Abstract
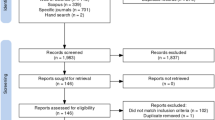
Background Clinical and cost-effectiveness evidence are needed to justify the existence or extension of routine clinical pharmacy services in hospital settings. Previous reviews have indicated that clinical pharmacist interventions are likely to have a positive economic impact on hospital budgets but highlighted issues relating to the quality of studies. Aim of the review The primary aim of this review was to feature economic evaluations of clinical pharmacy services which targeted hospital inpatients. The review focused on the current cost-effectiveness status of different services, in addition to evaluating the quality of individual studies. Results of this systematic review were compared with cost-effectiveness and quality related findings of reviews which considered earlier time frames and alternative settings. Methods A systematic review of the literature included a review of the following databases: Academic Search Complete, Cochrane Library, EconLit, Embase Elsevier, NHS Economic Evaluation Database and PubMed. Only studies with an economic assessment of a clinical pharmacy service provided in a hospital setting were included. Data relating to the cost-effectiveness was extracted from eligible studies. Methodologies employed and overall quality of the studies was also reviewed. A grading system was applied to determine the quality of studies. Consolidated Health Economic Evaluation Reporting Standards statement was employed to determine which aspects of a high quality health economic study were employed. Results Twenty studies were deemed eligible for inclusion. Overall, pharmacist interventions had a positive impact on hospital budgets. Only three studies (15 %) were deemed to be “good-quality” studies. No ‘novel’clinical pharmacist intervention was identified during the course of this review. Conclusions Clinical pharmacy interventions continue to provide cost savings. However, the standard of studies published has stagnated or even deteriorated in comparison with those included in previous reviews. Utilisation of published guidelines at initial stages of future studies may help improve the overall quality of studies.

Similar content being viewed by others
References
Kaboli PJ, Hoth AB, McClimon BJ, Schnipper JL. Clinical pharmacists and inpatient medical care: a systematic review. Arch Intern Med. 2006;166(9):955–64.
Kopp BJ, Mrsan M, Erstad BL, Duby JJ. Cost implications of and potential adverse events prevented by interventions of a critical care pharmacist. Am J Health Syst Pharm. 2007;64(23):2483–7.
Lada P, Delgado G Jr. Documentation of pharmacists’ interventions in an emergency department and associated cost avoidance. Am J Health Syst Pharm. 2007;64(1):63–8.
Olson LM, Desai S, Soto ML, Namazifard S, Quelland AK, Erstad BL. Evaluation of pharmacists’ interventions at a university teaching hospital. Can J Hosp Pharm. 2005;58(1):20–5.
Alderman CP, Farmer C. A brief analysis of clinical pharmacy interventions undertaken in an Australian teaching hospital. J Qual Clin Pract. 2001;21(4):99–103.
Marriott JL, Nation RL, Roller L, Costelloe M, Galbraith K, Stewart P, et al. Pharmacy education in the context of Australian practice. Am J Pharm Educ. 2008;72(6):131.
Sosabowski MH, Gard PR. Pharmacy education in the United Kingdom. Am J Pharm Educ. 2008;72(6):130.
Pickard AS, Hung SY. An update on evidence of clinical pharmacy services’ impact on health-related quality of life. Ann Pharmacother. 2006;40(9):1623–34.
Zellmer WA. Pharmacy’s future: transformation, diffusion, and imagination. Am J Health Syst Pharm. 2010;67(14):1199–204.
Anderson SV, Schumock GT. Evaluation and justification of clinical pharmacy services. Expert Rev Pharmacoecon Outcomes Res. 2009;9(6):539–45.
De Rijdt T, Willems L, Simoens S. Economic effects of clinical pharmacy interventions: a literature review. Am J Health Syst Pharm. 2008;65(12):1161–72.
Perez A, Doloresco F, Hoffman JM, Meek PD, Touchette DR, Vermeulen LC, et al. Economic evaluations of clinical pharmacy services: 2001–2005. Pharmacotherapy. 2009;29(1):128.
Touchette DR, Doloresco F, Suda KJ, Perez A, Turner S, Jalundhwala Y, et al. Economic evaluations of clinical pharmacy services: 2006–2010. Pharmacotherapy. 2014;34(8):771–93.
Chisholm-Burns MA, Zivin JSG, Lee JK, Spivey CA, Slack M, Herrier RN, et al. Economic effects of pharmacists on health outcomes in the United States: a systematic review. Am J Health Syst Pharm. 2010;67(19/20):1624–34.
American College of Clinical Pharmacy. The definition of clinical pharmacy. Pharmacotherapy. 2008;28(6):816–7.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS) statement. Value in Health. 2013;6(2):e1–5.
Magedanz L, Silliprandi EM, dos Santos RP. Impact of the pharmacist on a multidisciplinary team in an antimicrobial stewardship program: a quasi-experimental study. Int J Clin Pharm. 2012;34(2):290–4.
Dunn K, O’Reilly A, Silke B, Rogers T, Bergin C. Implementing a pharmacist-led sequential antimicrobial therapy strategy: a controlled before-and-after study. Int J Clin Pharm. 2011;33(2):208–14.
Shen J, Sun Q, Zhou X, Wei Y, Qi Y, Zhu J, et al. Pharmacist interventions on antibiotic use in inpatients with respiratory tract infections in a Chinese hospital. Int J Clin Pharm. 2011;33(6):929–33.
Steinberg JG, Machado C, Clarke H, Marsh WA, Kelly G. Impact of pharmacy-generated recommendations on antibiotic therapy in a community hospital. Hosp Pharm. 2008;43(12):988–93.
Ijo I, Feyerharm J. Pharmacy intervention on antimicrobial management of critically ill patients. Pharm Pract. 2011;9(2):106–9.
