Abstract
This study examined health professionals’ (HPs) experience, beliefs and attitudes towards brain death (BD) and two types of donation after circulatory death (DCD)—controlled and uncontrolled DCD. Five hundred and eighty-seven HPs likely to be involved in the process of organ procurement were interviewed in 14 hospitals with transplant programs in France, Spain and the US. Three potential donation scenarios—BD, uncontrolled DCD and controlled DCD—were presented to study subjects during individual face-to-face interviews. Our study has two main findings: (1) In the context of organ procurement, HPs believe that BD is a more reliable standard for determining death than circulatory death, and (2) While the vast majority of HPs consider it morally acceptable to retrieve organs from brain-dead donors, retrieving organs from DCD patients is much more controversial. We offer the following possible explanations. DCD introduces new conditions that deviate from standard medical practice, allow procurement of organs when donors’ loss of circulatory function could be reversed, and raises questions about “death” as a unified concept. Our results suggest that, for many HPs, these concerns seem related in part to the fact that a rigorous brain examination is neither clinically performed nor legally required in DCD. Their discomfort could also come from a belief that irreversible loss of circulatory function has not been adequately demonstrated. If DCD protocols are to achieve their full potential for increasing organ supply, the sources of HPs’ discomfort must be further identified and addressed.
Similar content being viewed by others
Introduction
In most countries, irreversible loss of circulatory function and irreversible loss of brain function are the only two legally accepted criteria for determining death. Each criterion is, independently from the other, sufficient for legally declaring death.
Thus, for legal purposes neither criterion takes precedence over the other. Despite this, many proponents of the so-called “bifurcated standard” for declaring death have assumed that irreversible loss of brain function is the “gold standard” for the determination of death, and that loss of cardiac function serves merely as a surrogate marker (Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death 1968; Bernat et al. 1982, 2010; Capron 1999; President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research 1981). Little is known about where health professionals (HPs) stand on this issue. Lack of clarity about the relationship between brain death (BD) and circulatory death may not only contribute to HPs’ discomfort in managing donors, but may also negatively influence their ability and willingness to discuss the donation option with families (D’Alessandro et al. 2008; Mathur et al. 2008).
To better understand the extent to which these questions have an impact on organ procurement practices, we conducted a study in three leading countries in organ donation—France, Spain and the US—where both donation after BD and donation after circulatory death (DCD) are performed (Council of Europe 2009; Roels et al. 2007) (Table 1). We interviewed HPs likely to be involved in organ procurement and sought to compare their understanding of and their attitudes toward the two standards. We hypothesized that participants would express more doubts about donors’ vital status, and more discomfort about organ procurement in DCD than in BD.
Donation after circulatory death in France, Spain and the US
In 2009, Spain, the US and France had the 1st, 2nd and 4th highest rates of deceased donors per million population in the world (Council of Europe 2009). Because brain-dead donors have not met the increased demand for organs, the transplant communities in all three countries have turned to protocols designed to retrieve organs from patients declared dead by traditional cardiopulmonary criteria (DeVita et al. 1993). There are two categories of DCD: uncontrolled DCD (uDCD) and controlled DCD (cDCD). While in the US, most of DCD protocols are cDCD, in Spain and France cDCD has been excluded from policy for a long time because of ethical and pragmatic reasons (Cabrol 2007; Matesanz 1996; Rodriguez-Arias et al. 2010). In contrast to the US and Spain, for individuals declared dead according to circulatory criteria, French law requires a bedside clinical exam demonstrating total absence of consciousness, spontaneous motor activity and all brain stem reflexes, including spontaneous respiration (“Décret no. 2005-949 du 2 août 2005 relatif aux conditions de prélèvement des organes, des tissus et des cellules et modifiant le livre II de la première partie du code de la santé publique (dispositions réglementaires), art. R1232-1” 2005). However, in none of the three countries, is there a requirement in DCD protocols for an apnea test, EEG, imaging studies or any proof of the absence of hypothermia or central nervous system (CNS) depressant drugs, which are, otherwise, routinely required for a BD diagnosis.
Materials and methods
Study instrument
This exploratory-descriptive study used a survey design to gather information from HPs who were likely to be involved in the process of organ donation. Our questionnaire was adapted from a previous study (Youngner et al. 1989). Two new scenarios of DCD were added (see “Scenarios” below). The final questionnaire consisted of 60 questions.
Validation of instrument
We used methods that had been validated in the previous study (Youngner et al. 1989). Scenario A (BD) and the associated questions were replicated from this study. Scenarios B (uDCD) and C (cDCD) were constructed by a team of four bioethicists (two physicians and two philosophers) and a social scientist. Three questions concerning Scenarios B and C were replicated from those used and validated with Scenario A. Two questions focusing on the necessity and possibility of demonstrating irreversible loss of all brain functions in both DCD scenarios were added. The study instrument was pilot tested in France (n = 60) and Spain (n = 36) for clarity in interpretation of each scenario and related questions, with satisfactory results. In order to validate the questionnaire in the three languages, a back-translation procedure was followed.
