Abstract
To explore the association between health care provider advice about weight gain and gestational weight gain. Using data from a prospective cohort study, we explored the association between provider advice about weight gain in pregnancy with weight gain adequacy among 1,454 pregnant women. Provider advice was measured by maternal self-report at 27–30 weeks’ gestation. Linear and Poisson regression were used to explore associations. Seventy-eight percent of the women gained outside current recommendations. Fifty-one percent reported receiving weight gain advice from a health care provider. Adjusted Generalized Linear Model (GLM) estimates showed weak effect of provider advice on inadequate or excessive gain (Relative Risk (RR) 0.96, 95% CI 0.74, 1.26 for inadequate gain and RR 1.01, 95% CI 0.97, 1.06 for excessive gain). There is a need for more women to hear about their targeted weight gains during pregnancy and the present advice that exists does little to influence actual gains. Further studies are warranted to find better strategies for providers to motivate their patients to gain weight within the appropriate ranges.
Similar content being viewed by others
Introduction
The Institute of Medicine (IOM) weight gain guidelines [1] have been widely published and adopted by the American College of Obstetrics and Gynecology and the American Academy of Pediatrics [2]. In spite of this, the majority of pregnant women continue to gain weight outside recommendations [3–5] and these numbers have increased over time [6]. Results from a systematic review demonstrate strong evidence that gaining outside recommended ranges increases the risk of preterm delivery and low birth weight for women with inadequate gain, and high birth weight, macrosomia, cesarean section, and postpartum weight retention among those with excessive gain [7].
Remarkably little is known about why pregnant women gain weight outside the IOM recommendations. Researchers have found that pregnant women who reported being advised about the appropriate amount of weight to gain during pregnancy were more likely to gain within the recommended range than women who did not report receiving such advice [8–11]. However, this association is based on a handful of studies, most of which were conducted prior to or soon after the 1990 IOM guidelines were made public. In 2006, the IOM reported that “despite the availability of the IOM recommendations and an effort to publicize their availability, their use and compliance are not well-understood” [6]. The committee called for future research on the role of provider advice in helping women achieve targeted pregnancy weight gain goals, [6] a recommendation echoed in the systematic evidence-based review on maternal weight gain [7].
The purpose of this study was to determine the proportion of women reporting having received provider advice about weight gain and to examine the association between reported advice and risk for excessive or inadequate pregnancy weight gain.
Methods
Study Design and Sample
Data for this study came from the Pregnancy, Infection, and Nutrition Study 3 (PIN), a longitudinal cohort study of risk factors for preterm birth conducted at the University of North Carolina (UNC) Hospitals in central North Carolina. PIN staff recruited women from prenatal care clinics at their second prenatal visit. Eligible women were English-speaking women less than or equal to 20 weeks’ gestation who were at least 16 years old, had a singleton fetus, planned to continue care at the clinic, and had access to a telephone for interviews. Data on sociodemographics, medical history, current pregnancy, and health behaviors were collected via clinic visits, in-depth phone interviews, and self-administered questionnaires. Between January 2001 and June 2005, a total of 2,006 women were recruited. The Institutional Review Board of the University of North Carolina at Chapel Hill approved all study protocols.
Exposure Measurement: Provider Advice About Pregnancy Weight Gain
Maternal self-report of provider advice about pregnancy weight gain was obtained from a telephone interview administered by a trained interviewer at 27–30 weeks’ gestation. Women were asked to answer yes or no to the following question: “At any time during this pregnancy, has a doctor, nurse, or other health professional given you advice about how much weight you should gain during pregnancy?” Women were also asked to identify the source of provider advice (doctor, nurse, other health professional) and to indicate whether they followed the advice (yes/no).
