Abstract
Fiberoptic bronchoscopy (FOB) via endotracheal tube (ETT) is the most frequent utilized technique for monitoring of percutaneous dilatational tracheostomy (PDT) procedure while maintaining mechanical ventilation. Endoscopic guidance has increased the safety of this procedure; nevertheless, the use of a bronchoscope via ETT potentially may deteriorate ventilation and lead to hypercarbia and/or hypoxia. EtView tracheoscopic ventilation tube (EtView TVT) is a standard endotracheal tube with a camera and light source embedded at the tip. The objectives of this study are to introduce EtView TVT as a monitoring tool during PDT and to compare it with video assisted FOB via ETT. We hypothesized that using EtView TVT during PDT may obtain similar visualization; also may have advantages regarding better mechanical ventilation conditions when compared with video-assisted FOB via ETT. Patients, 18–75 years of age requiring mechanical ventilation scheduled for PDT were randomly allocated into two groups for airway monitorization to guide PDT procedure either with FOB via ETT (Group FOB, n = 12) or EtView TVT (Group EtView, n = 12). After standard anesthesia protocol, alveolar recruitment maneuver was applied and all patients were mechanically ventilated at pressure-controlled ventilation mode with same pressure levels. The primary outcome variable was the reduction in arterial oxygen partial pressure (PaO2) values during the procedure. Other respiratory variables and the effectiveness (the visualization and identification of relevant airway structures) of two techniques were the secondary outcome variables. Patients in both groups were comparable with respect to demographic characteristics and initial respiratory variables. Visualization and identification of relevant airway structures in any steps of the PDT procedure were also comparable. The decrease in minute ventilation in Group FOB was higher when compared with Group EtView (51 ± 4 % vs. 12 ± 7.3 %, p < 0.05). The decrease in PaO2 from initial levels during (34 ± 21 % vs. 5 ± 7 % decrease) and after (26 ± 27 % vs. 2.8 ± 16 % decrease) the procedure was higher in Group FOB when compared with Group EtView (p < 0.05). Considering comparable features in monitorization and advantageous features over mechanical ventilation when compared with video bronchoscopy; EtView TVT would be a good alternative for airway monitorization during PDT especially for patients with poor pulmonary reserve.
Similar content being viewed by others
1 Introduction
In recent clinical practice, percutaneous dilatational tracheostomy (PDT), which has been firstly introduced by Ciaglia et al. [1] in 1985, is one of the most performed interventional airway management procedure in intensive care units. The procedure has been changed and modified several times through years and recently it is considered as safe, easy to perform, time and cost sparing bedside procedure. But, some serious complications may occur during or after the PDT procedure, like tracheal wall damage, marginal punctures (extra midline punctures, punctures above or below first and second tracheal cartilages), injury of neck structures, hemorrhage, para-tracheal placement, endotracheal tube (ETT) cuff rupture and loss of airway by undesirable extubation [2–4]. Most of these complications are related with lack of airway monitoring or poor visualization during PDT process. Fiberoptic bronchoscopy (FOB) via ETT or a laryngeal mask airway (LMA) is still the most frequent utilized technique for monitoring of this procedure while maintaining mechanical ventilation support [5, 6]. Endoscopic guidance has increased the safety of this procedure; nevertheless, the use of a bronchoscope via ETT or LMA potentially may deteriorate ventilation and lead to hypercarbia, hypoxia, and/or alveolar de-recruitment [7, 8].
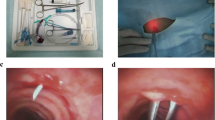
EtView tracheoscopic ventilation tube (EtView TVT™, ETView Ltd, Misgav, Israel) is a standard ETT with a camera embedded at the tip for continuous visualization of intra-tracheal structures and ETT position during mechanical ventilation support (Figs. 1 and 2). It has been employed for monitorization of endotracheal tube positioning and airway structures; airway management during one-lung ventilation, difficult intubation, and tracheal rupture [9–13].
The use of EtView TVT during PDT was not described before. We hypothesized that using EtView TVT during PDT may obtain similar visualization, also may have advantages regarding better mechanical ventilation conditions and improvement in oxygenation and gas exchange when compared with video-assisted FOB via ETT.
