Abstract
Purpose
Diabetic retinopathy (DR) is an important, chronic complication of diabetes, requiring competent self-management that depends on adherence to behavioral regimens. This study attempted to identify factors influencing self-management behaviors and develop a model illustrating the interdependence of several factors associated with DR patients.
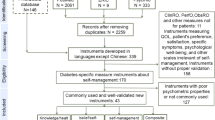
Methods
In June–December 2012, 368 patients with DR completed questionnaires assessing self-management behavior, diabetes knowledge, health beliefs, social support, and treatment adherence. Structural equation modeling was used to test predicted pathways linking self-management behavior to diabetes knowledge, health beliefs, social support, and treatment adherence.
Results
The results indicated that health beliefs, treatment adherence, and duration of diabetes each had a direct impact on diabetes self-management (p < 0.05). Diabetes knowledge only indirectly influenced diabetes self-management, through health beliefs. Social support had a direct impact on diabetes self-management (β = 0.35, p < 0.01), and an indirect influence on diabetes self-management, through treatment adherence (β = 0.77, p < 0.01).
Conclusion
Health beliefs, treatment adherence, and social support directly affect diabetes self-management, and diabetes knowledge indirectly affects diabetes self-management. This suggests that enhancing DR patients’ health beliefs, treatment adherence, and social support would facilitate their diabetes self-management. Meanwhile, improved health education can strengthen diabetes knowledge, which in turn, can positively affect diabetes self-management.


Similar content being viewed by others
References
Nagelkerk, J., Reick, K., & Meengs, L. (2006). Perceived barriers and effective strategies to diabetes self-management. Journal of Advanced Nursing, 54(2), 151–158.
Tumosa, N. (2008). Eye disease and the older diabetic. Clinics in Geriatric Medicine, 24(3), 515–527.
Glasgow, R. E., & Anderson, R. M. (1999). In diabetes care, moving from compliance to adherence is not enough. Something entirely different is needed. Diabetes Care, 22(12), 2090–2092.
Peeples, M., Tomky, D., Mulcahy, K., Peyrot, M., & Siminerio, L. (2007). Evolution of the American Association of Diabetes Educators diabetes education outcomes project. The Diabetes Educator, 33(5), 794–817.
Sousa, V. D., Zauszniewski, J. A., Musil, C. M., Price, L. P. J., & Davis, S. A. (2005). Relationships among self-care agency, self-efficacy, self-care, and glycemic control. Research and Theory for Nursing Practice, 19(3), 217–230.
Funnell, M. M., Brown, T. L., Childs, B. P., Haas, L. B., Hosey, G. M., Jensen, B., et al. (2012). National standards for diabetes self-management education. Diabetes Care, 35(Suppl 1), S101–S108.
Patel, A., MacMahon, S., Chalmers, J., Neal, B., Billot, L., Woodward, M., et al. (2008). Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. The New England Journal of medicine, 358(24), 2560–2572.
Yu, D. S., Lee, D. T., & Woo, J. (2004). Psychometric testing of the Chinese version of the medical outcomes study social support survey (MOS-SSS-C). Research in Nursing and Health, 27(2), 135–143.
Nam, S., Chesla, C., Stotts, N. A., Kroon, L., & Janson, S. L. (2011). Barriers to diabetes management: Patient and provider factors. Diabetes Research and Clinical Practice, 93(1), 1–9.
Tang, T. S., Brown, M. B., Funnell, M. M., & Anderson, R. M. (2008). Social support, quality of life, and self-care behaviors among African Americans with type 2 diabetes. The Diabetes Educator, 34(2), 266–276.
Toljamo, M., & Hentinen, M. (2001). Adherence to self-care and social support. Journal of Clinical Nursing, 10(5), 618–627.
Albright, T. L., Parchman, M., & Burge, S. K. (2001). Predictors of self-care behavior in adults with type 2 diabetes: An RRNeST study. Family Medicine, 33(5), 354–360.
Garay-Sevilla, M. E., Nava, L. E., Malacara, J. M., Huerta, R., de Leon, J. D., Mena, A., et al. (1995). Adherence to treatment and social support in patients with non-insulin dependent diabetes mellitus. Journal of Diabetes and its Complications, 9(2), 81–86.
