Abstract
Objective
To characterize the prevalence of and factors associated with clinicians’ prenatal suspicion of a large baby; and to determine whether communicating fetal size concerns to patients was associated with labor and delivery interventions and outcomes.
Methods
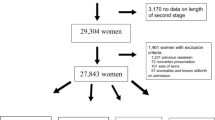
We examined data from women without a prior cesarean who responded to Listening to Mothers III, a nationally representative survey of women who had given birth between July 2011 and June 2012 (n = 1960). We estimated the effect of having a suspected large baby (SLB) on the odds of six labor and delivery outcomes.
Results
Nearly one-third (31.2 %) of women were told by their maternity care providers that their babies might be getting “quite large”; however, only 9.9 % delivered a baby weighing ≥4000 g (19.7 % among mothers with SLBs, 5.5 % without). Women with SLBs had increased adjusted odds of medically-induced labor (AOR 1.9; 95 % CI 1.4–2.6), attempted self-induced labor (AOR 1.9; 95 % CI 1.4–2.7), and use of epidural analgesics (AOR 2.0; 95 % CI 1.4–2.9). No differences were noted for overall cesarean rates, although women with SLBs were more likely to ask for (AOR 4.6; 95 % CI 2.8–7.6) and have planned (AOR 1.8; 95 % CI 1.0–4.5) cesarean deliveries. These associations were not affected by adjustment for gestational age and birthweight.
Conclusions for Practice
Only one in five US women who were told that their babies might be getting quite large actually delivered infants weighing ≥4000 g. However, the suspicion of a large baby was associated with an increase in perinatal interventions, regardless of actual fetal size.
Similar content being viewed by others
Notes
The most common means have been reported as walking or exercise, sexual intercourse and nipple stimulation; with the leading reason for trying to self-induce being a mother’s desire to “get the pregnancy over with” and to “avoid a medical induction.”
References
Martin, J. A, Hamilton, B. E, Ventura, S. J. et al. (2013). Births: Final data for 2011. National Vital Statistics Reports, 62(1), 1–69, 72.
Stotland, N. E., Caughey, A. B., Breed, E. M., et al. (2004). Risk factors and obstetric complications associated with macrosomia. International Journal of Gynaecology and Obstetrics, 87(3), 220–226.
Boulet, S. L., Alexander, G. R., Salihu, H. M., et al. (2003). Macrosomic births in the united states: Determinants, outcomes, and proposed grades of risk. American Journal of Obstetrics and Gynecology, 188(5), 1372–1378.
Rossi, A. C., Mullin, P., & Prefumo, F. (2013). Prevention, management, and outcomes of macrosomia: A systematic review of literature and meta-analysis. Obstetrical and Gynecological Survey, 68(10), 702–709.
Jolly, M. C., Sebire, N. J., Harris, J. P., et al. (2003). Risk factors for macrosomia and its clinical consequences: A study of 350,311 pregnancies. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 111(1), 9–14.
Rouse, D. J., & Owen, J. (2000). Sonography, suspected macrosomia, and prophylactic cesarean: A limited partnership. Clinical Obstetrics and Gynecology, 43(2), 326–334.
American College of Obstetricians and Gynecologists. (2000). ACOG committee opinion no 22: Fetal Macrosomia.
Chauhan, S. P., Grobman, W. A., Gherman, R. A., et al. (2005). Suspicion and treatment of the macrosomic fetus: A review. American Journal of Obstetrics and Gynecology, 193(2), 332–346.
Hoopmann, M., Abele, H., Wagner, N., et al. (2010). Performance of 36 different weight estimation formulae in fetuses with macrosomia. Fetal Diagnosis and Therapy, 27(4), 204–213.
American College of Obstetricians and Gynecologists. (2013). ACOG committee opinion no. 561: Nonmedically indicated early-term deliveries. Obstetrics and Gynecology, 121(4), 911–915.
Boulet, S. L., Alexander, G. R., & Salihu, H. M. (2005). Secular trends in cesarean delivery rates among macrosomic deliveries in the United States, 1989 to 2002. Journal of Perinatology, 25(9), 569–576.
Groom, K. M., Paterson-Brown, S., & Fisk, N. M. (2002). Temporal and geographical variation in UK obstetricians’ personal preference regarding mode of delivery. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 100(2), 185–188.
Gregory, K. D., Korst, L. M., & Platt, L. D. (2001). Variation in elective primary cesarean delivery by patient and hospital factors. American Journal of Obstetrics and Gynecology, 184(7), 1521–1532. (discussion 32–4).
Barber, E. L., Lundsberg, L. S., Belanger, K., et al. (2011). Indications contributing to the increasing cesarean delivery rate. Obstetrics and Gynecology, 118(1), 29–38.
Gonen, R., Bader, D., & Ajami, M. (2000). Effects of a policy of elective cesarean delivery in cases of suspected fetal macrosomia on the incidence of brachial plexus injury and the rate of cesarean delivery. American Journal of Obstetrics and Gynecology, 183(5), 1296–1300.