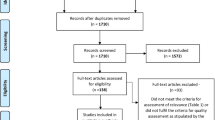
Inclusion criteria and sample
Between April 2007 and February 2008, 587 HPs involved in the care of potential donors and/or in the determination of death, and/or in the organ retrieval process were individually interviewed face-to-face in 14 hospitals in France, Spain and the US. The study protocol was submitted to and approved by institutional review boards in all three countries. The goal of the study was to collect data from 150 to 200 subjects in each country. The study was based on a cross-sectional design using different sampling methods. These methods were adapted to variations in hospital structure, leadership and policies. When the numbers of subjects belonging to a specific group (e.g. transplant coordinators) were small, attempts were made to collect data from all subjects in the group. For large groups (e.g. ICU nurses), a random sample was chosen. Sometimes, when policy or hospital leadership limited access to potential subjects, samples of convenience were used. Here, the interviewer remained in the service area during a given shift and approached all professionals working that shift.
Demographics: comparisons by countries
Statistical differences in terms of age, religion and specialty were found between countries. Distribution of our sample by these variables countries is shown in Table 2.
Measures and data collection
We examined study subjects’ experience, personal beliefs and attitudes about the three organ procurement protocols using case scenarios that are detailed below. Questions regarding beliefs and attitudes included whether: (1) each organ procurement protocol adequately determines death; (2) it is necessary to verify BD in DCD (both uDCD and cDCD); (3) it is possible to do so by a bedside clinical exam alone (we defined “bedside clinical exam” as an “exam with no special technical diagnostic measures—for example, EEG or apnea test”) and (4) it is morally acceptable to procure organs in the three cases.
Scenarios
Scenario A: brain death
Patient A has sustained irreversible loss of all brain functions according to the tests required by the medical standards in your state/country. Other physiological functions (e.g., beating heart, maintenance of blood pressure, electrolyte balance, etc.) are supported by intensive medical care.
Scenario B: uncontrolled DCD
Patient B suffers severe chest pain at home and an ambulance is called by the family. Shortly after the Emergency Medical Technicians (EMTs) arrive at the home, Patient B suffers cardiopulmonary arrest and they attempt cardiopulmonary resuscitation (CPR) for over 30 min, but without success. The patient is then transported to the hospital while CPR and assisted ventilation are continued. At the hospital, the emergency medical team decides to stop resuscitation after making the clinical judgment that it will not be successful. After CPR is stopped, no activity is indicated on an electro cardiogram (EKG) for 5 min. Considering that the patient is a candidate for organ donation, mechanical cardiac massage and ventilation are then restarted until the patient undergoes extra-corporeal membrane oxygenation (ECMO) [to preserve the organs]. The patient is now on ECMO (Fondevila et al. 2007).
Scenario C: controlled DCD
Patient C is a 45-year-old man who has suffered severe brain injury in a car accident. He is admitted to the ICU and seems to be progressing to BD. However, he stabilizes somewhat and does not meet brain-death criteria. The physicians tell the family that Patient C will never recover consciousness, will remain ventilator dependent, and will likely die from cardiovascular collapse within a week. The patient had signed a donor card and the family is anxious to donate his organs, but he is not brain-dead. The family agrees to DCD. The patient is taken to the operating room (OR) where he is prepped for surgery. The ventilator is disconnected. A few minutes later he suffers circulatory arrest with ventricular fibrillation. There is no effective circulation as measured by a femoral artery catheter. Two minutes after circulatory arrest, the patient is declared dead and organ retrieval surgery begins. The protocol states that after 2 min of circulatory arrest a patient is dead because the loss of cardiac function is irreversible. This is justified, the protocol reads, because a morally sound decision has been made not to reverse the ventricular fibrillation even though the technology is present that could possibly do so (Marquis 2010; Steinbrook 2007; Youngner et al. 1999).
Analysis
Chi-squares were used to make comparisons among specific subjects groups from the three countries for the outcomes of interest. In addition, Cochran’s Q was used to make comparisons of the total sample across the three scenarios.
Results
Sample
The total study sample consisted of 587 HPs (221 in France, 198 in Spain, 169 in the US).
In France, 221 of a potential 635 interviews were completed in 6 hospitals in Parisian region (Kremlin Bicêtre, Suresnes, Evry and Créteil) and Region of Lyon (Lyon and Bron). The Director of the Neurosurgical ICU in one of the hospitals refused the participation of his department. Interviews were attempted with the remaining 63 physicians who might have a role in declaring death. Forty-nine of them completed the survey. Three refused to participate; the others were absent at the time of the interviews. Of the 49 interviewees, 43 were intensivists, and 6 were physician transplant coordinators. Of the 572 HPs who might have a role in the clinical management of dead donors, 172 completed the survey. Thirteen of 14 nurse organ coordinators completed the interview. Twelve of 18 transplant surgeons were interviewed; the others were absent at the time of the interviews. Of 79 anesthesiologists, 31 of 33, chosen by convenience sample, agreed to complete interviews. Of 233 ICU nurses, 100 OR nurses, and 127 anesthetist nurses, convenience samples 68, 17, and 30 respectively completed interviews. One nurse who specialized in ECMO was interviewed.
