Abstract
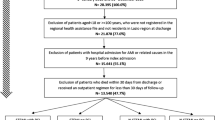
Background Secondary prevention pharmacotherapy improves outcomes after acute coronary syndrome (ACS). However, poor medication adherence is common, and various factors play a role in adherence. Objectives The purpose of this study was to evaluate patients’ level of adherence to evidence-based therapies at an average of 6 months after discharge for ACS and to identify factors associated with self-reported non-adherence. Setting This prospective study was conducted in the outpatient cardiac clinics of Hospital Pulau Pinang, located in Penang Island, a northern state in Malaysia. Method A random sample of ACS patients (n = 190) who had been discharged on a regimen of secondary preventive medications were included in this study. Six months after discharge and during their scheduled follow-up appointments to cardiac clinics, patients were interviewed using the translated eight-item Morisky Medication Adherence Scale. Main outcome measure self-reported patients’ adherence to medication. Results Six months following their hospital discharge, only 35 patients (18.4 %) reported high adherence. Medium adherence was reported in majority of patients (51.1 %). Low adherence was reported in 58 patients (30.5 %). Forgetfulness was the most frequently reported reason for patients’ non-adherence to their medications (23.2 %). Furthermore, this study identified 5 factors—namely age, employment status, ACS subtypes, number of comorbidities, and number of prescription medications per day—that may influence Patients’ level of adherence to the prescribed regimens. Conclusions Our findings revealed a problem of non-adherence to secondary prevention medications among patients with ACS in Malaysia. Furthermore, this study demonstrates that older patients, unemployed patients, patients with more comorbid conditions, and those receiving multiple medications are less likely to adhere to their prescribed medications 6 months after hospital discharge.


Similar content being viewed by others
References
Kernis SJ, Harjai KJ, Stone GW, Grines LL, Boura JA, et al. Does beta-blocker therapy improve clinical outcomes of acute myocardial infarction after successful primary angioplasty? J Am Coll Cardiol. 2004;43:1773–9.
Bhatt DL, Fox KA, Hacke W, Berger PB, Black HR, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Eng J Med. 2006;354:1706–17.
Serruys PC, de Feyter P, Macaya C, Kokott N, Puel J, et al. Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trial. J Am Med Assoc. 2002;287:3215–22.
Tea KK, Yusuf S, Pfeffer M, Kober L, Hall A, et al. Effects of long-term treatment with angiotensin-converting-enzyme inhibitors in the presence or absence of aspirin: a systematic review. Lancet. 2002;360:1037–43.
Ars F, Loma-Osorio Á, Vila J, Lpez-Bescs L, Cuat J, et al. Effect of combined beta-blocker and angiotensin-converting enzyme inhibitor treatment on 1-year survival after acute myocardial infarction: findings of the PRIAMHO-II registry. Rev Esp Cardiol. 2006;59:313–20.
Spencer FA, Lessard D, Yarzebski J, Gore JM, Goldberg RJ. Decade-long changes in the use of combination evidence-based medical therapy at discharge for patients surviving acute myocardial infarction. Am Heart J. 2005;150:838–44.
Sud A, Kline-Rogers EM, Eagle KA, Fang J, Armstrong DF, et al. Adherence to medications by patients after acute coronary syndromes. Ann Pharmacother. 2005;39:1792–7.
Kassab YW, Hassan Y, Abd Aziz N, Akram H, Ismail O. Use of evidence-based therapy for the secondary prevention of acute coronary syndromes in Malaysian practice. J Eval Clin Pract. 2012. doi:10.1111/j.1365-2753.2012.01894.x.
Al-Qasem A, Smith F, Clifford S. Adherence to medication among chronic patients in Middle Eastern countries: review of studies. East Mediterr Health J. 2011;17:356–63.
Gallagher E, Viscoli CM, Horwitz RI. The relationship of treatment adherence to the risk of death after myocardial infarction in women. J Am Med Assoc. 1993;270:742–4.
Ockene I, Hayman L, Pasternak R, Schron E, Dunbar-Jacob J. Task force #4-adherence issues and behavior changes: achieving a long-term solution. J Am Coll Cardiol. 2002;40:630–40.
Berg JS, Dischler J, Wagner DJ, Raia JJ, Palmer-Shevlin N. Medication compliance: a healthcare problem. Ann Pharmacother. 1993;27(9 suppl):S1–24.
Al-Qazaz HK, Hassali MA, Shafie AA, Sulaiman SA, Sundram S, Morisky DE. The eight-item Morisky Medication Adherence Scale MMAS: translation and validation of the Malaysian version. Diabetes Res Clin Pract. 2010;90:216–21.
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10:348–54.
Quek KF, Low WY, Razack AH, Loh CS. Reliability and validity of the International Prostate Symptom Score in a Malaysian population. Brit J Urol. 2001;88:21–5.
Hinton PR, Brownlow C, McMurray I, Cozens B. SPSS Explained. 1st ed. London: Routledge; 2004.
Eagle K, Kline-Rogers E, Goodman S, Gurfinkel E, Avezum A, et al. Adherence to evidence-based therapies after discharge for acute coronary syndromes: an ongoing prospective, observational study. Am J Med. 2004;117:73–81.
Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Non-compliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med. 2002;17:504–11.
Eagle KA, Goodman SG, Avezum Á, Budaj A, Sullivan CM, López-Sendón J. Practice variation and missed opportunities for reperfusion in ST-segment elevation myocardial infarction—findings from the global registry of acute coronary events (GRACE). Lancet. 2002;359:373–7.
Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. J Am Med Assoc. 2002;288:462–7.
Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J. Long-term persistence in use of statin therapy in elderly patients. J Am Med Assoc. 2002;288:455–61.
Cheng JWM, Kalis MM, Feifer S. Patient-reported adherence to guidelines of the sixth joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Pharmacotherapy. 2001;21:828–41.
Khanderia U, Townsend KA, Erickson SR, Vlasnik J, Prager RL, Eagle KA. Medication adherence following coronary artery bypass graft surgery: assessment of beliefs and attitudes. Ann Pharmacother. 2008;42:192–9.
Roe CM, Motheral BR, Teitelbaum F, Rich MW. Compliance with and dosing of angiotensin-converting-enzyme inhibitors before and after hospitalization. Am J Health Syst Pharm. 2000;57:139–45.
McLane CG, Zyzanski SJ, Flocke SA. Factors associated with medication noncompliance in rural elderly hypertensive patients. Am J Hypertens. 1995;8:206–9.
Acknowledgments
Special thanks to the staff of Hospital Pulau Pinang cardiology and pharmacy department for their support. This work formed part of a research project submitted as a thesis for the degree of Doctor of Philosophy in clinical pharmacy, Universiti Sains Malaysia, School of Pharmaceutical Sciences.
Funding
Funding for this project was provided by the Universiti Sains Malaysia Postgraduate research grant number (1001/PFARMASI/844055).
Conflicts of interest
None of the authors have any conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kassab, Y., Hassan, Y., Abd Aziz, N. et al. Patients’ adherence to secondary prevention pharmacotherapy after acute coronary syndromes. Int J Clin Pharm 35, 275–280 (2013). https://doi.org/10.1007/s11096-012-9735-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-012-9735-y