Outcome Measurement: Adequacy of Pregnancy Weight Gain
Adequacy of gestational weight gain was defined as gaining within predetermined ranges of the 1990 IOM guidelines [12]. We used the older version of the guidelines since they were in use at the time of the study. These guidelines delineate recommended pregnancy weight gain based on a woman’s prepregnancy body mass index (BMI). Self-reported prepregnancy weight and height measurements were collected at the time of recruitment and used to calculate prepregnancy BMI. Women were categorized into BMI categories based on the 1990 IOM cut points: BMI < 19.8 kg/m2 (underweight); BMI 19.8–26.0 kg/m2 (normal weight); BMI 26.1–29.0 kg/m2 (overweight); BMI > 29.0 kg/m2 (obese) [12]. After delivery, gestational weights at each prenatal visit were abstracted from the medical chart and used to determine total gestational weight gain based on gestational age, using a formula described elsewhere [3].
The outcome was explored in three different ways: (1) as a continuous variable of total pregnancy weight gain in kilograms, calculated by subtracting the prepregnancy weight from the last prenatal visit before delivery; (2) as a ratio of observed to expected weight gain, calculated by dividing the total weight gain in kilograms by the expected weight gain for a specific gestational age in kilograms (based on IOM recommendations as described above), such that a value >1 indicates greater than expected gain and a value <1 indicates less than expected gain; and (3) as a categorical variable of inadequate, adequate, or excessive weight gain. For the categorical variable, adequacy was defined based on the expected rate of weight gain (from the IOM pre-pregnancy specific weight gain recommendations) and the 1990 IOM recommended total pregnancy weight gain ranges. We expressed adequacy as the ratio of observed weight gain/expected weight gain and then multiplied by 100 to get a percentage. Inadequate gain was defined as gain below the lowest percent, adequate was within the percentage range, and excessive was gain above the percentage range. The IOM recommendations did not indicate an upper weight gain limit for obese women; thus to categorize obese women into adequacy categories we used the same upper percentage range as for overweight women. Details of the adequacy measure and calculations are described elsewhere [13].
Covariates
Potential confounders included maternal race (African American, Caucasian), age (in years), education level (less than high school, completed high school, and greater than high school), parity (0, 1, 2, and 3 or more children), and poverty level (≤185% of the Federal Poverty Level (FPL), > 185% FPL). We also evaluated pregnancy and maternal health status indicators. These variables were measured using prenatal records, which indicated the presence or absence of gestational diabetes, pregnancy-induced hypertension, preterm labor, vaginal bleeding, pre-existing diabetes, and smoking during pregnancy. Health behaviors included weight cycling, dieting history, and restrictive eating behaviors which were assessed at 27–30 weeks’ gestation using the Revised Restraint Scale [14, 15]. Maternal attitude toward pregnancy weight gain was assessed at 27–30 weeks’ gestation using the Pregnancy Weight Gain Attitude Scale [16].
Potential mediators included diet and physical activity. Dietary values of carbohydrate, protein, fat, and total caloric intake were estimated from a modified version of the Block Food Frequency Questionnaire designed to assess diet during the previous 3 months [17]. Women completed this questionnaire between 24 and 29 weeks’ gestation. In the analysis we used both the continuous forms of the dietary values as well as categorical forms divided into tertiles. Physical activity was assessed at 27–30 weeks’ gestation via a validated questionnaire in which women reported their physical activity in the week prior to the telephone interview [18].
Participants rated their activities that caused at least some increase in heart rate as fairly light, somewhat hard, or hard/very hard, and indicated the length of time they spent engaged in each activity. The length of time and frequency of participation in each activity were multiplied and summed for the week for each of the three intensity levels. Total activity was calculated by adding up the time per week spent in fairly light, somewhat hard, and hard/very hard activities for all activities. Recreational activity was calculated in the same manner but limited to time spent in recreational activities, such as walking (not as a means of transportation), running, swimming, tennis, yoga, etc.
Statistical Analysis
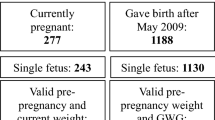
From the 2,006 women who were recruited into PIN, we excluded 233 (11.6%) without sufficient prenatal weight gain data and 213 (10.6%) who did not complete the second phone interview (in which the provider advice question was asked). Of the remaining 1,560 women, we excluded 23 (1.5%) with fetal or infant deaths and 83 (5.3%) who had more than one pregnancy in the cohort, the second (and, in 3 cases, the third) of which was dropped to remove issues of dependency, resulting in a final analysis file of 1,454 women.