In Spain, 198 of a potential 414 interviews were completed in 6 hospitals from 5 cities: Barcelona, Coruña, Madrid, Salamanca and Santiago de Compostela. Interviews were attempted with the 104 potentially available physicians who might have a role in declaring death or in discussing the donation option with the families. Sixty-seven of them completed the survey. Six refused to participate and in 31 cases either interviews could not be scheduled or HPs failed to show up for scheduled interviews. Of these 67 HPs interviewed, 36 were ICU physicians, 5 were neurosurgeons, 5 were neurologists, 4 were ICU fellows, 15 were physician transplant coordinators and two were physician neurophysiologists. One hundred thirty-one of the 310 HPs who might have a role in the clinical management of dead patients completed the survey. All 8 available non physician transplant coordinators completed interviews. Eighty-five of the 218 potentially available ICU nurses were randomly selected and, of these, 6 refused and 79 completed interviews. Forty-four of the 84 potentially available OR staff were interviewed. Six refused and 34 could not be scheduled. Among the 44 staff that completed the survey, 12 were transplant surgeons, 14 were anesthesiologists, 10 were OR nurses, and 8 were “other” groups of physicians who participate in the organ retrieval, including 3 urologists, 2 pneumologists, 1 nephrologist, 1 cardiologist and 1 gastroenterologist.
In the US, 169 of a potential 287 interviews were completed in 2 hospitals in Cleveland, Ohio. In one hospital, interviews were attempted with all 105 physicians who might have a role in declaring death. Seventy-five of them completed the survey. Eleven medical intensivists did not participate because their chairmen failed to respond to our request for permission to approach his faculty. The other 19 non participants either did not respond to attempts at contact or agreed to an interview but could not find time. Of the 75 interviewed, 31 were neurologists, 12 were neurosurgeons, and 32 were surgical, pediatric or medical intensive care physicians. Interviews were attempted with the 182 HPs who might have a role in the clinical management of dead donors; 94 completed the survey. Forty-nine of the 55 potentially available ICU nurses were interviewed by a convenience sample method in which the interviewer sat in the ICU during any given shift and approached all nurses working that shift. Of the 55, 3 refused and 3 were not approached because of time constraints. Forty-one of the 58 potentially available OR nurses were interviewed by the same convenience sample method. None refused to participate. All 4 potentially available transplant surgeons completed the survey. Interviews with the other 65 OR professionals, namely anesthesiologists, could not be scheduled because of the lack of responses from the chairmen at one hospital and the lack of responses from individual anesthesiologists at the other (Table 2).
Experience with donation after brain death and after circulatory death
Five hundred and twenty-eight (91%) study subjects had participated in the clinical care or the organ retrieval of a brain-dead donor (Scenario A), 123 (21%) of a donor who underwent uDCD (Scenario B), and only 16 (3%) of a donor who underwent cDCD (Scenario C). In our sample, a higher proportion of French and Spanish HPs had experience with BD (France n = 209, 95%; Spain n = 182, 93%; US n = 137, 83%) (P < 0.001) and with uDCD (France n = 63, 29%; Spain n = 48, 25%; US n = 12, 7%) (P < 0.001). Americans had more experience with cDCD (France n = 0; Spain n = 3, 2%; US n = 13, 8%) (P < 0.001) (Table 3).
Personal beliefs about organ donors being dead or alive
In response to questions about Scenarios A, B and C, 551 study subjects (94%) had the personal belief that a brain-dead patient is dead, 497 (85%) believed that a donor under uDCD is dead, and 331 (57%) believed that a donor under cDCD is dead. In comparing the belief that the patient is dead across the three scenarios, some differences were found. (Cochran’s Q = 257.752, df = 2, P < 0.001). Compared to the French and Spanish, Americans were more likely to believe that Patient C (cDCD) is dead. (US n = 113, 67%; France n = 117, 53%; Spain n = 101, 52%;) (P < 0.001) (Table 4).
Primacy of brain death or circulatory death in DCD
In order to understand HPs’ beliefs about the interrelationship between BD and circulatory death, and about the primacy of one standard over the other, HPs were asked whether circulatory criteria are sufficient for declaring death in DCD and—for those who answered that a brain exam is also necessary—whether it is possible to assess BD by a bedside clinical exam. These two questions were asked in both DCD scenarios.
Brain death in uncontrolled DCD
Three hundred and twenty-four participants (55%) believed that circulatory criteria alone are sufficient for declaring death in uDCD (they did not consider it also necessary to demonstrate irreversible loss of all brain function for these donors). Spanish professionals were the least likely to hold this position (Spain n = 94, 48%; France n = 127, 58%; US n = 103, 61%) (P < 0.01). Of the 248 (42%) subjects who considered that a determination of BD is also necessary for the uDCD donor to be dead, 172 (69%) believed that BD cannot be satisfactorily assessed by a bedside clinical exam alone (Table 5). Ironically, although only 89 participants (15%) answered that donors such as Patient B are alive (or didn’t know) (Table 4), nearly double that number (172, 29% of the total sample) felt that BD should, but cannot, be demonstrated in those cases (Table 5).
