Abstract
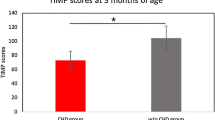
Brain maturation in 1–36 month old children suffering from congenital cardiopathologies was assessed after a study of psychomotor development. The Rogers’ test (Rogers et al., Developmental programming for infants and young children. Volume 2. Early intervention developmental profile, Revised edition, ESL/ELT Michigan, Ann Arbor, 1981) was applied to 65 children, of whom 21 presented with simple cardiopathologies (CpS) and 22 with complex cardiopathologies (CpC). All children were matched by age, sex and socioeconomic status to 22 healthy children in a control group (C). Mean differences between the three groups were established by applying the Kruskal–Wallis test, and mean differences between the C and CpS/CpC groups were determined using the Mann–Whitney test. The proportion of cases evaluated as “low” in each group was calculated by applying the Rogers’ test, and a test of proportion differences was applied between the C and CpS/CpC groups. CpS children performed similarly to the C, whereas CpC children scored significantly lower than C children on all variables. It is highly likely that the suboptimal psychomotor performance observed in CpC children was due to compromised hemodynamics and related to subclinical immaturity of cerebral development.

Similar content being viewed by others
References
Bellinger, D. C., Wypij, D., Duplessis, A. J., Rappaport, L. A., Jonas, R. A., Wernovsky, G., et al. (2003). Neurodevelopmental status at eight years in children with dextro-transposition of the great arteries: The Boston Circulatory Arrest Trial. Journal of Thoracic and Cardiovascular Surgery, 126, 1385–1396.
Bellinger, D. C., Wypij, D., Kuban, K. C., Rappaport, L. A., Hickey, P. R., Wernovsky, G., et al. (1999). Developmental and neurological status of children at 4 years of age after heart surgery with hypothermic circulatory arrest or low-flow cardiopulmonary bypass. Circulation, 100, 526–532.
Brosig, C. L., Mussatto, K. A., Kuhn, E. M., & Tweddell, J. S. (2007). Psychosocial outcomes for preschool children and families after surgery for complex congenital heart disease. Pediatric Cardiology, 28, 255–262.
Daliento, L., Mazzotti, E., Mongillo, E., Rotundo, M., & Dalla Volta, S. (2002). Life expectancy and quality of life in adult patients with congenital heart disease. Italian Heart Journal, 3, 339–347.
Galli, K., Kimmerman, R. A., Jarvik, G. P., Wernovsky, G., Kuypers, M. K., Clancy, R. R., et al. (2004). Periventricular leukomalacia is common after neonatal cardiac surgery. Journal of Thoracic Cardiovascular Surgery, 127, 692–704.
Gillum, R. F. (1994). Epidemiology of congenital heart disease in the United States. American Heart Journal, 127, 919–927.
Hoffman, J. I., & Kaplan, S. (2002). The incidence of congenital heart disease. Journal of the American College of Cardiology, 39, 1890–1900.
Hövels-Gürich, H. H., Konrad, K., Skorzenski, D., Herpertz-Dahlmann, B., Messmer, B. J., & Seghaye, M. C. (2007). Attentional dysfunction in children after corrective cardiac surgery in infancy. Annals of Thoracic Surgery, 83, 1425–1430.
Hövels-Gürich, H. H., Seghaye, M. C., Däbritz, S., Messmer, B. J., & von Bernuth, G. (1997). Cognitive and motor development in preschool and school-aged children after neonatal arterial switch operation. Journal of Thoracic Cardiovascular Surgery, 114, 578–585.
Hövels-Gürich, H. H., Seghaye, M. C., Schnitker, R., Wiesner, M., Huber, W., Minkenberg, R., et al. (2002). Long-term neurodevelopmental outcomes in school-aged children after neonatal arterial switch operation. Journal of Thoracic Cardiovascular Surgery, 124, 448–458.
