Abstract
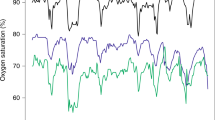
Alterations in arterial blood oxygen saturation, heart rate (HR), and respiratory rate (RR) are strongly associated with intra-hospital cardiac arrests and resuscitations. A wireless, easy-to-use, and comfortable method for monitoring these important clinical signs would be highly useful. We investigated whether the Nellcor™ OxiMask MAX-FAST forehead sensor could provide data for vital sign measurements when located at the distal forearm instead of its intended location at the forehead to provide improved comfortability and easy placement. In a prospective setting, we recruited 30 patients undergoing surgery requiring postoperative care. At the postoperative care unit, patients were monitored for two hours using a standard patient monitor and with a study device equipped with a Nellcor™ Forehead SpO2 sensor. The readings were electronically recorded and compared in post hoc analysis using Bland–Altman plots, Spearman’s correlation, and root-mean-square error (RMSE). Bland–Altman plot showed that saturation (SpO2) differed by a mean of −0.2 % points (SD, 4.6), with a patient-weighted Spearman’s correlation (r) of 0.142, and an RMSE of 4.2 points. For HR measurements, the mean difference was 0.6 bpm (SD, 2.5), r = 0.997, and RMSE = 1.8. For RR, the mean difference was −0.5 1/min (4.1), r = 0.586, and RMSE = 4.0. The SpO2 readings showed a low mean difference, but also a low correlation and high RMSE, indicating that the Nellcor™ saturation sensor cannot reliably assess oxygen saturation at the forearm when compared to finger PPG measurements.


Similar content being viewed by others
References
Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990;98:1388–92.
Jones DA, DeVita MA, Bellomo R. Rapid-response teams. N Engl J Med. 2011;365:139–46.
Fukushima H, Kawanaka H, Bhuiyan MS, Oguri K. Estimating heart rate using wrist-type Photoplethysmography and acceleration sensor while running. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:2901–4.
Renevey P, Sola J, Theurillat P, Bertschi M, Krauss J, Andries D, Sartori C. Validation of a wrist monitor for accurate estimation of RR intervals during sleep. Conf Proc IEEE Eng Med Biol Soc. 2013;2013:5493–6.
Zhang Z, Pi Z, Liu B. TROIKA: a general framework for heart rate monitoring using wrist-type photoplethysmographic signals during intensive physical exercise. IEEE Trans Biomed Eng. 2015;62:522–31.
Nesseler N, Frenel JV, Launey Y, Morcet J, Malledant Y, Seguin P. Pulse oximetry and high-dose vasopressors: a comparison between forehead reflectance and finger transmission sensors. Intensive Care Med. 2012;38:1718–22.
Sugino S, Kanaya N, Mizuuchi M, Nakayama M, Namiki A. Forehead is as sensitive as finger pulse oximetry during general anesthesia. Can J Anaesth. 2004;51:432–6.
Agashe GS, Coakley J, Mannheimer PD. Forehead pulse oximetry: headband use helps alleviate false low readings likely related to venous pulsation artifact. Anesthesiology. 2006;105:1111–6.
Schallom L, Sona C, McSweeney M, Mazuski J. Comparison of forehead and digit oximetry in surgical/trauma patients at risk for decreased peripheral perfusion. Heart Lung. 2007;36:188–94.
Safar H, El-Dash H. Pulse oximetry: Could wrist and ankle be alternative placement sites? Clin Pediatr (Phila). 2015;54:1375–9.
Phattraprayoon N, Sardesai S, Durand M, Ramanathan R. Accuracy of pulse oximeter readings from probe placement on newborn wrist and ankle. J Perinatol. 2012;32:276–80.
Nilsson L, Goscinski T, Kalman S, Lindberg LG, Johansson A. Combined photoplethysmographic monitoring of respiration rate and pulse: a comparison between different measurement sites in spontaneously breathing subjects. Acta Anaesthesiol Scand. 2007;51:1250–7.
Wiklund L, Hok B, Stahl K, Jordeby-Jonsson A. Postanesthesia monitoring revisited: frequency of true and false alarms from different monitoring devices. J Clin Anesth. 1994;6:182–8.
Gaucher A, Frasca D, Mimoz O, Debaene B. Accuracy of respiratory rate monitoring by capnometry using the Capnomask(R) in extubated patients receiving supplemental oxygen after surgery. Br J Anaesth. 2012;1(08):316–20.
Meredith DJ, Clifton D, Charlton P, Brooks J, Pugh CW, Tarassenko L. Photoplethysmographic derivation of respiratory rate: a review of relevant physiology. J Med Eng Technol. 2012;36:1–7.
Johansson A, Öberg PÅ. Estimation of respiratory volumes from the photoplethysmographic signal. Part I: experimental results. Med Biol Eng Comput. 1999;37:42–7.
Dash S, Shelley KH, Silverman DG, Chon KH. Estimation of respiratory rate from ECG, photoplethysmogram, and piezoelectric pulse transducer signals: a comparative study of time-frequency methods. IEEE Trans Biomed Eng. 2010;57:1099–107.
