Abstract
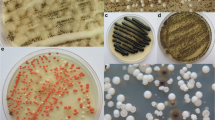
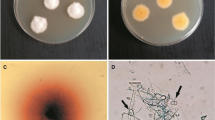
Exophiala dermatitidis is an ascomycetous black yeast from the order Chaetothyriales. Its growth characteristics include the polymorphic life cycle, ability to grow at high and low temperatures, at a wide pH range, survival at high concentrations of NaCl, and survival at high UV and radioactive radiation. Exophiala dermatitidis causes deep or localized phaeohyphomycosis in immuno-compromised people worldwide and is regularly encountered in the lungs of cystic fibrosis patients. Regardless of numerous ecological studies worldwide, little is known about its natural habitat or the possible infection routes. The present review summarizes the published data on its frequency of occurrence in nature and in man-made habitats. We additionally confirmed its presence with culture-depending methods from a variety of habitats, such as glacial meltwater, mineral water, mineral-rich salt-pan mud, dishwashers, kitchens and different environments polluted with aromatic hydrocarbons. In conclusion, the frequency of its recovery was the highest in man-made indoor habitats, connected to water sources, and exposed to occasional high temperatures and oxidative stress.

Similar content being viewed by others
References
Haase G, Sonntag L, Melzer-Krick B, de Hoog GS. Phylogenetic inference by SSU-gene analysis of members of the Herpotrichiellaceae with special reference to human pathogenic species. Stud Mycol. 1999;43:80–97.
Badali H, Najafzadeh MJ, van Esbroeck M, et al. The clinical spectrum of Exophiala jeanselmei, with a case report and in vitro antifungal susceptibility of the species. Med Mycol. 2010;48:318–27.
Badali H, Chander J, Bayat M, et al. Multiple subcutaneous cysts due to Exophiala spinifera in an immunocompetent patient. Med Mycol. 2012;50:207–13.
Morio F, Berre JY, Garcia-Hermoso D, et al. Phaeohyphomycosis due to Exophiala xenobiotica as a cause of fungal arthritis in an HIV-infected patient. Med Mycol. 2012;50:513–7.
Pattanaprichakul P, Bunyaratavej S, Leeyaphan C, et al. An unusual case of eumycetoma caused by Exophiala jeanselmei after a sea urchin injury. Mycoses. 2013;56:491–4.
Woo PC, Ngan AH, Tsang CC, et al. Clinical spectrum of Exophiala infections and a novel Exophiala species, Exophiala hongkongensis. J Clin Microbiol. 2013;51:260–7.
Najafzadeh MJ, Suh MK, Lee MH, et al. Subcutaneous phaeohyphomycosis caused by Exophiala equina, with susceptibility to eight antifungal drugs. J Med Microbiol. 2013;62:797–800.
de Hoog GS, Vicente VA, Najafzadeh MJ, et al. Waterborne Exophiala species causing disease in cold-blooded animals. Persoonia. 2011;27:46–72.
Seyedmousavi S, Badali H, Chlebicki A, et al. Exophiala sideris, a novel black yeast isolated from environments polluted with toxic alkyl benzenes and arsenic. Fungal Biol. 2011;115:1030–7.
Borman AM, Fraser M, Szekely A, Larcombe DE, Johnson EM. Rapid identification of clinically relevant members of the genus Exophiala by matrix-assisted laser desorption ionization-time of flight mass spectrometry and description of two novel species, Exophiala campbellii and Exophiala lavatrina. J Clin Microbiol. 2017;55:1162–76.
Karuppayil SM, Szaniszlo PJ. Importance of calcium to the regulation of polymorphism in Wangiella (Exophiala) dermatitidis. Med Mycol. 1997;35:379–88.
de Hoog GS, Haase G. Nutritional physiology and selective isolation of Exophiala dermatitidis. Antonie Van Leeuwenhoek. 1993;64:17–26.
Prenafeta-Boldú XF, Summerbell R, de Hoog GS. Fungi growing on aromatic hydrocarbons: biotechnology’s unexpected encounter with biohazard? FEMS Microbiol Rev. 2006;30:109–30.
Zalar P, Novak M, de Hoog GS, Gunde-Cimerman N. Dishwashers—a man-made ecological niche accommodating human opportunistic fungal pathogens. Fungal Biol. 2011;115:997–1007.
Zajc J, Džeroski S, Kocev D, et al. Chaophilic or chaotolerant fungi: a new category of extremophiles? Front Microbiol. 2014;5:1–15.
de Hoog GS, Guarro J, Gené J, Figueras MJ. Atlas of clinical fungi. 3rd ed. Centraalbureau Voor Schimmelcultures/Univeesitat Rovira I Virgili; 2009.
Zeng JS, Sutton DA, Fothergill AW, et al. Spectrum of clinically relevant Exophiala species in the United States. J Clin Microbiol. 2007;45:3713–20.