Brain death in controlled DCD
Three hundred and forty-nine participants (60%) believed that circulatory criteria are sufficient for declaring death in cDCD protocols. Spanish professionals were the least likely to hold this position (Spain n = 96, 51%; France n = 126, 57%; US n = 128, 76%) (P < 0.001). Of the 194 subjects (34%) who considered that a determination of BD is also necessary for these patients, 141 (73%) believed that BD cannot be satisfactorily assessed by a brief bedside clinical exam alone (Table 5).
Attitudes towards organ procurement
Almost all participants (98%) considered it acceptable to procure organs in Scenario A (BD). There were no statistical differences between countries in this regard. In all three countries, acceptance of organ procurement in both DCD protocols was considerably less than that for BD: comparing the moral acceptability of organ procurement across the three scenarios using the entire study sample showed significant differences (Cochran’s Q = 278.72, df = 2, P < 0.001). Among all participants, 125 (21%) considered organ procurement unacceptable in Scenario B (uDCD) and 222 (38%) in Scenario C (cDCD). cDCD was the least morally accepted practice overall, and also the one in which the most national differences occurred: 92 (47%) Spanish, 80 (37%) French and 51 (30%) American professionals considered it unacceptable (P < 0.001) (Table 6).
Discussion
Our study has two main findings: (1) In the context of organ procurement, HPs believe that BD is a more reliable standard for determining death than circulatory death, and (2) While the vast majority of HPs consider it morally acceptable to retrieve organs from brain-dead donors, retrieving organs from DCD patients is much more controversial. We offer four possible explanations.
First, HPs involved in providing care to potential donors, declaring death, or procuring organs are less familiar with DCD protocols. After four decades of experience, HPs have become comfortable with the idea that death can be declared by neurological criteria even in the presence of a beating heart, and that organ procurement can follow such a diagnosis. More recently, DCD protocols have exposed HPs to a new situation in which organ procurement can take place when the heart has stopped but irreversible loss of all brain function has not been rigorously demonstrated. Whereas 91% of our study subjects had been involved with a brain-dead donor, only 21% had been involved with uDCD and 3% with cDCD. In France and Spain, where cDCD is not regularly practiced, the numbers were particularly low, as they were for uDCD in the US, where it is rarely practiced. It appears that time and experience have changed the understanding and acceptance of BD over the last two decades. This conclusion is supported by a comparison of our data with that from a 1989 study that addressed many of the same issues (Youngner et al. 1989).
Second, DCD protocols have introduced new conditions that clearly deviate from normal medical practice. For example, uDCD initiates invasive measures before, rather than after, seeking family permission, and restores cardiopulmonary function after death is declared (Borry et al. 2008; Doig and Zygun 2008; Volk et al. 2010; Wall et al. 2011). In cDCD protocols, death is most often declared in the OR (a place where death rarely occurs and is generally unwelcome). Intravenous heparin or vasodilators may be administered to improve organ function before the donor is dead (Bernat 2008; Gardiner and Sparrow 2010). Bernat has suggested that some of these deviations “test the permissible societal boundaries of donation after circulatory death” (Bernat 2008).
Third, DCD protocols allow procuring organs at a time when the donor’s loss of circulatory function could actually be reversed. In cDCD, organs are procured as soon as 75 s or 2 min after circulatory arrest (Boucek et al. 2008). After such a short period, circulatory function could be restored with aggressive intervention, and even spontaneously (Hornby et al. 2010; Institute of Medicine 1999). Although the law in most countries requires irreversible loss of circulatory function for declaring death by cardiopulmonary criteria, DCD protocols use a weak, contingent and context-dependent meaning of irreversibility—the so-called permanent cessation—(Marquis 2010; Menikoff 1998; Youngner et al. 1999). This position has been endorsed by the Institute of Medicine (IOM) and a recent Health Resources and Services Administration (HRSA) panel of experts (Bernat et al. 2010; Institute of Medicine 1999, 2006). Permanent cessation ultimately relies on a moral judgment that attempts to reverse ought not to rather than cannot be made (Marquis 2010; Verheijde et al. 2007). Several commentators have warned of the theoretical and practical problems which arise if death declarations ultimately depend on moral judgments (Joffe 2007; Marquis 2010; McMahan 2006; Molina et al. 2008; Rodriguez-Arias et al. 2011).
Another related problem for HPs’ acceptance, in this case, of uncontrolled DCD protocols, is the recent finding by Hornby et al. 2010 that attempting to restore circulatory function through resuscitation efforts increases the chances of spontaneous auto-resuscitation after failed CPR. The longest reported auto-resuscitation time interval after asystole is 7 min (Hornby et al. 2010). Furthermore, new evidence suggests that some of the patients judged to have failed standard resuscitation in the field, could survive (even with good neurological outcomes), if more innovative resuscitative efforts (e.g. percutaneous coronary interventions with ongoing mechanical CPR) are implemented (Wagner et al. 2010). In summary, the official position about the determination of the moment of death in DCD protocols has depended more on a moral judgment about what should be done rather than a clinical assessment of what can be done. While some HPs working in transplant environments may understand and accept the official position about irreversibility, others remain uncomfortable.