2 Materials and methods
The study protocol was approved by the Institutional Ethical Committee of Bezmialem Vakif University. Patients, 18–75 years of age requiring mechanical ventilation scheduled for PDT in our Intensive Care Unit were included in this study. Emergency procedures, patients having difficult intubation criteria and any contraindication to the PDT procedure, patients with low oxygenation score (PaO2/FiO2 < 200) and patients requiring higher positive end-expiratory pressure (PEEP) levels (>10 cm H2O) were excluded. In accordance with the Declaration of Helsinki, the purpose and method of the study were sufficiently explained to the legal representatives of each patient and the study was conducted after obtaining informed written consent. Enteral nutrition of patients was discontinued at least 6 h before PDT procedure. Patients were randomly allocated into two groups by a computer-generated randomization list. Computer-generated randomization was done using 24 opaque sealed envelopes, 12 for each group, indicating group assignment. Before PDT procedure was started, an anesthesiologist opened the next envelope in the sequence to reveal the monitoring technique allocation.
2.1 Anesthesia
All patients received midazolam 0.03–0.05 mg/kg, propofol 1–2 mg/kg, vecuromium 0.1 mg/kg for anesthesia induction. Anesthesia was maintained with propofol 3–10 mg/kg/h and remifentanil 0.05–0.25 mg/kg/min intravenous infusions. In one group (Group EtView), patients were re-intubated with EtView TVT with 7.0–7.5 mm internal diameter, which allows for continuous monitoring of the tracheal lumen. In other group (Group FOB), the procedure was continued with the existing ETT.
Before the PDT procedure, alveolar recruitment maneuver was applied to all patients with 100 % oxygen and CPAP mode consisting a peak pressure 40 cm H2O for 40 s. All patients were mechanically ventilated at pressure-controlled ventilation mode in FiO2: 100 % and with pressure support level 15 cm H2O, PEEP: 10 cm H2O, inspirium time/expirium time: ½. Respiratory rate was adjusted to maintain end-tidal carbon dioxide (EtCO2) 30–40 mmHg before the procedure and kept constant during and after the procedure. Procedure was started 30 min after the recruitment maneuver.
The interspace between the first and the second tracheal cartilages were marked as puncture site and all patients received skin infiltration of 3–5 ml bupivacaine 0.5 % after skin preparation. The PDT was performed according to Griggs method [14] with Portex Griggs-Set (Smiths Medical, Colonial Way, Watford, UK).
In Group EtView, the EtView TVT was withdrawn to the level of first tracheal cartilage while the cuff was deflated and the LED light at the tip was used as a landmark for puncture. In Group FOB, at the beginning of the procedure, a fiberoptic bronchoscope (Karl Storz, Tuttlingen, Germany) with an external diameter equal to 3.7 mm was introduced into the ETT though a catheter-mount, which had a small opening on the cap (in order to maintain mechanical ventilation). The FOB was positioned at the tip of the ETT, the cuff was deflated, and under direct vision, the ETT was withdrawn to the level of the first tracheal cartilage and the light of the bronchoscope was used as a landmark for puncture. The cuff was then inflated to maintain positive pressure mechanical ventilation in both groups.
The same experienced anesthetist-intensivist was performed all PDT procedures. Another experienced anesthetist performed all monitorization, either EtView TVT or FOB. And the third experienced anesthetist evaluated the visualization of the PDT procedure.
The effectiveness (the visualization and identification of relevant airway structures) of EtView TVT or video-assisted FOB via ETT during PDT procedure was evaluated using a standardized 4-step rating scale from 1 to 4 (1: very good; 2: good, mostly visible; 3: poorly visible, mostly unrecognized; 4: any of the anatomic landmarks does not recognized) adopted from Linstedt et al. [6]. The following steps were evaluated:
-
1.
Identification of thyroid, cricoid, and tracheal (first to third) cartilage,
-
2.
Visualization of tracheal circumference,
-
3.
Monitoring of puncture site,
-
4.
Monitoring of anterior wall and pars membranacea during forceps dilatation.
Arterial blood gases analysis was obtained 3 times: just before the procedure was started; just before the tracheostomy cannula was inserted and 15 min after the procedure. Minimal (the lowest) minute volume (MV) values were also recorded before, during (after ETT or EtView TVT was withdrawn and cuff was inflated until tracheal dilatation phase) and after the procedure. Hearth rate, arterial pressures, peripheral oxygen saturation levels were also monitorized during the whole PDT procedure.
The primary outcome variable was the reduction in arterial oxygen partial pressure (PaO2) values during the procedure (just before the tracheostomy cannula was inserted) when compared with initial values. The sample size requirement was based on preliminary data from a previous pilot study with 5 patients in Group FOB in which there is a 31 ± 13 % decrease in PO2 values. Thus, at an alpha risk of 0.05, 12 patients per group would provide 90 % power and detect a 50 % improvement in this decrease in a treatment group. Secondary outcome measures were the effectiveness of video bronchoscopy via ETT or EtView TVT and the changes in MV and arterial carbon dioxide partial pressure (PaCO2) during PDT procedure.