Hiruma M, Kawada A, Ohata H, et al. Systemic phaeohyphomycosis caused by Exophiala dermatitidis. Mycoses. 1993;36:1–7.
Nachman S, Alpan O, Malowitz R, Spitzer ED. Catheter-associated fungemia due to Wangiella (Exophiala) dermatitidis. J Clin Microbiol. 1996;34:1011–3.
Cohen ZY, Stead W. Exophiala pneumonia presenting with a cough productive of black sputum. Case Rep Infect Dis. 2015;2015:821049.
Kondori N, Gilljam M, Lindblad A, et al. High rate of Exophiala dermatitidis recovery in the airway of patients with cystic fibrosis is associated with pancreatic insufficiency. J Clin Microbiol. 2011;49:1004–9.
Horré R, de Hoog GS. Primary cerebral infections by melanized fungi: a review. Stud Mycol. 1999;43:176–93.
Sudhadham M, Prakitsin S, Sivichai S, et al. The neurotropic black yeast Exophiala dermatitidis has a possible origin in the tropical rain forest. Stud Mycol. 2008;61:145–55.
Branda E, Turchetti B, Diolaiuti G, et al. Yeast and yeast-like diversity in the southernmost glacier of Europe (Calderone Glacier, Apennines, Italy). FEMS Microbiol Ecol. 2010;72:354–69.
Matos T, de Hoog GS, de Boer AG, de Crom I, Haase G. High prevalence of the neurotrope Exophiala dermatitidis and related oligotrophic black yeasts in sauna facilities. Mycoses. 2002;45:373–7.
Hamada N, Abe N. Physiological characteristics of 13 common fungal species in bathrooms. Mycoscience. 2009;50:421–9.
Döğen A, Kaplan E, Oksüz Z, et al. Dishwashers are a major source of human opportunistic yeast-like fungi in indoor environments in Mersin, Turkey. Med Mycol. 2013;51:493–8.
Zupančič J, Novak Babič M, Zalar P, Gunde-Cimerman N. The black yeast Exophiala dermatitidis and other selected opportunistic human fungal pathogens spread from dishwashers to kitchens. PLoS ONE. 2016;11(2):e0148166.
Gümral R, Tümgör A, Saraçlı MA, et al. Black yeast diversity on creosoted railway sleepers changes with ambient climatic conditions. Microb Ecol. 2014;68:699–707.
Novak Babič M, Zalar P, Ženko B, Džeroski S, Gunde-Cimerman N. Yeasts and yeast-like fungi in tap water and groundwater, and their transmission to household appliances. Fungal Ecol. 2016;20:30–9.
Anaissie EJ, McGinnis RM, Pfaller AM. Clinical mycology. 2nd ed. Philadelphia: Churchill Livingstone Elsevier; 2009.
Russo JP, Raffaeli R, Ingratta SM, Rafti P, Mestroni S. Cutaneous and subcutaneous phaeohyphomycosis. Skinmed. 2010;8:366–9.
Park KY, Kim HK, Suh MK, Seo SJ. Unusual presentation of onychomycosis caused by Exophiala (Wangiella) dermatitidis. Clin Exp Dermatol. 2011;36:418–9.
Richardson DM, Warnock WD. Fungal infection: diagnosis and management. UK: Wiley-Blackwell; 2012. p. 383–90.
Banaoudia F, Assouline M, Pouliquen Y, Bouvet A, Guého E. Exophiala (Wangiella) dermatitidis keratitis after keratoplasty. Med Mycol. 1999;37:53–6.
Pastel SR, Hammersmith KM, Rapuano CJ, Cohen EJ. Exophiala dermatitidis keratitis after laser in situ keratomileusis. J Cataract Refract Surg. 2006;32:681–4.
Kerkmann ML, Piontek K, Mitze H, Haase G. Isolation of Exophiala (Wangiella) dermatitidis in a case of otitis externa. Clin Infect Dis. 1999;36:241–7.
Vlassopoulos D, Kouppari G, Arvanitis D, et al. Wangiella dermatitidis peritonitis in a CAPD patient. Perit Dial Int. 2001;39:2261–6.
Greig J, Harkness M, Taylor P, et al. Peritonitis due to the dermatiaceous mold Exophiala dermatitidis complicating continuous ambulatory peritoneal dialysis. Clin Microbiol Infect. 2003;9:713–5.
Kusenbach G, Skopnik H, Haase G, Friedrichs F, Dohmen H. Exophiala dermatitidis pneumonia in cystic fibrosis. Eur J Pediatr. 1992;151:344–6.
Mukaino T, Koga T, Oshita Y, et al. Exophiala dermatitidis infection in non-cystic fibrosis bronchiectasis. Respir Med. 2006;100:2069–71.
