Abstract
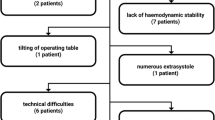
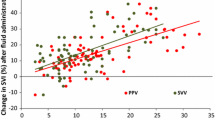
The aim of this prospective study was to evaluate the usefulness of stroke volume variation (SVV) derived from NICOM® to predict fluid responsiveness in the prone position. Forty adult patients undergoing spinal surgery in the prone position were included in this study. We measured SVV from NICOM® (SVVNICOM) and FloTrac™/Vigileo™ systems (SVVVigileo), and pulse pressure variation (PPV) using automatic (PPVauto) and manual (PPVmanual) calculations at four time points including supine and prone positions, and before and after fluid loading of 6 ml kg−1 colloid solution. Fluid responsiveness was defined as an increase in the cardiac index from Vigileo™ of ≥12 %. There were 19 responders and 21 non-responders. Prone positioning induced a significant decrease in SVVNICOM, SVVVigileo, PPVauto, and PPVmanual. However, all of these parameters successfully predicted fluid responsiveness in the prone position with area under the receiver-operator characteristic curves for SVVNICOM, SVVVigileo, PPVauto, and PPVmanual of 0.78 [95 % confidence interval (CI) 0.62–0.90, P = 0.0001], 0.79 (95 % CI 0.63–0.90, P = 0.0001), 0.76 (95 % CI 0.6–0.88, P = 0.0006), and 0.84 (95 % CI 0.69–0.94, P < 0.0001), respectively. The optimal cut-off values were 12 % for SVVNICOM, SVVVigileo, and PPVauto, and 10 % for PPVmanual. SVV from NICOM® successfully predicts fluid responsiveness during surgery in the prone position. This totally non-invasive technique for assessing individual functional intravenous volume status would be useful in a wide range of surgeries performed in the prone position.



Similar content being viewed by others
References
Benes J, Chytra I, Altmann P, Hluchy M, Kasal E, Svitak R, Pradl R, Stepan M. Intraoperative fluid optimization using stroke volume variation in high risk surgical patients: results of prospective randomized study. Crit Care. 2010;14:R118. doi:10.1186/cc9070.
Perel A, Habicher M, Sander M. Bench-to-bedside review: functional hemodynamics during surgery—should it be used for all high-risk cases? Crit Care. 2013;17:203. doi:10.1186/cc11448.
Navarro LH, Bloomstone JA, Auler JO Jr, Cannesson M, Rocca GD, Gan TJ, Kinsky M, Magder S, Miller TE, Mythen M, Perel A, Reuter DA, Pinsky MR, Kramer GC. Perioperative fluid therapy: a statement from the international Fluid Optimization Group. Perioper Med (Lond). 2015;4:3. doi:10.1186/s13741-015-0014-z.
Sudheer PS, Logan SW, Ateleanu B, Hall JE. Haemodynamic effects of the prone position: a comparison of propofol total intravenous and inhalation anaesthesia. Anaesthesia. 2006;61:138–41. doi:10.1111/j.1365-2044.2005.04464.x.
Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. Br J Anaesth. 2008;100:165–83. doi:10.1093/bja/aem380.
Biais M, Bernard O, Ha JC, Degryse C, Sztark F. Abilities of pulse pressure variations and stroke volume variations to predict fluid responsiveness in prone position during scoliosis surgery. Br J Anaesth. 2010;104:407–13. doi:10.1093/bja/aeq031.
Yang SY, Shim JK, Song Y, Seo SJ, Kwak YL. Validation of pulse pressure variation and corrected flow time as predictors of fluid responsiveness in patients in the prone position. Br J Anaesth. 2013;110:713–20. doi:10.1093/bja/aes475.
Marque S, Cariou A, Chiche JD, Squara P. Comparison between Flotrac–Vigileo and bioreactance, a totally noninvasive method for cardiac output monitoring. Crit Care. 2009;13:R73. doi:10.1186/Cc7884.
Squara P, Rotcajg D, Denjean D, Estagnasie P, Brusset A. Comparison of monitoring performance of Bioreactance vs. pulse contour during lung recruitment maneuvers. Crit Care. 2009;13:R125. doi:10.1186/cc7981.
Vergnaud E, Vidal C, Verchere J, Miatello J, Meyer P, Carli P, Orliaguet G. Stroke volume variation and indexed stroke volume measured using bioreactance predict fluid responsiveness in postoperative children. Br J Anaesth. 2015;114:103–9. doi:10.1093/bja/aeu361.
Benomar B, Ouattara A, Estagnasie P, Brusset A, Squara P. Fluid responsiveness predicted by noninvasive bioreactance-based passive leg raise test. Intensive Care Med. 2010;36:1875–81. doi:10.1007/s00134-010-1990-6.
Marik PE, Levitov A, Young A, Andrews L. The use of bioreactance and carotid Doppler to determine volume responsiveness and blood flow redistribution following passive leg raising in hemodynamically unstable patients. Chest. 2013;143:364–70. doi:10.1378/chest.12-1274.
Pai MP, Paloucek FP. The origin of the “ideal” body weight equations. Ann Pharmacother. 2000;34:1066–9.
Aboy M, McNames J, Thong T, Phillips CR, Ellenby MS, Goldstein B. A novel algorithm to estimate the pulse pressure variation index deltaPP. IEEE Trans Biomed Eng. 2004;51:2198–203. doi:10.1109/TBME.2004.834295.