Lazaro J, Gil E, Bailon R, Minchole A, Laguna P. Deriving respiration from photoplethysmographic pulse width. Med Biol Eng Comput. 2013;51:233–42.
Charlton PH, Bonnici T, Tarassenko L, Clifton DA, Beale R, Watkinson PJ. An assessment of algorithms to estimate respiratory rate from the electrocardiogram and photoplethysmogram. Physiol Meas. 2016;37:610–26.
Nilsson L, Johansson A, Kalman S. Monitoring of respiratory rate in postoperative care using a new photoplethysmographic technique. J Clin Monit Comput. 2000;16:309–15.
Addison PS, Watson JN, Mestek ML, Ochs JP, Uribe AA, Bergese SD. Pulse oximetry-derived respiratory rate in general care floor patients. J Clin Monit Comput. 2015;29:113–20.
Garde A, Karlen W, Ansermino JM, Dumont GA. Estimating respiratory and heart rates from the correntropy spectral density of the photoplethysmogram. PLoS ONE. 2014;9:e86427.
Nilsson L, Johansson A, Kalman S. Respiration can be monitored by photoplethysmography with high sensitivity and specificity regardless of anaesthesia and ventilatory mode. Acta Anaesthesiol Scand. 2005;49:1157–62.
Oksala N, Liuhanen S (2015) Method and device for the detection of respiratory rate. PCT/FI2015/050023.
Charlton PH (2016) In: Synthetic dataset: dataset for verification of algorhitm implementions. Charlton Peter H. http://peterhcharlton.github.io/RRest/synthetic_dataset.html. Accessed 10 Aug 2016.
Shrivastava A, Gupta V. Methods for the determination of limit of detection and limit of quantitation of the analytical methods. Chron Young Sci. 2011;2:21–5.
Zou GY. Confidence interval estimation for the Bland–Altman limits of agreement with multiple observations per individual. Stat Methods Med Res. 2013;22:630–42.
Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17:571–82.
Batchelder PB, Raley DM. Maximizing the laboratory setting for testing devices and understanding statistical output in pulse oximetry. Anesth Analg. 2007;105:S85–94.
Finnish Standards association (2011) Medical electrical equipment—Part 2–61: particular requirements for basic safety and essential performance of pulse oximeter equipment (ISO 80601-2-61:2011).
Fischer MO, Fornier W, Hanouz JL, Fellahi JL. Cephalic and digital pulse oximetry in cardiac surgery: a comparative pilot study with arterial oximetry. Eur J Anaesthesiol. 2015;32:60–1.
Salyer JW. Neonatal and pediatric pulse oximetry. Respir Care. 2003;48:386–96 (discussion 397-8).
MacLeod DB, Cortinez LI, Keifer JC, Cameron D, Wright DR, White WD, Moretti EW, Radulescu LR, Somma J. The desaturation response time of finger pulse oximeters during mild hypothermia. Anaesthesia. 2005;60:65–71.
Tendera M, Aboyans V, Bartelink M, Baumgartner I, Clement D, Collet J, Cremonesi A, De Carlo M, Erbel R, Fowkes FG, Heras M, Kownator S, Minar E, Ostergren J, Poldermans D, Riambau V, Roffi M, Röther J, Sievert H, van Sambeek M, Zeller T. ESC Guidelines on the diagnosis and treatment of peripheral artery diseases. Eur Heart J. 2011;32:2851–906.
Hernandez-Silveira M, Ahmed K, Ang SS, Zandari F, Mehta T, Weir R, Burdett A, Toumazou C, Brett SJ. Assessment of the feasibility of an ultra-low power, wireless digital patch for the continuous ambulatory monitoring of vital signs. BMJ Open. 2015;5:e006606.
Nair D, Tan SY, Gan HW, Lim SF, Tan J, Zhu M, Gao H, Chua NH, Peh WL, Mak KH. The use of ambulatory tonometric radial arterial wave capture to measure ambulatory blood pressure: the validation of a novel wrist-bound device in adults. J Hum Hypertens. 2008;22:220–2.
Acknowledgments
The authors wish to thank the Paulo Foundation, Finnish Society of Anaesthesiologists and the Finnish Cultural Foundation, Pirkanmaa Regional Fund for grants, as well as the Medieta Oy (Helsinki, Finland), which provided the study device.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
SL and NO have a pending patent on RR measurement. NO has been a shareholder on a former company Medieta. AV and PK have been former employees on a former company Medieta. JH, VL, and AY-H declare no conflicts of interest.
Ethical approval
This study was approved by the Pirkanmaa Hospital district ethics committee. All procedures involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee, as well as with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Harju, J., Vehkaoja, A., Lindroos, V. et al. Determination of saturation, heart rate, and respiratory rate at forearm using a Nellcor™ forehead SpO2-saturation sensor. J Clin Monit Comput 31, 1019–1026 (2017). https://doi.org/10.1007/s10877-016-9940-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9940-7