In this study, SPSS Version 15.0 (SPSS, Chicago, IL) was used for statistical analysis. Mann–Whitney U test was used to compare arterial blood gases analysis results and minute ventilation levels between groups. Wilcoxon test was used to compare blood gas analysis and minute ventilation levels inside the groups. The assessment of the effectiveness of PDT with video bronchoscopy via ETT or EtView TVT was compared between groups with the x2 test. P < 0.05 was regarded as statistically significant.
3 Results
Of the 46 patient approached, 19 did not meet the criteria for inclusion, consent could not be received in 3, leaving 24 patients (12 for each group) suitable to be enrolled in this investigation (Fig. 3).
Patients in both groups were comparable with respect to demographic characteristics (Table 1) and to initial respiratory variables (Table 2). Duration of PDT procedure (from time when ETT was withdrawn to tracheostomy cannula was inserted) was 21.6 ± 3 min in Group EtView and 20.8 ± 3 min in Group FOB, also comparable between groups.
There was no statistically significant difference (p > 0.05) between groups with respect to visualization and identification of relevant airway structures in any steps of the PDT procedure using 4-step rating scale, while the median rate was 1 (range: 1–2) in all steps.
Arterial blood gas analysis results are shown in Table 2. The decrease in PaO2 levels during (34 ± 21 % vs. 5 ± 7 %) and after (26 ± 27 % vs. 2.8 ± 16 %) the procedure when compared with initial levels was higher in Group FOB (p < 0.05). Also, the increase in PaCO2 levels during and after the procedure when compared with initial levels was statistically significant.
Minimal MV values are shown in Table 2. There was a statistically significant decrease in MV during the procedure in both groups, but the decrease in Group FOB was higher (12 ± 7.3 % vs. 51 ± 4 %, p < 0.05). There was no procedure-related complication in both groups.
4 Discussion
Monitorization of relevant airway structures and puncture site with EtView TVT for ease and safety of PDT procedure was not described before. In this prospective randomized study, we compared video bronchoscopy and EtView TVT as a monitorization tool during PDT. Both tools had similar effectiveness for monitorization and all two techniques seem to be safe and easy to perform, as there was no complication occurred during procedures. But, there was deterioration in MV during PDT in both groups. In Group FOB, the marked decrease in MV was accompanied with a decrease in PO2 and an increase in PCO2. This decrease in MV before tracheal dilatation phase may be due to an increase in airway resistance or leakage. It can be calculated that a bronchoscope with 3.7 mm diameter causes an approximately 28 % obstruction inside an ETT with 7 mm internal diameter. We think that the marked decrease in MV was due to both increases in airway resistance, leakage around the catheter-mount, ETT cuff and puncture site in Group FOB; while, the relatively lower decrease in MV in Group EtView was mostly due to leakage around the cuff and puncture site. After the procedure, MV was improved in both groups, however PO2, PCO2 levels in Group FOB may indicate an alveolar de-recruitment. In Group FOB the deterioration in ventilation may not be clinically significant, but much worse clinical consequences can be expected in a group of patients with lower pulmonary reserve. Using EtView TVT for PDT could be of interest in high-risk patients, such as those with severe hypoxemia.
Some previous studies reported that FOB via LMA during PDT may improve both visualization and ventilation [5, 6]. Linstedt et al. [6] found the LMA group more advantageous in mechanical ventilation and monitorization over ETT group. Additionally they stated that bronchoscope damage and loss of airway only occurred in ETT group. Furthermore, they found that 3 patients with ETT showed critically impaired ventilation and resulted hypoxia (PaO2 < 60 mmHg) while no patients with LMA suffered significant deterioration of mechanical ventilation support and oxygenation during the procedure. In our study, we didn’t encounter hypoxia in any group that may be due to recruitment maneuver employed before PDT procedure or the relatively smaller size bronchoscope (with 3.7 mm internal diameter) we used. Recruitment maneuver in prevention of hypoxia during PDT was suggested [15]. However, LMA may not be suitable in patients requiring higher airway pressures and PEEP levels.
Recently, single-use EtView TVT may be an expensive tool. However the cost-effectiveness of FOB over EtView TVT is questionable. It is estimated one to two bronchoscopes were damaged per 100 PDT procedures [2, 6], also cost of disinfection should be considered. Routine-use of EtView TVT for airway monitorization in intensive care units in the near future will not be a surprise. Continuous airway monitorization with EtView TVT may inform us for the correct positioning of the tube and secretions in the airway (time for suctioning).