Taj-Aldeen SJ, El Shafie S, Alsoub H, Eldeeb Y, de Hoog GS. Isolation of Exophiala dermatitidis from endotracheal aspirate of a cancer patient. Mycoses. 2006;49:504–9.
Ozawa Y, Suda T, Kaida Y, et al. A case of bronchial infection of Wangiella dermatitidis. Nihon Kokyuki Gakkai Zasshi. 2007;45:907–11.
Haase G, Skopnik H, Kusenbach G. Exophiala dermatitidis infection in cystic-fibrosis. Lancet. 1990;336:188–9.
Diemert D, Kunimoto D, Sand C, Rennie R. Sputum isolation of Wangiella dermatitidis in patients with cystic fibrosis. Scand J Infect Dis. 2001;33:777–9.
Horré R, Schaal KP, Siekmeier R, et al. Isolation of fungi, especially Exophiala dermatitidis, in patients suffering from cystic fibrosis. A prospective study. Respiration. 2004;71:360–6.
Kabel PJ, Illy KE, Holl RA, Buiting AGM, Wintermans RGF. Nosocomial intravascular infection with Exophiala dermatitidis. Lancet. 1994;344:1167–8.
Myoken Y, Sugata T, Fujita Y, et al. Successful treatment of invasive stomatitis due to Exophiala dermatitidis in a patient with acute myeloid leukemia. J Oral Pathol Med. 2003;32:51–4.
Kenney RT, Kwon-Chung KJ, Waytes AT, et al. Successful treatment of systemic Exophiala dermatitidis infection in a patient with chronic granulomatous disease. Clin Infect Dis. 1992;14:235–42.
Matsumoto T, Matsuda T, McGinnis MR, Ajello L. Clinical and mycological spectra of Wangiella dermatitidis infections. Mycoses. 1993;36:145–55.
Fukushiro R, Kagawa S, Nishiyama S, Takahashi H. Un cas de chromoblastomycose cutanée avec métastase cérébrale mortelle. Presse Méd. 1957;65:2142.
Mori A, Morikawi H, Akagi M. A case of chromoblastomycosis due to Hormiscium dermatitidis. Skin Res. 1961;3:158.
Naka W, Fukuda T, Nishikawa T, et al. Cerebral Exophiala dermatitidis infection in a patient with a history of cutaneous Exophiala jeanselmei infection (in Japanese). 14th Kanto Med Mycol Conf.; 1993. p. 14.
Ikeda K, Kunisaki T, Abe H, et al. Chromoblastomycosis occurring with cerebral symptoms without cutaneous lesions (in Japanese). Sogo Rinsho. 1973;22:1463–71.
Chang LC, Kim D-S, Park JD, et al. Acute cerebral phaeohyphomycosis due to Wangiella dermatitidis accompanied by cerebrospinal fluid eosinophilia. J Clin Microbiol. 2000;38:1965–6.
Uijthof JMJ, de Hoog GS, de Cock AWAM, Takeo K, Nishimura K. Pathogenicity of strains of the black yeast Exophiala (Wangiella) dermatitidis: an evaluation based on polymerase chain reaction. Mycoses. 1994;37:235–42.
Lanternier F, Barbati E, Meinzer U, et al. Inherited CARD9 deficiency in 2 unrelated patients with invasive Exophiala infection. J Infect Dis. 2014;211:1241–50.
CDC - Centers for Disease Control and Prevention. Exophiala infection from contaminated injectable steroids prepared by a compounding pharmacy. Morb Mortal Wkly Rep. 2002;51:1109–12.
de Hoog GS, Matos T, Sudhadham M, Luijsterburg FK, Haase G. Intestinal prevalence of the neurotropic black yeast Exophiala (Wangiella) dermatitidis in healthy and impaired individuals. Mycoses. 2005;48:142–5.
Pedrozo CPM, de Azevedo S, Gomes RR, et al. Fonsecaea pugnacius, a novel agent of disseminated chromoblastomycosis. J Clin Microbiol. 2015;53:2674–85.
Sudhadham M, van den Ende AHG, Sihanonth P, et al. Elucidation of distribution patterns and possible infection routes of the neurotropic black yeast Exophiala dermatitidis using AFLP. Fungal Biol. 2011;115:1051–65.
Vicente AV, Attili-Angelis D, Pie MR, et al. Environmental isolation of black yeast-like fungi involved in human infection. Stud Mycol. 2008;61:137–44.
Duarte APM, Attili-Angelis D, Baron NC, Forti LC, Pagnocca FC. Leaf-cutting ants: an unexpected microenvironment holding human opportunistic black fungi. Antonie Van Leeuwenhoek. 2014;106:465–73.