The responses ‘no’ to our question ‘in your opinion, is the Patient-B or C-dead?’ do not allow us to determine whether professionals’ relative reluctance to consider DCD donors dead just reflects skepticism towards currently accepted criteria and tests to determine circulatory death (e.g. they distrust the standard tests to verify that loss or circulatory function is irreversible), or a deeper conceptual concern (i.e. they believe that the heart is not a vital organ but the brain is). Similarly, the responses, ‘no’ to our question ‘is it necessary to demonstrate that all brain function of Patient-B or C-is irreversibly lost for the patient to be declared dead?’ do not allow us to determine whether those professionals believed that (a) only the death of the brain counts as death and cardiac measures by themselves accurately measure the death of the brain or (b) the cessation of circulatory function is itself death so the status of the brain is irrelevant. However, the interpretation of the answers “yes” to the last question (42% in uDCD and 33% in cDCD) does not fall into the same kind of indetermination. For significant minorities of professionals, cardiac measures by themselves do not accurately measure the death of the brain, and the death of the brain is—according to them—necessary for an individual to be declared dead. In other words, for significant minorities of HPs, verification of BD in DCD cases is not expendable.
We thus offer a fourth explanation: DCD protocols bring into question the notion that death is a unified concept; that the two standards for identifying it are interchangeable. This contradicts the previously mentioned assumption, made by defenders of the bifurcated standard, that both cardiopulmonary and neurological criteria represent a unified notion of death so that one does not have to choose between them (Capron 1999; Capron and Kass 1972; President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research 1981). To support that assumption, some have claimed that when death is declared by cardio-respiratory criteria, loss of all brain function has or will quickly become irreversible (Bernat et al. 2010; Capron 1999). As Menikoff has pointed out, this rationale supports the official viewpoint that cardio-respiratory criteria have always served as a surrogate for determining the status of the brain (Menikoff 1998). In most clinical settings where death occurs, cardio-respiratory arrest is indeed immediately followed by loss of brain function and vice versa. However, this is not the case with organ procurement in critical care settings. In brain-dead donors, the heart continues to beat. In DCD, organs must be taken so close to the time of circulatory arrest that irreversible loss of neurological function cannot be thoroughly evaluated. According to Verheijde et al. (2007), this fact has important and potentially disturbing implications. By declaring death before an adequate determination of irreversible loss of all brain function, donors retain the potential for regaining some degree of consciousness and, perhaps, experiencing harm. Glannon has recently addressed the issue of the relationship between harm, organ procurement and death determinations. He argues that donors’ experiential and surviving interests (i.e. that they do not experience pain and that their previous whishes are respected) are morally more relevant than their vital status (Glannon 2011).
It has been acknowledged that ECMO could actually restore brain function in some DCD patients (Bernat et al. 2010; Shemie et al. 2006; Verheijde et al. 2007). To prevent this possibility, measures can be taken to block the aorta between the organs being perfused and the brain (Bernat et al. 2010; Shemie 2007; Wall et al. 2011). Even if this procedure is successful in preventing a return of consciousness, it represents yet another highly invasive deviation from the standard care of dead individuals or dying patients (Bernat 2008). One could even argue that this is a form of causing the death of the donor (Rodriguez-Arias et al. 2011). In BD protocols, death is declared and acted upon while the heart continues to pump oxygenated blood throughout the body. However,—given the present limits of medical technology and knowledge—there is a supposed certainty that the neurological condition is irreversible, even when the stronger concept of irreversibility is applied. A rigorous clinical protocol requires not only a clear demonstration of loss of function of the whole brain, but also that potentially reversible conditions such as hypothermia and presence of CNS suppressants have been excluded. This is clearly the stronger meaning of irreversible. In contrast, DCD protocols merely focus on permanent loss of circulatory function. They do not insist on the same set of confirmatory tests for the brain that are required by BD protocols (Youngner et al. 1999).
Significant minorities of our study subjects insisted that there should be a determination of death by neurological criteria in both uDCD (42%) and cDCD (34%), while a majority of each of these concerned groups (69% for uDCD and 73% for cDCD) thought that BD cannot be adequately determined by a bedside exam alone. Interestingly, even in France, where a more formal but not comprehensive BD exam is required by law in DCD, French professionals expressed concern in the same proportion as their colleagues in the two other countries.
Differences between countries
In many ways, the data from the three countries is quite consistent. That French and Spanish HPs seem to have more experience with BD can be explained by the existence of in-hospital transplant coordinators in these countries. Experience with uDCD is more frequent in Spain and in France than in the US, which is consistent with the incidence of this protocol in each country (Table 1). Conversely, experience with cDCD is more frequent in the US than in Spain and France, which is consistent with its greater use there. Because of our study did not address differences in practice, they can only be speculated upon. It is possible that greater ease of turning off ventilators in the US (Esteban et al. 2001; Ferrand et al. 2001; Nelson et al. 2006) explains the more widespread use of cDCD there. uDCD may be used more widely in France and Spain because of their greater emphasis on opt-out system for donation. Our finding of a reluctance to accept cDCD patients as dead in Spain and France, as compared to the US, may be due to the infrequent use of cDCD in those two countries. It is not clear why there is greater insistence in Spain that more rigor be applied in determining BD in both DCD protocols.