Yen YH, Chen HY, Wuan-Jin L, Lin YM, Shen WC, Cheng KJ. Clinical and economic impact of a pharmacist-managed i.v.-to-p.o. conversion service for levofloxacin in Taiwan. Int J Clin Pharmacol Ther. 2012;50(2):136–41.
Winger BJ, Clements EA, DeYoung JL, O’Rourke TJ, Claypool DL, Vachon S, et al. Cost savings from dose rounding of biologic anticancer agents in adults. J Oncol Pharm Pract. 2011;17(3):246–51.
Jing YS, Lai PSM, Siew SC, Siew PC. The impact of pharmacist intervention on the use of activated vitamin D in a tertiary referral hospital in Malaysia. Int J Pharm Pract. 2009;17(5):305–11.
Nasser SC, Nassif JG, Mahfouz F. Cost reduction associated with restriction policy on dispensing intravenous esomeprazole in Lebanon. Pharm World Sci. 2010;32(6):707–10.
Chan AL, Hsieh HJ, Lin SJ. Pharmacist intervention in activated protein C therapy for severe sepsis: influence on health and economic outcomes. Int J Clin Pharmacol Ther. 2009;47(4):229–35.
Wallerstedt SM, Bladh L, Ramsberg J. A cost-effectiveness analysis of an in-hospital clinical pharmacist service. BMJ Open. 2012;2(1).
Gillespie U, Alassaad A, Henrohn D, Garmo H, Hammarlund-Udenaes M, Toss H, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894–900.
Wilkinson ST, Pal A, Couldry RJ. Impacting readmission rates and patient satisfaction: results of a discharge pharmacist pilot program. Hosp Pharm. 2011;46(11):876–83.
Moffett BS, Mott AR, Nelson DP, Gurwitch KD. Medication dosing and renal insufficiency in a pediatric cardiac intensive care unit: impact of pharmacist consultation. Pediatr Cardiol. 2008;29(4):744–8.
Zhang C, Zhang L, Huang L, Luo R, Wen J. Clinical pharmacists on medical care of pediatric inpatients: a single-center randomized controlled trial. PLoS One. 2012;7(1):e30856.
Hassan Y, Al-Ramahi RJ, Aziz NA, Ghazali R. Impact of a renal drug dosing service on dose adjustment in hospitalized patients with chronic kidney disease. Ann Pharmacother. 2009;43(10):1598–605.
Hou JY, Wang YJ, Kuo LN, Shen WC, Lee YY. Retrospective evaluation of the outcomes of applying the renal dosing monitoring system in a medical center. J Exp Clin Med. 2011;3(4):176–80.
Campbell AR, Nelson LA, Elliott E, Hieber R, Sommi RW. Analysis of cost avoidance from pharmacy students’ clinical interventions at a psychiatric hospital. Am J Pharm Educ. 2011;75(1):8.
Klopotowska JE, Kuiper R, van Kan HJ, de Pont AC, Dijkgraaf MG, Lie-A-Huen L, et al. On-ward participation of a hospital pharmacist in a Dutch intensive care unit reduces prescribing errors and related patient harm: an intervention study. Crit Care. 2010;14(5).
MacLaren R, Bond CA. Effects of pharmacist participation in intensive care units on clinical and economic outcomes of critically ill patients with thromboembolic or infarction-related events. Pharmacotherapy. 2009;29(7):761–8.
Swoboda S, Lichtenstern C, Ober MC, Taylor LA, Storzinger D, Michel A, et al. Implementation of practice guidelines for antifungal therapy in a surgical intensive care unit and its impact on use and costs. Chemotherapy. 2009;55(6):418–24.
Weant KA, Armitstead JA, Ladha AM, Sasaki-Adams D, Hadar EJ, Ewend MG. Cost effectiveness of a clinical pharmacist on a neurosurgical team. Neurosurgery. 2009;65(5):946–50.
Blanch L, Annane D, Antonelli M, Chiche JD, Cunat J, Girard TD, et al. The future of intensive care medicine. Med Intensiva. 2013;37(2):91–8.
Erstad BL. A primer on critical care pharmacy services. Ann Pharmacother. 2008;42(12):1871–81.
Stephens JM, Handke B, Doshi JA. International survey of methods used in health technology assessment (HTA): does practice meet the principles proposed for good research? Comp Eff Res. 2012;2:29–44.
Weinstein MC, Torrance G, McGuire A. QALYs: the basics. Value Health. 2009;12(Suppl 1):S5–9.
Pignone M, Saha S, Hoerger T, Lohr KN, Teutsch S, Mandelblatt J. Challenges in systematic reviews of economic analyses. Ann Intern Med. 2005;142(12 Pt 2):1073–9.
Coons SJ, Rao S, Keininger DL, Hays RD. A comparative review of generic quality-of-life instruments. PharmacoEconomics. 2000;17(1):13–35.
Versteegh MM, Leunis A, Uyl-de Groot CA, Stolk EA. Condition-specific preference-based measures: benefit or burden? Value Health. 2012;15(3):504–13.
Nord E, Daniels N, Kamlet M. QALYs: some challenges. Value Health. 2009;12(suppl):S10–S15.
Acknowledgments
The authors gratefully acknowledge the help of Professor John Browne and the UCC Graduate Studies Office for providing the module entitled, ‘Systematic Reviews for the Health Sciences.’ which notably helped with the development of this systematic review.
Funding
None.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix 1
Rights and permissions
About this article
Cite this article
Gallagher, J., McCarthy, S. & Byrne, S. Economic evaluations of clinical pharmacist interventions on hospital inpatients: a systematic review of recent literature. Int J Clin Pharm 36, 1101–1114 (2014). https://doi.org/10.1007/s11096-014-0008-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-014-0008-9