Singh P, Raghukumar C, Verma P, Shouche Y. Phylogenetic diversity of culturable fungi from the deep-sea sediments of the Central Indian Basin and their growth characteristics. Fungal Divers. 2010;40:89–102.
Gadanho M, Sampaio JP. Occurrence and diversity of yeasts in the mid-Atlantic ridge hydrothermal fields near the Azores Archipelago. Microb Ecol. 2005;50:408–17.
Efstratiou M, Velegraki A. Recovery of melanized yeasts from Eastern Mediterranean beach sand associated with the prevailing geochemical and marine flora patterns. Med Mycol. 2009;48:1–3.
Vishniac HS. Yeast biodiversity in the Antarctic. In: Gabor P, Carlos Augusto R, editors. The yeast handbook. Biodiversity and ecophysiology of yeasts. Berlin: Springer; 2006. p. 419–40.
Teixeira MM, Moreno LF, Stielow BJ, et al. Exploring the genomic diversity of black yeasts and relatives (Chaetothyriales, Ascomycota). Stud Mycol. 2017;86:1–28.
Zhao J, Zeng J, de Hoog GS, Attili-Angelis D, Prenafeta-Boldú FX. Isolation and identification of black yeasts by enrichment on atmospheres of monoaromatic hydrocarbons. Microb Ecol. 2010;60:149–56.
Prenafeta-Boldú FX, Guivernau M, Gallastegui G, et al. Fungal/bacterial interactions during the biodegradation of TEX hydrocarbons (toluene, ethylbenzene and p-xylene) in gas biofilters operated under xerophilic conditions. FEMS Microbiol Ecol. 2012;80:722–34.
Blasi B, Poyntner C, Rudavsky T, et al. Pathogenic yet environmentally friendly? Black fungal candidates for bioremediation of pollutants. Geomicrobiol J. 2016;33:308–17.
Döğen A, Kaplan E, Ilkit M, de Hoog GS. Massive contamination of Exophiala dermatitidis and E. phaeomuriformis in railway stations in subtropical Turkey. Mycopathologia. 2013;175:381–6.
Yazdanparast SA, Mohseni S, De Hoog GS, et al. Consistent high prevalence of Exophiala dermatitidis, a neurotropic opportunist, on railway sleepers. J Mycol Med. 2017. doi:10.1016/j.mycmed.2017.01.007.
UKNCC. UKNCC biological resource: properties, maintenance and management. 1st ed. London: The UK National Culture Collection; 2001.
Heinrichs G, Hübner I, Schmidt KC, de Hoog GS, Haase G. Analysis of black fungal biofilms occurring at domestic water taps (I): compositional analysis using Tag-encoded FLX amplicon pyrosequencing. Mycopathologia. 2013;175:387–97.
Nishimura K, Miyaji M. Studies on a saprophyte of Exophiala dermatitidis isolated from a humidifier. Mycopathologia. 1982;77:173–81.
Gümral R, Özhak-Baysan B, Tümgör A, et al. Dishwashers provide a selective extreme environment for human opportunistic yeast-like fungi. Fungal Divers. 2016;76:1–9.
Matos T, Haase G, Gerrits van den Ende AHG, de Hoog GS. Molecular diversity of oligotrophic and neurotropic members of the black yeast genus Exophiala, with accent on E. dermatitidis. Antonie Van Leeuwenhoek. 2003;83:293–303.
Sterflinger K. Black yeasts and meristematic fungi: ecology, diversity and identification. In: Rosa AC, Gábor P, editors. Biodiversity and ecophysiology of yeasts. Berlin: Springer; 2006. p. 501–14.
Yurlova NA, de Hoog GS. Exopolysaccharides and capsules in human pathogenic Exophiala species. Mycoses. 2002;45:443–8.
Dadachova E, Bryan RA, Huang X, et al. Ionizing radiation changes the electronic properties of melanin and enhances the growth of melanized fungi. PLoS ONE. 2007;2(5):e457.
Kazanas N. Pathogenicity of a fungus resembling Wangiella dermatitidis isolated from edible mushrooms. Appl Environ Microbiol. 1986;51:261–7.
Acknowledgements
Authors kindly acknowledge everybody who helped to collect the samples. We also thank the Ministry of Higher Education, Science and Technology of the Republic of Slovenia in corporation with Slovenia Research Agency for financially supporting Jerneja Zupančič as a Young Researcher (Grant No. 382228-1/2013), as well as the Slovenian Research Agency ARRS for providing financial support to the Infrastructural Centre Mycosmo, MRIC UL (Grant P2-0103).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All other authors declare no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Babič, M.N., Zupančič, J., Gunde-Cimerman, N. et al. Ecology of the Human Opportunistic Black Yeast Exophiala dermatitidis Indicates Preference for Human-Made Habitats. Mycopathologia 183, 201–212 (2018). https://doi.org/10.1007/s11046-017-0134-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-017-0134-8