Chlebowy, D. O., & Garvin, B. J. (2006). Social support, self-efficacy, and outcome expectations: Impact on self-care behaviors and glycemic control in Caucasian and African American adults with type 2 diabetes. The Diabetes Educator, 32(5), 777–786.
Rodrigues, F. F., Zanetti, M. L., dos, S. M. A., Martins, T. A., Sousa, V. D., & de Sousa Teixeira, C. R. (2009). Knowledge and attitude: Important components in diabetes education. Revista Latino-Americana de Enfermagem, 17(4), 468–473.
Mazzuca, S. A. (1982). Does patient education in chronic disease have therapeutic value. Journal of Chronic Diseases, 35(7), 521–529.
Harvey, J. N., & Lawson, V. L. (2009). The importance of health belief models in determining self-care behaviour in diabetes. Diabetic Medicine: A Journal of the British Diabetic Association, 26(1), 5–13.
Brownlee-Duffeck, M., Peterson, L., Simonds, J. F., Goldstein, D., Kilo, C., & Hoette, S. (1987). The role of health beliefs in the regimen adherence and metabolic control of adolescents and adults with diabetes mellitus. Journal of Consulting and Clinical Psychology, 55(2), 139–144.
Gillibrand, R., & Stevenson, J. (2006). The extended health belief model applied to the experience of diabetes in young people. British Journal of Health Psychology, 11(Pt 1), 155–169.
Zimet, G. D., Powell, S. S., Farley, G. K., Werkman, S., & Berkoff, K. A. (1990). Psychometric characteristics of the multidimensional scale of perceived social support. Journal of Personality Assessment, 55(3–4), 610–617.
Guan, N. C., Huai, S. L., Hway, A. A. Y., & Ong, H. K. (2015). Factorial validity and reliability of the malaysian simplified chinese version of multidimensional scale of perceived social support (MSPSS-SCV) among a group of university students. Asia-Pacific Journal of Public Health, 27(2), 225–231.
Toobert, D. J., Hampson, S. E., & Glasgow, R. E. (2000). The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care, 23(7), 943–950.
Wang, R. H., & Lin, C. C. (1998). Self-care behaviors and related factors in outpatients newly diagnosed with non-Insulin dependent. The Journal of Nursing (in Chinese), 4(5), 60–74.
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55.
Hamta, A., Khalilian, A. R., Farhadi, R., & Ranjbaran, H. (2013). Path analysis of the risk of low birth weight for multipara. Iranian Red Crescent Medical Journal, 15(6), 462–466.
Gallant, M. P. (2003). The influence of social support on chronic illness self-management: A review and directions for research. Health Education and Behavior: The Official Publication of the Society for Public Health Education, 30(2), 170–195.
Rosland, A. M., Kieffer, E., Israel, B., Cofield, M., Palmisano, G., Sinco, B., et al. (2008). When is social support important? The association of family support and professional support with specific diabetes self-management behaviors. Journal of General Internal Medicine, 23(12), 1992–1999.
Mayberry, L. S., & Osborn, C. Y. (2012). Family support, medication adherence, and glycemic control among adults with type 2 diabetes. Diabetes Care, 35(6), 1239–1245.
Xu, Y., Toobert, D., Savage, C., Pan, W., & Whitmer, K. (2008). Factors influencing diabetes self-management in Chinese people with type 2 diabetes. Research in Nursing and Health, 31(6), 613–625.
Chan, Y. M., & Molassiotis, A. (1999). The relationship between diabetes knowledge and compliance among Chinese with non-insulin dependent diabetes mellitus in Hong Kong. Journal of Advanced Nursing, 30(2), 431–438.
Acknowledgments
We would like to thank all study participants, and the doctors and nurses from the Jianhua community clinics in Qiqihar city for their considerable assistance.
Funding
This study was funded by the Ministry of Education of Heilongjiang province (Grant Number 12541377).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Li Yang, Yu Cui, and Libo Liang contributed equally to this article.
Rights and permissions
About this article
Cite this article
Yang, L., Wu, Q., Hao, Y. et al. Self-management behavior among patients with diabetic retinopathy in the community: a structural equation model. Qual Life Res 26, 359–366 (2017). https://doi.org/10.1007/s11136-016-1396-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-016-1396-1