Analysis included descriptive statistics. Chi square and t test statistics were used to identify any differences in population characteristics by provider advice and by weight gain adequacy, with statistical significance set at p < 0.05. We hypothesized that dietary intake and physical activity operated as mediators in the causal pathway between advice and pregnancy weight gain. We tested for mediation using both Baron and Kenny’s criteria [19] and the Sobel test for mediation [20], exploring the mediating variables in their continuous and categorical forms and the outcome as total, observed/expected, and adequacy of weight gain.
Maternal race and prepregnancy BMI were identified from the literature [8–10] as potential effect measure modifiers and were tested prior to assessing confounding by comparing the odds ratios for inadequate or excessive gain among women who reported receiving provider advice versus women who reported receiving no provider advice. Effect measure modification was considered present if the Mantel Hanzel test for homogeneity detected a difference in odds ratios between groups (p < 0.1). Race was limited to African American and Caucasian; other races were excluded due to low numbers in the population (n = 132, 9.1%). Prepregnancy BMI was categorized into two groups (underweight/normal weight and overweight/obese) following a sensitivity analysis that found no significant differences when collapsing the four groups into two (results not shown). The socio-demographic, health status, health behavior, and attitude variables were assessed as potential confounders using a backward elimination method; those that did not change the beta coefficient or the relative risk by 10% or more were dropped from the final model.
We used linear regression to examine the outcome in its continuous forms; for the categorical form of the variable, we performed a multivariable analysis using a generalized linear model to estimate the adjusted risk of inadequate or excessive gain associated with provider advice. Inadequate and excessive gains were modeled separately, with adequate gain as the referent variable in each model. Intercooled STATA 9.0 was employed for all statistical analyses.
Results
Table 1 provides descriptive characteristics of the study population, the majority of which was White and over the age of 25 with a greater than high school education level. The sample was comparable to the population served by the hospital at which the births occurred [21]. Less than 25% of the population gained weight within IOM recommendations, while 10% gained less and two-thirds gained more than recommended. When asked at 27–30 weeks’ gestation, 51.8% of the population reported having received provider advice about pregnancy weight gain. When compared to women who reported no advice, those who reported advice were more often of a higher education level and income, nulliparous, to have a history of dieting, and to have a lesser amount of physical activity in the first trimester (p < 0.05). Age, race, marital status, and prepregnancy BMI were not associated with provider advice (Table 1).
Adequacy of Weight Gain
Average total pregnancy weight gain among women who delivered term was 15.0 kg (33.0 lb.) (SD) 6.0 kg (13.2 lb.). The majority gained in excess of the recommendations (Table 1). Adequate gain was lower with higher prepregnancy BMI, while excessive gain tended to be higher with higher BMI (Fig. 1).
Total Weight Gain and the Weight Gain Adequacy Ratio (Observed/Expected Gain)
In the linear regression analysis, a change from no advice to receiving advice resulted in a 0.46 kg (1.01 lb.) lower total pregnancy weight gain (adjusting for maternal race, parity, age, and restrained eating, 95% CI −1.22, 0.30) and a 0.003 lower weight gain adequacy ratio compared to women not reporting having received advice (adjusting for the confounders of maternal race, prepregnancy BMI, age, education level, gestational diabetes, restrained eating, and total and recreational physical activity in the first trimester, 95% CI −0.10, 0.10). Neither result was statistically significant at the p < 0.05 level. Following provider advice showed no association with either total weight gain or the adequacy ratio in the bivariate analysis.