Limitations of the study
This study has several limitations. First, the results are based on a structured interview and hypothetical scenarios, rather than actual cases. It is certainly possible that some respondents would have answered questions differently had they been confronted with real patients in a clinical setting. Nevertheless, clearly delineated hypothetical cases are a useful way to understand and compare professionals’ thinking in different countries. Second, our study was conducted at a limited number of hospitals in each country (2 in the US, 6 in Spain and 6 in France). It is possible that responses may vary according to geographical region or type of hospital and are therefore not generalizable. Third, because of different organizational structures in the institutions studied, we had to use a convenience sample in some cases. Such variation in sampling could, theoretically, skew the results, though how it might do so is not obvious. Finally, in Scenario C (cDCD), we mentioned a stand-off period of 2 min after circulatory arrest, a policy which is not shared by all cDCD protocols (the waiting time varies among local protocols from 75 s to 10 min). In this scenario we also told participants about the specific meaning of “irreversible” that applied. Although all cDCD protocols ground their justification in this meaning, mentioning it could have raised concerns that would not otherwise have been expressed.
Conclusions and implications for policy making
Our data indicate that HPs are significantly less comfortable with DCD than with BD protocols. How do we understand these findings regarding their implications for policies which aim to increase organ procurement rates?
First, that some HPs believe that DCD donors are not dead admits of at least two interpretations. On one hand, one could conclude that subjects who do not hold the “official” position are mistaken: they simply lack factual knowledge. If this is the case, more education about the “official” determination of death may help solve the problem. On the other hand, subjects who do not hold the official position could be expressing an intellectually legitimate rejection of the theoretical underpinnings of the official point of view. Certainly, many scholars have taken this position (Marquis 2010; Menikoff 1998; Miller et al. 2010; Rady et al. 2008; Shewmon and Shewmon 2004; Veatch 2010).
That HPs are concerned about DCD protocols seems to be related in part to the fact that these protocols do not require a rigorous examination of brain function. Again, it is unclear whether this discomfort is the result of lack of education and experience or represents a more fundamental intuition that the brain alone holds the key position in the determination of death (rather than sharing it with the heart) and is not adequately accounted for in DCD protocols (Hester and Green 2011).
How might all this play out? Some authors have argued that “death” is a social construct that changes over time (Arnold and Youngner 1993; Veatch 1989). What seem like important ethical or conceptual concerns fade over time or remain hidden from view. This phenomenon has been called “policy creep”. Policy creeps more steadily if symbolic harms are dwarfed by important and tangible goods, for example, saving the lives of thousands of clearly identified individuals without harming the interests of irreversibly unconscious, brain-dead donors (Feinberg 1985). Calabresi and Bobbit addressed this issue in their classic work, “Hard Choices” and it was applied to DCD by Arnold and Youngner (Arnold and Youngner 1993). Speaking of early DCD controversies they wrote:
Given the difficulties our society is likely to experience in trying to openly adjudicate these disparate views, why not simply go along with the quieter strategy of policy creep? It seems to be getting us where we seem to want to go, albeit, slowly. Besides, total candor is not always compatible with the moral compromises that inevitably accompany the formulation of public policy. (Arnold and Youngner 1993, p. 272)
This pragmatic approach to increasing the supply of organs could be seriously undermined if the gradual deviations from standard practices and the reconstruction of death to facilitate organ transplantation do not take seriously potential sources of discomfort (moral or other), as is the case in DCD. In such circumstances, attempts to address the discomfort, particularly among HPs who have to carry out “policy creep” in practice, become necessary. Indeed, it is not difficult to imagine how unexamined “policy creep” could open the door to potentially devastating scenarios for patients, families, procurement and transplant professionals and the broader society. Even a single instance, for example, of a uDCD donor “waking up” after being placed on ECMO would be tragic not only for those involved, but, by severely damaging public confidence and trust, could also undermine decades of work in increasing the organ supply. To avoid such an undesirable outcome, transparent policies and qualitative research to properly understand the sources of public alarm and HPs’ discomfort are necessary. Careful and critical examination of protocols and practices could inform the necessary strategies to reduce professionals’ unease and to minimize the chances of losing public trust in organ transplantation. It is our hope that this study of the attitudes and beliefs of HPs involved in organ procurement in three countries regarding BD, uDCD, and cDCD is a small step to furthering this end.
References
Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death. 1968. A definition of irreversible coma. Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death. JAMA 205(6): 337–340.
Arnold, R.M., and S.J. Youngner. 1993. The dead donor rule: Should we stretch it, bend it, or abandon it? Kennedy Institute of Ethics Journal 3(2): 263–278.
Bernat, J.L. 2008. The boundaries of organ donation after circulatory death. New England Journal of Medicine 359(7): 669–671.
Bernat, J.L., C.M. Culver, and B. Gert. 1982. Defining death in theory and practice. The Hastings Center Report 12(1): 5–8.