One of the limitations of the study is the lack of blinding. As the monitor devices of FOB and EtView TVT was not similar in shape, blinding of the study was difficult to apply. Another limitation of this study is the fact that all patients randomized in the EtView TVT were reintubated to benefit from the new tracheal tube. However, reintubation is a risk factor for microaspiration and ventilator-associated pneumonia. Also, the number of patients that may not be sufficient for the assessment of visualization quality. A trial in patients undergoing PDT procedure that compares EtView TVT with video-assisted FOB via LMA as a monitoring technique would be considered as a future study.
In conclusion: EtView TVT had comparable effectiveness in airway monitorization and caused less deterioration in minute ventilation during PDT when compared with video assisted FOB via ETT. EtView TVT guidance during PDT may be a good alternative to FOB in patients with poor pulmonary reserve.
References
Ciaglia P, Firsching R, Syniec C. Elective percutaneous dilatational tracheostomy. A new simple bedside procedure; preliminary report. Chest. 1985;87(6):715–9.
Treu TM, Knoch M, Focke N, Schulz M. Percutaneous dilatative tracheostomy as a new method in intensive medicine. Procedure, advantages and risks. Dtsch Med Wochenschr. 1997;122(19):599–605.
Heuer B, Deller A. Early and long-term results of percutaneous dilatation tracheostomy (PDT Ciaglia) in 195 intensive care patients. Anasthesiol Intensivmed Notfallmed Schmerzther. 1998;33(5):306–12.
Polderman KH, Spijkstra JJ, de Bree R, Christiaans HM, Gelissen HP, Wester JP, Girbes AR. Percutaneous dilatational tracheostomy in the ICU: optimal organization, low complication rates, and description of a new complication. Chest. 2003;123(5):1595–602.
Dosemeci L, Yilmaz M, Gürpinar F, Ramazanoglu A. The use of the laryngeal mask airway as an alternative to the endotracheal tube during percutaneous dilatational tracheostomy. Intensive Care Med. 2002;28(1):63–7.
Linstedt U, Zenz M, Krull K, Häger D, Prengel AW. Laryngeal mask airway or endotracheal tube for percutaneous dilatational tracheostomy: a comparison of visibility of intratracheal structures. Anesth Analg. 2010;110:1076–82.
Reilly PM, Anderson HL 3rd, Sing RF, Schwab CW, Bartlett RH. Occult hypercarbia. An unrecognized phenomenon during percutaneous endoscopic tracheostomy. Chest. 1995;107:1760–3.
Durbin CG Jr. Early complications of tracheostomy. Respir Care. 2005;50:511–5.
Giglio M, Oreste D, Oreste N. Usefullness of ETView TVT endotracheal tube for correct positioning of the bronchial blockers in left lobectomy; an easy and safe combination. Minerva Anestesiol. 2009;75(suppl.1 to No.7–8):1–4.
Barak M, Putilov V, Meretyk S, Halachmi S. ETView tracheoscopic ventilation tube for surveillance after tube position in patients undergoing percutaneous nephrolithotomy. Br J Anaesth. 2010;104:501–4.
Heitz JW, Shum PP, Grunwald Z. Use of a tracheoscopic ventilation tube for endotracheal intubation in the difficult airway. J Clin Anesth. 2011;23:403–6.
Umutoglu T, Bakan M, Topuz U, Alver S, Ozturk E. Use of ETView Tracheoscopic Ventilation Tube® in airway management of a patient with tracheal injury. Minerva Anestesiol. 2014;80:398–9.
Topuz U, Bakan M, Umutoglu T, Karaaslan K. Use of ETView™ tracheoscopic ventilation tube for unilateral pulmonary ventilation. Turk Gogus Kalp Dama. 2014;22(2):461–3.
Griggs WM, Worthley LIG, Gilligan JE, Thomas PD, Myburg JA. A simple percutaneous tracheostomy technique. Surg Gynecol Obstet. 1990;170:543–5.
Franchi F, Cubattoli L, Faltoni A, Scolletta S, Falciani E, Mastrocinque E, et al. Recruitment maneuver in prevention of hypoxia during percutaneous dilational tracheostomy: randomized trial. Respir Care. 2012;57:1850–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Umutoglu, T., Bakan, M., Topuz, U. et al. Comparison of EtView™ tracheoscopic ventilation tube and video-assisted fiberoptic bronchoscopy during percutaneous dilatational tracheostomy. J Clin Monit Comput 31, 507–512 (2017). https://doi.org/10.1007/s10877-016-9885-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9885-x