Inadequate and Excessive Weight Gain
Table 2 displays the crude and adjusted relative risks and their respective 95% confidence intervals for both inadequate and excessive weight gain among women with no provider advice compared to women who reported receiving advice. We did not detect effect measure modification by race or prepregnancy BMI and thus one estimate each is reported for total weight gain, the ratio of observed/expected gain, and for inadequate and excessive gain. The crude analysis demonstrated a weak risk for inadequate gain, which became null after accounting for restrained eating and recreational activity in the second trimester. There was a weak effect of provider advice on excessive gain.
Source of Advice and Whether Advice was Followed
Of the 52% of women reporting weight gain advice, 75% reported advice from a doctor, 8% from a nurse and 18% from ‘other health professional’. Ninety-one percent of women reported following advice. After controlling for race and BMI, following advice was associated with a statistically significant lower risk of excessive weight gain (RR = 0.87, 95% CI = 0.78, 0.98). There was no association between type of provider and weight gain adequacy.
Advice and Weight Gain Mediation
Table 3 illustrates the steps undertaken to determine the presence of mediation using the Baron and Kenny criteria [19], with the outcome of total weight gain in kilograms. The potential mediators tested were caloric intake, first-trimester physical activity, and second-trimester physical activity (all self-reported, continuous measures). We also assessed mediation defining the weight gain outcome as observed/expected gain and weight gain adequacy, with mediators measured as total caloric intake in tertiles, and physical activity levels of no activity, below the median, or above the median (results not shown).
The Sobel test statistics varied according to which forms of the pregnancy weight gain and mediating variables we tested, with a total effect of the mediators ranging from −20.4 to 31.5%, none of which were statistically significant (results not shown). Thus neither diet nor physically activity proved to be mediators between provider advice and pregnancy weight gain.
Discussion
The majority of our population gained outside IOM recommendations and most gained excessively. Just over half of the women reported receiving advice from a health care professional about how much weight they should gain. We found no evidence for an association between provider advice and pregnancy weight gain. Contrary to our hypotheses, neither dietary intake nor physical activity proved to be mediators in the causal pathway between advice and weight gain. Possible inaccuracies in self-reported dietary intake and physical activity may have created measurement error and nullified an effect of one or the other variable. It is also possible that an effect exists but that neither the Sobel test nor the Baron and Kenny criteria were able to detect a difference as both approaches are known to be limited by small sample size [22]. More likely, no mediating effect was found because of the lack of main effect, i.e. the lack of association between advice and weight gain.
The proportion of women reporting provider advice about weight gain is similar to results found by Olson and Strawderman [23], higher than Phelan et al. [24]. but lower than other studies [8–10]. With one exception, [25] earlier weight gain studies comprised mainly White women, who were more likely to report receiving advice than women of other races (though we did not find this in our population). Several of the previous studies asked women to report solely about physician advice; given that we queried women about advice from any health care provider and that women interact with multiple providers throughout the course of a pregnancy, one would expect the proportion of those reporting advice to be higher in our sample but this was not the case [24].
Of equal concern is the very low proportion of women with significant health concerns who reported advice. In our sample, only 54% of smokers and 55, 43, 53 and 63% of women with pre-existing hypertension, pre-existing diabetes, gestational hypertension, and gestational diabetes, respectively, reported advice (results derived from Table 1). Such health conditions put pregnant women at increased risk of poor birth outcomes and warrant particular attention to weight gain advice yet a high proportion of these at-risk women reported having received no weight gain advice.
In contrast to earlier studies [8–10, 25, 26], our results provide no evidence for an association between provider advice and pregnancy weight gain. It is possible that we did not detect an effect not because advice is unrelated to weight gain but because the type or quality of advice is critical to noting an effect. Brawarsky et al. [25] found that ‘no physician advice’ versus ‘correct physician advice’ had no effect on excessive gain, but that women who reported advice to gain above IOM recommendations were most likely to gain excessively. Providers may be offering advice, but ineffectively. Although providers may feel weight gain counseling is important, research suggests that many are uncomfortable with weight gain counseling, feel poorly skilled to offer it, and/or feel weight issues are intransigent and unlikely to change with intervention [27]. A possible next step then may be targeting providers for counseling and motivational interviewing skills training [28].
