Abstract
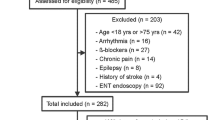
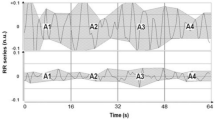
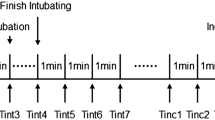
Noxious stimulation influences the autonomic nervous system activity. Sympathetic tone monitoring is currently used to assess the adequacy of the balance between nociception and anti-nociception during general anesthesia. The Surgical Plethysmographic Index (SPI) and the EBMi software (Custos©) are commercial devices that use different algorithms to measure it. We aimed at determining whether those devices provide similar information during routine surgical procedures under general anesthesia. Data acquired during a previously published study in patients undergoing surgery under general anesthesia were retrospectively analyzed and passed through the EBMi software. The occurrence of EBMi alarms of increased sympathetic tone was compared to the occurrence of SPI values ≥ 60, a commonly recommended intraoperative SPI threshold. Trends in classical parameters of sympathetic tone during the 5 min preceding a SPI ≥ 60, namely blood pressure, heart rate, and plethysmographic pulse amplitude were assessed. SPI ≥ 60 episodes (n = 307) were more frequent than EBMi alerts (n = 240). Approximately 70% of EBMi alerts occurred during periods where the SPI was below 60. Among all episodes of SPI ≥ 60, absence of any EBMi alerts was much more frequent than the inverse. A majority, but not all SPI ≥ 60 episodes were consistently preceded by an increase in heart rate and/or a decrease in pulse amplitude. Blood pressure did not significantly change before SPI ≥ 60. Longer SPI ≥ 60 episodes were associated with lower anti-nociception anesthetic regimen. Different methods of sympathetic tone assessment during general anesthesia provide conflicting information. Prospective studies should be undertaken to clarify the clinical indications of both techniques.


Similar content being viewed by others
References
Kovac AL. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. J Clin Anesth. 1996;8:63–79.
Rantanen M, Yppärilä-Wolters H, van Gils M, Yli-Hankala A, Huiku M, Kymäläinen M, et al. Tetanic stimulus of ulnar nerve as a predictor of heart rate response to skin incision in propofol-remifentanil anaesthesia. Br J Anaesth. 2007;99:509–13.
Defresne A, Barvais L, Clement F, Bonhomme V. Standardised noxious stimulation-guided individual adjustment of remifentanil target-controlled infusion to prevent haemodynamic responses to laryngoscopy and surgical incision: A randomised controlled trial. Eur J Anaesthesiol. 2018;35:173–83.
Geisz-Everson MA, Wren K, Kennedy L. Asystole during laryngoscopy of a patient with pleural and pericardial effusions: a case report. AANA J. 2008;76:25–7.
Defresne A, Bonhomme V. Multimodal Monitoring. In: Prabhakar H, editor. Essent. Neuroanesthesia. 1st ed. London: Elsevier Inc.; 2017. pp. 161–80.
Funcke S, Sauerlaender S, Pinnschmidt HO, Saugel B, Bremer K, Reuter DA, et al. Validation of Innovative Techniques for Monitoring Nociception during General Anesthesia. Anesthesiology. 2017;127:272–83.
Huiku M, Uutela K, van Gils M, Korhonen I, Kymäläinen M, Meriläinen P, et al. Assessment of surgical stress during general anaesthesia. Br J Anaesth. 2007;98:447–55.
Barvais L, Engelman E, Eba JM, Coussaert E, Cantraine F, Kenny GN. Effect site concentrations of remifentanil and pupil response to noxious stimulation. Br J Anaesth. 2003;91:347–52.
Edry R, Recea V, Dikust Y, Sessler DI. Preliminary intraoperative validation of the nociception level index: a noninvasive nociception monitor. Anesthesiology. 2016;125:193–203.
Chen X, Thee C, Gruenewald M, Wnent J, Illies C, Hoecker J, et al. Comparison of surgical stress index-guided analgesia with standard clinical practice during routine general anesthesia: a pilot study. Anesthesiology. 2010;112:1175–83.
Defresne A, Harrison M, Bonhomme V. Clinical pertinence and diagnostic accuracy of an evidence-based monitoring system: Custos. Eur J Anaesthesiol. 2016;33:590–2.