Hövels-Gürich, H. H., Seghaye, M. C., Sigler, M., Kotlarek, F., Bartl, A., Neuser, J., et al. (2001). Neurodevelopmental outcome related to cerebral risk factors in children after neonatal arterial switch operation. Annals of Thoracic Surgery, 71, 881–888.
Kurth, C. D., Steven, J. L., Montenegro, L. M., Watzman, H. M., Gaynor, J. W., Spray, T. L., et al. (2001). Cerebral oxygen saturation before congenital heart surgery. Annals of Thoracic Surgery, 72, 187–192.
Licht, D. J., Agner, S., Montenegro, L. M., Nicolson, S. C., Silvestre, D., Tabbutt, S., et al. (2006). Preoperative MRI abnormalities are common in full-term infants with severe CHD and resemble lesions in pre-term infants. Neuropediatrics, 37(Suppl 1), S1–S183.
Licht, D. J., Shera, D. M., Clancy, R. R., Wernovsky, G., Montenegro, L. M., Nicolson, S. C., et al. (2009). Brain maturation is delayed in infants with complex congenital heart defects. Journal of Thoracic Cardiovascular Surgery, 137, 529–537.
Limperopoulos, C., Majnemer, A., Shevell, M. I., Rohlicek, C., Rosenblatt, B., Tchervenkov, C., et al. (2002). Predictors of developmental disabilities after open-heart surgery in young children with congenital heart defects. Journal of Pediatrics, 141, 51–58.
Limperopoulos, C., Majnemer, A., Shevell, M. I., Rosenblatt, B., Rohlicek, C., & Tchervenkov, C. (1999). Neurologic status of newborns with congenital heart defects before open-heart surgery. Pediatrics, 103, 402–408.
Limperopoulos, C., Majnemer, A., Shevell, M. I., Rosenblatt, B., Rohlicek, C., Tchervenkov, C., et al. (2001). Functional limitations in young children with congenital heart defects after cardiac surgery. Pediatrics, 108, 1325–1331.
Mahle, W. T., & Wernovsky, G. (2001). Long-term developmental outcome of children with complex congenital heart disease. Clinical Perinatology, 28, 235–247.
Majnemer, A., Limperopoulos, C., Shevell, M., Rohlicek, C., Rosenblatt, B., & Tchervenkov, C. (2008). Developmental and functional outcomes at school entry in children with congenital heart defects. Journal of Pediatrics, 153, 55–60.
Majnemer, A., Limperopoulos, C., Shevell, M., Rosenblatt, B., Rohlicek, C., & Tchervenkov, C. (2006). Long-term neuromotor outcome at school entry of infants with congenital heart defects requiring open-heart surgery. Journal of Pediatrics, 148, 72–77.
Massaro, A. N., El-Dib, M., Glass, P., & Aly, H. (2008). Factors associated with adverse neurodevelopmental outcomes in infants with congenital heart diseases. Brain Development, 30, 437–446.
McQuillen, P. S., Barkovich, A. J., Hamrick, S. E., Perez, M., Ward, P., Glidden, D. V., et al. (2007). Temporal and anatomic risk profile of brain injury with neonatal repair of congenital heart defects. Stroke, 38, 736–741.
Mendieta-Alcántara, G. G., Otero-Ojeda, G. A., Motolinía, R., Colmenero, M., Pliego-Rivero, F. B., Fernández, T., et al. (2011). Alteraciones electroencefalográficas en niños con cardiopatías congénitas severas. Revista Ecuatoriana de Neurología, 20, 60–67.
Miatton, M., De Wolf, D., François, K., Thiery, E., & Vingerhoets, G. (2006). Neurocognitive consequences of surgically corrected congenital heart defects: A review. Neuropsychology Review, 16, 65–85.
Miatton, M., De Wolf, D., François, K., Thiery, E., & Vingerhoets, G. (2007a). Intellectual, neuropsychological, and behavioral functioning in children with tetralogy of Fallot. Journal of Thoracic and Cardiovascular Surgery, 133, 449–455.