A lack of effect may also mean that women are receiving advice but not following it. Results from focus groups we conducted of 58 White, African American, and Hispanic pregnant women of varying body sizes suggest that women do not follow advice that they view as conflicting and generalized, desiring instead specific, clear, tailored advice (results not yet published). These results suggest that simply being advised to gain within a specific range is not enough to effect behavior change. At least one intervention study which provided education and support to participants provides evidence of this assertion: low-income women in the intervention group gained significantly less weight during pregnancy and retained less weight at 1-year postpartum compared to controls [29].
Our results suggest that provider advice, as provided in routine prenatal care, is not sufficient to help women gain within recommended ranges during pregnancy. In contrast, results from studies of comprehensive weight gain interventions in pregnancy have been somewhat promising [29–32]. In those interventions, women received intensive, individualized counseling about diet and physical activity over a period of time. Intervention results lead us to believe that women would benefit from advice beyond what providers currently offer.
Some practical guidance for providers on how to counsel women has been detailed in earlier publications and includes suggestions for nutrition, physical activity, and weight gain tools and counseling spanning the preconception, prenatal, and postpartum periods [33–35]. It is equally important to recognize that individual providers cannot address pregnancy weight gain alone. Rather, they must be a part of a team effort and “share the care”, involving other staff and making referrals when necessary, for example to nutritionists or WIC counselors [35]. Systems-level issues need also be addressed and could include tools such as electronic medical record prompts to remind providers to inquire about weight gain.
This study has both notable strengths and caveats. The study’s prospective nature limited recall bias and enabled us to capture women’s experiences with advice while pregnant. The richness of the data also allowed us to examine a multitude of covariates, such as diet, physical activity, restrained eating, and general health indicators of pre-existing diabetes and hypertension that are largely non-existent in other studies of advice and weight gain. Importantly, this study was unique in exploring potential mediators in the pathway to gestational weight gain.
As in others, our study was limited to maternal self-report of advice. We have neither provider input nor an objective record of whether advice was provided, what it was, or how it was offered. This limits our ability to identify links between the nature of advice and whether it is recalled, but does not undermine the important result that, whether provided or not, women did not hear the advice. The evidence that half of women report receiving no weight gain advice is in and of itself cause for concern.
Another limitation is the self-reported prepregnancy weight and height, leading to potential misclassification of BMI. As is common with pregnancy cohorts, measuring height and weight prior to pregnancy was not feasible in this study. Prior studies show reasonable accuracy of self-reported weight in similar populations [36]. In our study, some of the misclassification risk is reduced as a result of combining underweight/normal weight together and overweight/obese together, creating a measure less sensitive to slight under or over-reporting. Of potential concern would be the overweight women being misclassified as normal weight [37].
The collective findings of earlier research [8–11] suggest that advice is an important influence on women’s behavior. Future research on weight gain advice would benefit from qualitative study which is well-suited to in-depth examination of personal experiences. It could provide greater insight into what women think of weight-related issues in pregnancy, how they feel about the advice they receive, and why they do or do not follow it. Given limited research on the provider’s perspective, qualitative investigation could aid in the development of a questionnaire for a large sample of providers, one that could assess their current practices as well as counseling needs and comfort level. Such inquiry could prove important as exploratory research with the ultimate aim of informing effective interventions to aid women in achieving healthy pregnancy weight gain.
References
Rasmussen, K., & Yaktine, A. (Eds.). (2009). Weight gain during pregnancy: Reexamining the guidelines. Committee to reexamine IOM pregnancy weight gain guidelines. Washington, DC: National Academies Press.
American Academy of Pediatrics, American College of Obstetricians and Gynecologists, & March of Dimes Birth Defects Foundation. (1988). Guidelines for perinatal care (6th ed.). Elk Grove Village, Illinois: American Academy of Pediatrics.
Siega-Riz, A. M., Adair, L. S., & Hobel, C. J. (1994). Institute of medicine maternal weight gain recommendations and pregnancy outcome in a predominantly Hispanic population. Obstetrics and Gynecology, 84(4), 565–573.