Bernat, J.L., A.M. Capron, T.P. Bleck, S. Blosser, S.L. Bratton, J.F. Childress, et al. 2010. The circulatory-respiratory determination of death in organ donation. Critical Care Medicine 38(3): 963–970.
Borry, P., W. Van Reusel, L. Roels, and P. Schotsmans. 2008. Donation after uncontrolled cardiac death (uDCD): A review of the debate from a European perspective. The Journal of Law, Medicine & Ethics 36(4): 752–759, 610.
Boucek, M.M., C. Mashburn, S.M. Dunn, R. Frizell, L. Edwards, B. Pietra, et al. 2008. Pediatric heart transplantation after declaration of cardiocirculatory death. New England Journal of Medicine 359(7): 709–714.
Cabrol, C. 2007. Prélèvements d’organes sur donneur à coeur arrêté. Académie Nationale de Médecine.
Capron, A.M. 1999. The bifurcated legal standard for determining death: Does it work? In The definition of death: Contemporary controversies, ed. S.J. Youngner, R. Arnold, and R. Schapiro, 117–136. Baltimore: The Johns Hopkins University Press.
Capron, A.M., and L.R. Kass. 1972. A statutory definition of the standards for determining human death: An appraisal and a proposal. University of Pennsylvania Law Review 121(87): 102–104.
Council of Europe. 2009. International figures on donation and transplantation—2008. Newsletter Transplant 14(1): 26–29.
D’Alessandro, A.M., J.W. Peltier, and J.E. Phelps. 2008. Understanding the antecedents of the acceptance of donation after cardiac death by healthcare professionals. Critical Care Medicine 36(4): 1075–1081.
Décret no. 2005-949 du 2 août .2005. Relatif aux conditions de prélèvement des organes, des tissus et des cellules et modifiant le livre II de la première partie du code de la santé publique (dispositions réglementaires), art. R1232-1. Journal Officiel de la République Française, 6 août 2005.
DeVita, M.A., J.V. Snyder, and A. Grenvik. 1993. History of organ donation by patients with cardiac death. Kennedy Institute of Ethics Journal 3(2): 113–129.
Doig, C.J., and D.A. Zygun. 2008. (Uncontrolled) donation after cardiac determination of death: A note of caution. The Journal of Law, Medicine & Ethics 36(4): 760–765, 610.
Esteban, A., F. Gordo, J.F. Solsona, I. Alia, J. Caballero, C. Bouza, et al. 2001. Withdrawing and withholding life support in the intensive care unit: A Spanish prospective multi-centre observational study. Intensive Care Medicine 27(11): 1744–1749.
Feinberg, J. 1985. The mistreatment of dead bodies. The Hastings Center Report 15(1): 31–37.
Ferrand, E., R. Robert, P. Ingrand, and F. Lemaire. 2001. Withholding and withdrawal of life support in intensive-care units in France: A prospective survey. French LATAREA Group. Lancet 357(9249): 9–14.
Fondevila, C., A.J. Hessheimer, A. Ruiz, D. Calatayud, J. Ferrer, R. Charco, et al. 2007. Liver transplant using donors after unexpected cardiac death: Novel preservation protocol and acceptance criteria. American Journal of Transplantation 7(7): 1849–1855.
Gardiner, D., and R. Sparrow. 2010. Not dead yet: Controlled non-heart-beating organ donation, consent, and the dead donor rule. Cambridge Quarterly of Healthcare Ethics 19(1): 17–26.
Glannon, W. 2011. Donation, death, and harm. The American Journal of Bioethics 11(8): 48–49.
Hester, D.M., and J. Green. 2011. It’s all about the brain. The American Journal of Bioethics 11(8): 44–45.
Hornby, K., L. Hornby, and S.D. Shemie. 2010. A systematic review of autoresuscitation after cardiac arrest. Critical Care Medicine 38(5): 1246–1253.
Institute of Medicine. 1999. Non-heart-beating transplantation II: The scientific and ethical basis for practice and protocols. Washington, DC.
Institute of Medicine. 2006. Opportunities for action. Washington, DC: National Academies Press.
Joffe, A.R. 2007. The ethics of donation and transplantation: Are definitions of death being distorted for organ transplantation? Philosophy, Ethics, and Humanities in Medicine 2: 28.
Marquis, D. 2010. Are DCD donors dead? Hastings Center Report 40(3): 24–31.
Matesanz, R. 1996. Documento de consenso español sobre extracción de órganos de donantes en asistolia. Nefrologia XVI(suppl. 2): 48–53.
Mathur, M., S. Taylor, K. Tiras, M. Wilson, and S. Abd-Allah. 2008. Pediatric critical care nurses’ perceptions, knowledge, and attitudes regarding organ donation after cardiac death. Pediatric Critical Care Medicine 9(3): 261–269.
McMahan, J. 2006. An alternative to brain death. The Journal of Law, Medicine & Ethics 34(1): 44–48, 43.
Menikoff, J. 1998. Doubts about death: The silence of the Institute of Medicine. The Journal of Law, Medicine & Ethics 26(2): 157–165.