Vendittelli, F., Riviere, O., & Breart, G. (2012). Is prenatal identification of fetal macrosomia useful? European Journal of Obstetrics, Gynecology, and Reproductive Biology, 161(2), 170–176.
Weeks, J. W., Pitman, T., & Spinnato, J. A, 2nd. (1995). Fetal macrosomia: Does antenatal prediction affect delivery route and birth outcome? American Journal of Obstetrics and Gynecology, 173(4), 1215–1219.
Melamed, N., Yogev, Y., Meizner, I., et al. (2010). Sonographic prediction of fetal macrosomia: The consequences of false diagnosis. Journal of Ultrasound in Medicine, 29(2), 225–230.
Sadeh-Mestechkin, D., Walfisch, A., Shachar, R., et al. (2008). Suspected macrosomia? Better not tell. Archives of Gynecology and Obstetrics, 278(3), 225–230.
Little, S. E, Edlow, A. G., Thomas, A.M., et al. Estimated fetal weight by ultrasound: A modifiable risk factor for cesarean delivery? American Journal of Obstetrics and Gynecology, 207(4), 309 e1–6.
Blackwell, S. C., Refuerzo, J., Chadha, R., et al. Overestimation of fetal weight by ultrasound: Does it influence the likelihood of cesarean delivery for labor arrest? American Journal of Obstetrics and Gynecology, 200(3), 340 e1–3.
Declercq, E. R., Sakala, C., Corry, M. P., et al. (2014). Major survey findings of listening to mothers III: New mothers speak out: report of national surveys of women’s childbearing experiences conducted October–December 2012 and January–April 2013. The Journal of Perinatal Education, 23(1), 17–24.
Declercq, E. R., Sakala, C., Corry, M.P., et al. (2006). Listening to mothers II: Report of the Second National U.S. Survey of women’s childbearing experiences. New York: Childbirth Connection; .
Commission, Joint. (2010). Advancing effective communication, cultural competence, and patient-and family-centered care: A roadmap for hospitals. Oakbrook Terrace: Joint Commission.
Declercq, E. R., Sakala, C., Corry, M. P., et al. (2007). Listening to Mothers II: Report of the Second National U.S. Survey of Women’s Childbearing Experiences: Conducted January–February 2006 for Childbirth Connection by Harris Interactive in partnership with Lamaze International. The Journal of Perinatal Education, 16(4), 15–17.
American Institute of Ultrasound in Medicine. (2003). AIUM Practice Guideline for the performance of an antepartum obstetric ultrasound examination. Journal of Ultrasound in Medicine, 22(10), 1116–1125.
Weiss, J. L., Malone, F. D., Emig, D., et al. (2004). Obesity, obstetric complications and cesarean delivery rate: A population-based screening study. American Journal of Obstetrics and Gynecology, 190(4), 1091–1097.
Reid, E. W., McNeill, J. A., Holmes, V. A., et al. (2014). Women’s perceptions and experiences of fetal macrosomia. Midwifery, 30(4), 456–463.
Poikkeus, P., Saisto, T., Unkila-Kallio, L., et al. (2006). Fear of childbirth and pregnancy-related anxiety in women conceiving with assisted reproduction. Obstetrics and Gynecology, 108(1), 70–76.
Saisto, T., Toivanen, R., Salmela-Aro, K., et al. (2006). Therapeutic group psychoeducation and relaxation in treating fear of childbirth. Acta Obstetricia et Gynecologica Scandinavica, 85(11), 1315–1319.
Nerum, H., Halvorsen, L., Sorlie, T., et al. (2006). Maternal request for cesarean section due to fear of birth: Can it be changed through crisis-oriented counseling? Birth, 33(3), 221–228.
Yawn, B. P., Suman, V. J., & Jacobsen, S. J. (1998). Maternal recall of distant pregnancy events. Journal of Clinical Epidemiology, 51(5), 399–405.
Seidman, D. S., Slater, P. E., Ever-Hadani, P., et al. (1987). Accuracy of mothers’ recall of birthweight and gestational age. British Journal of Obstetrics and Gynaecology, 94(8), 731–735.
Buka, S. L., Goldstein, J. M., Spartos, E., et al. (2004). The retrospective measurement of prenatal and perinatal events: Accuracy of maternal recall. Schizophrenia Research, 71(2–3), 417–426.
Acknowledgments
Dr. Cheng was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Research Training in Prevention and Care of Chronic Illness in Childhood (T32HD075727-01; PI: JA Finkelstein).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cheng, E.R., Declercq, E.R., Belanoff, C. et al. Labor and Delivery Experiences of Mothers with Suspected Large Babies. Matern Child Health J 19, 2578–2586 (2015). https://doi.org/10.1007/s10995-015-1776-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1776-0