Devader, S. R., Neeley, H. L., Myles, T. D., & Leet, T. L. (2007). Evaluation of gestational weight gain guidelines for women with normal prepregnancy body mass index. Obstetrics and Gynecology, 110(4), 745–751.
Caulfield, L. E., Witter, F. R., & Stoltzfus, R. J. (1996). Determinants of gestational weight gain outside the recommended ranges among black and white women. Obstetrics and Gynecology, 87(5 Pt 1), 760–766.
National Research Council. (2007). Influence of pregnancy weight on maternal and child health: Worskhop Report. Committee on the Impact of Pregnancy Weight on Maternal and Child Health. Board on Children, Youth, and Families, Division of Behavioral and Social Sciences and Education and Food and Nutrition Board, Institute of Medicine. Washington, DC: The National Academies Press.
Viswanathan, M., Siega-Riz, A. M., Moos, M. K., Deierlein, A., Mumford, S., Knaack, J., et al. (2008). Outcomes of maternal weight gain. Evidence Report Technology Assessment (Full Rep), 168, 1–223.
Cogswell, M. E., Scanlon, K. S., Fein, S. B., & Schieve, L. A. (1999). Medically advised, mother’s personal target, and actual weight gain during pregnancy. Obstetrics and Gynecology, 94(4), 616–622.
Taffel, S. M., & Keppel, K. G. (1986). Advice about weight gain during pregnancy and actual weight gain. American Journal of Public Health, 76(12), 1396–1399.
Taffel, S. M., Keppel, K. G., & Jones, G. K. (1933). Medical advice on maternal weight gain and actual weight gain. Results from the, 1988 National maternal and infant health survey. Annals of the New York Academy of Sciences, 1993(678), 293–305.
Stotland, N. E., Haas, J. S., Brawarsky, P., Jackson, R. A., Fuentes-Afflick, E., & Escobar, G. J. (2005). Body mass index, provider advice, and target gestational weight gain. Obstetrics and Gynecology, 105(3), 633–638.
Institute of Medicine. (1990). Nutrition during pregnancy. Part I weight gain. Washington, DC: National Academy Press.
Bodnar, L. M., Siega-Riz, A. M., Arab, L., Chantala, K., & McDonald, T. (2004). Predictors of pregnancy and postpartum haemoglobin concentrations in low-income women. Public Health Nutrition, 7(6), 701–711.
Ruderman, A. J. (1983). The restraint scale: A psychometric investigation. Behaviour Research and Therapy, 21(3), 253–258.
Herman, C. P., & Mack, D. (1975). Restrained and unrestrained eating. Journal of Personality, 43(4), 647–660.
Palmer, J. L., Jennings, G. E., & Massey, L. (1985). Development of an assessment form: Attitude toward weight gain during pregnancy. Journal of the American Dietetic Association, 85(8), 946–949.
Laraia, B. A., Bodnar, L. M., & Siega-Riz, A. M. (2007). Pregravid body mass index is negatively associated with diet quality during pregnancy. Public Health Nutrition, 10(9), 920–926.
Evenson, K. R., & Wen, F. (2010). Measuring physical activity among pregnant women using a structured one-week recall questionnaire: Evidence for validity and reliability. The international journal of behavioral nutrition and physical activity, 7, 21–32.
Baron, R., & Kenny, D. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182.
MacKinnon, D. P., Lockwood, C. M., Hoffman, J. M., West, S. G., & Sheets, V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83–104.
Savitz, D. A., Dole, N., Kaczor, D., Herring, A. H., Siega-Riz, A. M., Kaufman, J., et al. (2005). Probability samples of area births versus clinic populations for reproductive epidemiology studies. Paediatric and Perinatal Epidemiology, 19(4), 315–322.
Fritz, M. S., & Mackinnon, D. P. (2007). Required sample size to detect the mediated effect. Psychological Science, 18(3), 233–239.