Miatton, M., De Wolf, D., François, K., Thiery, E., & Vingerhoets, G. (2007b). Neuropsychological performance in school-aged children with surgically corrected congenital heart disease. Journal of Pediatrics, 151, 73–78.
Miller, S. P., McQuillen, P. S., Hamrick, S., Xu, D., Glidden, D. V., Charlton, N., et al. (2007). Abnormal brain development in newborns with congenital heart disease. New England Journal of Medicine, 357, 1928–1938.
Oates, R. K., Simpson, J. M., Cartmill, T. B., & Turnbull, J. A. (1995). Intellectual function and age of repair in cyanotic congenital heart disease. Archives of Diseases in Childhood, 72, 298–301.
Palencia, R. (2002). Complicaciones neurológicas del paciente con cardiopatía. Revista de Neurología, 35, 279–285.
Palmen, M., de Jong, P. L., Klieverik, L. M. A., Venema, A. C., Meijboom, F. J., & Bogers, J. J. C. (2008). Long-term follow-up after repair of Ebstein’s anomaly. European Journal of Cardio-Thoracic Surgery, 34, 48–54.
Rogers, S. J., Donovan, C. M., D’Eugenio S., Brown, S. L., Lynch, E. W., Moersch, M. S., et al. (1981). Developmental programming for infants and young children. Volume 2. Early intervention developmental profile (Revised ed.). Ann Arbor, MI: ESL/ELT Michigan.
Sarajuuri, A., Jokinen, E., Puosi, R., Eronen, M., Mildh, L., Mattila, I., et al. (2007). Neurodevelopmental and neuroradiologic outcomes in patients with univentricular heart aged 5 to 7 years: Related risk factor analysis. Journal of Thoracic and Cardiovascular Surgery, 133, 1524–1532.
Sharma, R., Choudary, S. K., Mohan, M. R., Padma, M. V., Jain, S., Bhardwaj, M., et al. (2000). Neurological evaluation and intelligence testing in the child with operated congenital heart disease. Annals of Thoracic Surgery, 70, 575–581.
Shillingford, A. J., Glanzman, M. M., Ittenbach, R. F., Clancy, R. R., Gaynor, J. W., & Wernovsky, G. (2008). Inattention, hyperactivity, and school performance in a population of school-age children with complex congenital heart disease. Pediatrics, 121, 759–767.
Simons, J. S., Glidden, R., Sheslow, D., & Pizarro, C. (2010). Intermediate neurodevelopmental outcome after repair of Ventricular Septal Defect. Annals of Thoracic Surgery, 90, 1586–1592.
Wernovsky, G., Shillingford, A. J., & Gaynor, J. W. (2005). Central nervous system outcomes in children with complex congenital heart disease. Current Opinion in Cardiology, 20, 94–99.
Wernovsky, G., Stiles, K. M., Grauvreau, K., Gentles, T. L., duPlessis, A. J., Bellinger, D. C., et al. (2000). Cognitive development after the Fontan operation. Circulation, 102, 883–889.
Wray, J., & Sensky, T. (1999). Controlled study of preschool development after surgery for congenital heart disease. Archives of Diseases in Childhood, 80, 511–516.
Wray, J., & Sensky, T. (2001). Congenital heart disease and cardiac surgery in childhood: Effects on cognitive function and academic ability. Heart, 85, 687–691.
Wren, C., & O’Sullivan, J. J. (2001). Survival with congenital heart disease and need for follow-up in adult life. Heart, 85, 438–443.
Wright, M., & Nolan, T. (1994). Impact of cyanotic heart disease on school performance. Archives of Diseases in Childhood, 71, 64–70.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Porcayo-Mercado, M.R., Otero-Ojeda, G.A., Pliego-Rivero, F.B. et al. Neurobehavioral Assessment of Children Presenting Diverse Congenital Cardiopathologies. J Clin Psychol Med Settings 20, 71–78 (2013). https://doi.org/10.1007/s10880-012-9314-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-012-9314-3