Connor CW, Gohil B, Harrison MJ. Triggering of systolic arterial pressure alarms using statistics-based versus threshold alarms. Anaesthesia. 2009;64:131–5.
Raymer KE, Bergström J, Nyce JM. Anaesthesia monitor alarms: a theory-driven approach. Ergonomics. 2012;55:1487–501.
Harrison MJ, Scott-Weekly R, Zacharias M. The qualitative detection of decreases in cardiac output. Comput Biol Med. 2015;58:85–90.
Harrison MJ, Connor CW. Statistics-based alarms from sequential physiological measurements. Anaesthesia. 2007;62:1015–23.
Gruenewald M, Meybohm P, Ilies C, Höcker J, Hanss R, Scholz J, et al. Influence of different remifentanil concentrations on the performance of the surgical stress index to detect a standardized painful stimulus during sevoflurane anaesthesia. Br J Anaesth. 2009;103:586–93.
Wennervirta J, Hynynen M, Koivusalo AM, Uutela K, Huiku M, Vakkuri A. Surgical stress index as a measure of nociception/antinociception balance during general anesthesia. Acta Anaesthesiol Scand. 2008;52:1038–45.
Paloheimo MPJ, Sahanne S, Uutela KH. Autonomic nervous system state: The effect of general anaesthesia and bilateral tonsillectomy after unilateral infiltration of lidocaine. Br J Anaesth. 2010;104:587–95.
Gruenewald M, Willms S, Broch O, Kott M, Steinfath M, Bein B. Sufentanil administration guided by surgical pleth index vs standard practice during sevoflurane anaesthesia: a randomized controlled pilot study. Br J Anaesth. 2014;112:898–905.
Park JH, Lim BG, Kim H, Lee IO, Kong MH, Kim NS. Comparison of surgical pleth index-guided analgesia with conventional analgesia practices in children: a randomized controlled trial. Anesthesiology. 2015;122:1280–7.
Ahonen J, Jokela R, Uutela K, Huiku M. Surgical stress index reflects surgical stress in gynaecological laparoscopic day-case surgery. Br J Anaesth. 2007;98:456–61.
Höcker J, Broch O, Gräsner JT, Gruenewald M, Ilies C, Steinfath M, et al. Surgical stress index in response to pacemaker stimulation or atropine. Br J Anaesth. 2010;105:150–4.
Bonhomme V, Uutela K, Hans G, Maquoi I, Born JD, Brichant JF, et al. Comparison of the surgical Pleth Index™ with haemodynamic variables to assess nociception-anti-nociception balance during general anaesthesia. Br J Anaesth. 2011;106:101–11.
Ilies C, Gruenewald M, Ludwigs J, Thee C, Höcker J, Hanss R, et al. Evaluation of the surgical stress index during spinal and general anaesthesia. Br J Anaesth. 2010;105:533–7.
Hans P, Verscheure S, Uutela K, Hans G, Bonhomme V. Effect of a fluid challenge on the surgical pleth index uring stable propofol-emifentanil anaesthesia. Acta Anaesthesiol Scand. 2012;56:787–96.
Acknowledgements
This study was supported by the Department of Anaesthesia and ICM, Liege University Hospital, Liege, Belgium, by the University Department of Anaesthesia and ICM, CHR Citadelle, Liege, Belgium, and by the Department of Anesthesiology, Erasme University Hospital, Université Libre de Bruxelles (ULB), Brussels, Belgium. The authors want to warmly thank Kimmo Uutela from GE Healthcare Finland Oy (Helsinki, Finland) for help in data extraction.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Michael Harrison is one of the designers of the EBMi software. The other authors declare that they have no conflict of interest.
Ethical approval
All procedures performed on human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study is a retrospective analysis of data acquired during a previously published study, for which Ethics Committee approval was obtained. The initial study was registered at Clinicaltrials.gov, NCT: 02884310; https://clinicaltrials.gov/ct2/show/NCT02884310. Although formal consent is not required for retrospective studies, informed consent was obtained from all individual participants included in the study.
Additional information
An abstract related to this work has been submitted to the ANZCA ASM 2018 (https://asm.anzca.edu.au/) for possible presentation, and its evaluation is still under progress.
Rights and permissions
About this article
Cite this article
Defresne, A., Harrison, M., Clement, F. et al. Two different methods to assess sympathetic tone during general anesthesia lead to different findings. J Clin Monit Comput 33, 463–469 (2019). https://doi.org/10.1007/s10877-018-0175-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0175-7