Olson, C. M., & Strawderman, M. S. (2003). Modifiable behavioral factors in a biopsychosocial model predict inadequate and excessive gestational weight gain. Journal of the American Dietetic Association, 103(1), 48–54.
Phelan, S., Phipps, M. G., Abrams, B., Darroch, F., Schaffner, A., & Wing, R. R. (2011). Practitioner advice and gestational weight gain. Journal of Womens Health (Larchmt), 20(4), 585–591.
Brawarsky, P., Stotland, N. E., Jackson, R. A., Fuentes-Afflick, E., Escobar, G. J., Rubashkin, N., et al. (2005). Pre-pregnancy and pregnancy-related factors and the risk of excessive or inadequate gestational weight gain. International Journal of Gynaecology and Obstetrics, 91(2), 125–131.
Strychar, I. M., Chabot, C., Champagne, F., Ghadirian, P., Leduc, L., Lemonnier, M. C., et al. (2000). Psychosocial and lifestyle factors associated with insufficient and excessive maternal weight gain during pregnancy. Journal of the American Dietetic Association, 100(3), 353–356.
Stotland, N. E., Gilbert, P., Bogetz, A., Harper, C. C., Abrams, B., & Gerbert, B. (2010). Preventing excessive weight gain in pregnancy: How do prenatal care providers approach counseling? Journal of Womens Health (Larchmt), 19(4), 807–814.
Resnicow, K., DiIorio, C., Soet, J. E., Ernst, D., Borrelli, B., & Hecht, J. (2002). Motivational interviewing in health promotion: It sounds like something is changing. Health Psychology, 21(5), 444–451.
Olson, C. M., Strawderman, M. S., & Reed, R. G. (2004). Efficacy of an intervention to prevent excessive gestational weight gain. American Journal of Obstetrics and Gynecology, 191(2), 530–536.
O’Toole, M. L., Sawicki, M. A., & Artal, R. (2003). Structured diet and physical activity prevent postpartum weight retention. Journal of Womens Health (Larchmt), 12(10), 991–998.
Wolff, S., Legarth, J., Vangsgaard, K., Toubro, S., & Astrup, A. (2008). A randomized trial of the effects of dietary counseling on gestational weight gain and glucose metabolism in obese pregnant women. International Journal of Obesity (Lond), 32(3), 495–501.
Polley, B. A., Wing, R. R., & Sims, C. J. (2002). Randomized controlled trial to prevent excessive weight gain in pregnant women. International Journal of Obesity and Related Metabolic Disorders, 26(11), 1494–1502.
Widen, E., & Siega-Riz, A. M. (2010). Prenatal nutrition: A practical guide for assessment and counseling. Journal of Midwifery and Womens Health, 55(6), 540–549.
Siega-Riz, A. M., Deierlein, A., & Stuebe, A. (2010). Implementation of the new Institute of Medicine gestational weight gain guidelines. Journal of Midwifery and Womens Health, 55(6), 512–519.
Siega-Riz, A. M., & Ciannini, C. (2009). Promoting healthy weight in women: What the physician can do to help. North Carolina Medical Journal, 70(5), 449–453.
Brunner Huber, L. R. (2007). Validity of self-reported height and weight in women of reproductive age. Maternal and Child Health Journal, 11(2), 137–144.
Bodnar, L. M., Siega-Riz, A. M., Simhan, H. N., Diesel, J. C., & Abrams, B. (2010). The impact of exposure misclassification on associations between prepregnancy BMI and adverse pregnancy outcomes. Obesity (Silver Spring), 18(11), 2184–2190.
Acknowledgments
This study received support from the National Institute of Child Health and Human. Development, National Institutes of Health (HD37584, HD39373), the National Institute of Diabetes and Digestive and Kidney Diseases (DK61981, DK56350), and the Carolina Population Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferrari, R.M., Siega-Riz, A.M. Provider Advice About Pregnancy Weight Gain and Adequacy of Weight Gain. Matern Child Health J 17, 256–264 (2013). https://doi.org/10.1007/s10995-012-0969-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-012-0969-z