedwetting, behaviour and self-esteem: a review of the literature. Child Care Health Dev 27(2):149–162
Theunis M, Van Hoecke E, Paesbrugge S, Hoebeke P, Vande Walle J (2002) Self-image and performance in children with nocturnal enuresis. Eur Urol 41(6):660–667 (discussion 667)
Caldwell PH, Nankivell G, Sureshkumar P (2013) Simple behavioural interventions for nocturnal enuresis in children. Cochrane Database Syst Rev 7:CD003637
El-Anany FG, Maghraby HA, Shaker SE, Abdel-Moneim AM (1999) Primary nocturnal enuresis: a new approach to conditioning treatment. Urology 53(2):405–408 (discussion 408-9)
Atala A, Bauer SB, Dyro FM et al (1992) Bladder functional changes resulting from lipomyelomeningocele repair. J Urol 148(2 Pt 2):592–594
Forsythe WI, Redmond A (1974) Enuresis and spontaneous cure rate. Study of 1129 enuretis. Arch Dis Child 49(4):259–263
Shin SH, Im YJ, Lee MJ, Lee YS, Choi EK, Han SW (2013) Spina bifida occulta: not to be overlooked in children with nocturnal enuresis. Int J Urol 20(8):831–835
Djurhuus JC, Nørgaard JP, Rittig S (1992) Monosymptomatic bedwetting. Scand J Urol Nephrol Suppl 141:7–17 (discussion 18-9)
Hjalmas K, Arnold T, Bower W et al (2004) Nocturnal enuresis: an international evidence based management strategy. J Urol 171(6 Pt 2):2545–2561
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest in this paper. There was no funding for this manuscript.
Rights and permissions
About this article
Cite this article
Kurt, O., Yazici, C.M. & Paketci, C. Nocturnal enuresis with spina bifida occulta: Does it interfere behavioral management success?. Int Urol Nephrol 47, 1485–1491 (2015). https://doi.org/10.1007/s11255-015-1047-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-1047-4