Miller, F.G., R.D. Truog, and D.W. Brock. 2010. The dead donor rule: Can it withstand critical scrutiny? Journal of Medicine and Philosophy 35(3): 299–312.
Molina, A., D. Rodríguez-Arias, and S.J. Youngner. 2008. Should individuals choose their definition of death? Journal of Medical Ethics 34(9): 688–689.
Nelson, J.E., D.C. Angus, L.A. Weissfeld, K.A. Puntillo, M. Danis, D. Deal, et al. 2006. End-of-life care for the critically ill: A national intensive care unit survey. Critical Care Medicine 34(10): 2547–2553.
President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. 1981. Defining death: Medical, legal and ethical issues in the determination of death. Washington, DC: Government Printing Office.
Rady, M.Y., J.L. Verheijde, and J. McGregor. 2008. Organ procurement after cardiocirculatory death: A critical analysis. Journal of Intensive Care Medicine 23(5): 303–312.
Rodriguez-Arias, D., L. Wright, and D. Paredes. 2010. Success factors and ethical challenges of the Spanish model of organ donation. Lancet 376(9746): 1109–1112.
Rodriguez-Arias, D., M.J. Smith, and N.M. Lazar. 2011. Donation after circulatory death: Burying the dead donor rule. The American Journal of Bioethics 11(8): 36–43.
Roels, L., B. Cohen, and C. Gachet. 2007. Countries’ donation performance in perspective: Time for more accurate comparative methodologies. American Journal of Transplantation 7(6): 1439–1441.
Shemie, S.D. 2007. Clarifying the paradigm for the ethics of donation and transplantation: Was ‘dead’ really so clear before organ donation? Philosophy, Ethics, and Humanities in Medicine 2: 18.
Shemie, S.D., A.J. Baker, G. Knoll, W. Wall, G. Rocker, D. Howes, et al. 2006. National recommendations for donation after cardiocirculatory death in Canada: Donation after cardiocirculatory death in Canada. CMAJ 175(8): S1.
Shewmon, A.D., and E.S. Shewmon. 2004. The semiotics of death and its medical implications. In Brain death and disorders of consciousness. Proceedings of the IV international symposium on coma and death, held March 9–12, 2004, in Havana, Cuba, eds. C. Machado, and A.D. Shewmon, 89–114. New York: Kluwer/Plenum.
Steinbrook, R. 2007. Organ donation after cardiac death. New England Journal of Medicine 357(3): 209–213.
UNOS. 2007. Annual report, OPTN data. http://optn.transplant.hrsa.gov. Accessed 28 Nov 2011.
UNOS. 2008. Annual report, OPTN data. http://optn.transplant.hrsa.gov. Accessed 28 Nov 2011.
Veatch, R.M. 1989. Death, dying and the biological revolution. New York: Yale University Press.
Veatch, R.M. 2010. Transplanting hearts after death measured by cardiac criteria: The challenge to the dead donor rule. Journal of Medicine and Philosophy 35(3): 313–329.
Verheijde, J.L., M.Y. Rady, and J. McGregor. 2007. Recovery of transplantable organs after cardiac or circulatory death: Transforming the paradigm for the ethics of organ donation. Philosophy, Ethics, and Humanities in Medicine 2: 8.
Volk, M.L., G.J. Warren, R.R. Anspach, M.P. Couper, R.M. Merion, and P.A. Ubel. 2010. Attitudes of the American public toward organ donation after uncontrolled (sudden) cardiac death. American Journal of Transplantation 10(3): 675–680.
Wagner, H., C.J. Terkelsen, H. Friberg, J. Harnek, K. Kern, J.F. Lassen, et al. 2010. Cardiac arrest in the catheterisation laboratory: A 5-year experience of using mechanical chest compressions to facilitate PCI during prolonged resuscitation efforts. Resuscitation 81(4): 383–387.
Wall, S.P., B.J. Kaufman, A.J. Gilbert, Y. Yushkov, M. Goldstein, J.E. Rivera, et al. 2011. Derivation of the uncontrolled donation after circulatory determination of death protocol for New York City. American Journal of Transplantation 11(7): 1417–1426.
Youngner, S.J., C.S. Landefeld, C.J. Coulton, B.W. Juknialis, and M. Leary. 1989. ‘Brain death’ and organ retrieval. A cross-sectional survey of knowledge and concepts among health professionals. JAMA 261(15): 2205–2210.
Youngner, S.J., R.M. Arnold, and M.A. DeVita. 1999. When is “dead”? The Hastings Center Report 29(6): 14–21.
Acknowledgments
This study was supported in part by the French Agence de la Biomédecine and by an unrestricted grant from the Musculoskeletal Transplant Foundation. We thank Carissa Véliz, Sam Shemie, Howard Doyle and Linda Wright for their thoughtful comments and suggestions on previous versions of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rodríguez-Arias, D., Tortosa, J.C., Burant, C.J. et al. One or two types of death? Attitudes of health professionals towards brain death and donation after circulatory death in three countries. Med Health Care and Philos 16, 457–467 (2013). https://doi.org/10.1007/s11019-011-9369-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11019-011-9369-1