Cannesson M, Slieker J, Desebbe O, Bauer C, Chiari P, Henaine R, Lehot JJ. The ability of a novel algorithm for automatic estimation of the respiratory variations in arterial pulse pressure to monitor fluid responsiveness in the operating room. Anesth Analg. 2008;106:1195–200. doi:10.1213/01.ane.0000297291.01615.5c.
Raval NY, Squara P, Cleman M, Yalamanchili K, Winklmaier M, Burkhoff D. Multicenter evaluation of noninvasive cardiac output measurement by bioreactance technique. J Clin Monit Comput. 2008;22:113–9. doi:10.1007/s10877-008-9112-5.
Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Casp J Intern Med. 2013;4:627–35.
Frezza EE, Mezghebe H. Indications and complications of arterial catheter use in surgical or medical intensive care units: analysis of 4932 patients. Am Surg. 1998;64:127–31.
Mermel LA. Prevention of intravascular catheter-related infections. Ann Intern Med. 2000;132:391–402.
Marque S, Cariou A, Chiche JD, Squara P. Comparison between Flotrac–Vigileo and bioreactance, a totally noninvasive method for cardiac output monitoring. Crit Care. 2009;13:R73. doi:10.1186/cc7884.
Khan FZ, Virdee MS, Pugh PJ, Read PA, Fynn SP, Dutka DP. Non-invasive cardiac output measurements based on bioreactance for optimization of atrio- and interventricular delays. Europace. 2009;11:1666–74. doi:10.1093/europace/eup358.
Lee JY, Kim JY, Choi CH, Kim HS, Lee KC, Kwak HJ. The ability of stroke volume variation measured by a noninvasive cardiac output monitor to predict fluid responsiveness in mechanically ventilated children. Pediatr Cardiol. 2014;35:289–94. doi:10.1007/s00246-013-0772-7.
Grocott MP, Mythen MG, Gan TJ. Perioperative fluid management and clinical outcomes in adults. Anesth Analg. 2005;100:1093–106. doi:10.1213/01.ANE.0000148691.33690.AC.
Hojlund J, Sandmand M, Sonne M, Mantoni T, Jorgensen HL, Belhage B, van Lieshout JJ, Pott FC. Effect of head rotation on cerebral blood velocity in the prone position. Anesthesiol Res Pract. 2012;2012:647258. doi:10.1155/2012/647258.
Cannesson M, Le Manach Y, Hofer CK, Goarin JP, Lehot JJ, Vallet B, Tavernier B. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a “gray zone” approach. Anesthesiology. 2011;115:231–41. doi:10.1097/ALN.0b013e318225b80a.
Michard F, Chemla D, Teboul JL. Applicability of pulse pressure variation: how many shades of grey? Crit Care. 2015;19:144. doi:10.1186/s13054-015-0869-x.
Monnet X, Dres M, Ferre A, Le Teuff G, Jozwiak M, Bleibtreu A, Le Deley MC, Chemla D, Richard C, Teboul JL. Prediction of fluid responsiveness by a continuous non-invasive assessment of arterial pressure in critically ill patients: comparison with four other dynamic indices. Br J Anaesth. 2012;109:330–8. doi:10.1093/bja/aes182.
Biais M, Stecken L, Ottolenghi L, Roullet S, Quinart A, Masson F, Sztark F. The ability of pulse pressure variations obtained with CNAP device to predict fluid responsiveness in the operating room. Anesth Analg. 2011;113:523–8. doi:10.1213/ANE.0b013e3182240054.
Ameloot K, Palmers PJ, Malbrain ML. The accuracy of noninvasive cardiac output and pressure measurements with finger cuff: a concise review. Curr Opin Crit Care. 2015;21:232–9. doi:10.1097/MCC.0000000000000198.
Yin JY, Ho KM. Use of plethysmographic variability index derived from the Massimo® pulse oximeter to predict fluid or preload responsiveness: a systematic review and meta-analysis. Anaesthesia. 2012;67:777–83. doi:10.1111/j.1365-2044.2012.07117.x.
Mehta Y, Chand RK, Sawhney R, Bhise M, Singh A, Trehan N. Cardiac output monitoring: comparison of a new arterial pressure waveform analysis to the bolus thermodilution technique in patients undergoing off-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth. 2008;22:394–9. doi:10.1053/j.jvca.2008.02.015.
Hong DM, Lee JM, Seo JH, Min JJ, Jeon Y, Bahk JH. Pulse pressure variation to predict fluid responsiveness in spontaneously breathing patients: tidal vs. forced inspiratory breathing. Anaesthesia. 2014;69:717–22. doi:10.1111/anae.12678.
Monnet X, Pinsky M, Teboul J-L. FTc is not an accurate predictor of fluid responsiveness. Intensive Care Med. 2006;32:1090–1. doi:10.1007/s00134-006-0158-x.
Schonauer C, Bocchetti A, Barbagallo G, Albanese V, Moraci A. Positioning on surgical table. Eur Spine J. 2004;13(Suppl 1):S50–5. doi:10.1007/s00586-004-0728-y.
Huang L, Critchley LA, Zhang J. Major upper abdominal surgery alters the calibration of bioreactance cardiac output readings, the NICOM, when comparisons are made against suprasternal and esophageal Doppler intraoperatively. Anesth Analg. 2015;121:936–45. doi:10.1213/ANE.0000000000000889.
Kupersztych-Hagege E, Teboul JL, Artigas A, Talbot A, Sabatier C, Richard C, Monnet X. Bioreactance is not reliable for estimating cardiac output and the effects of passive leg raising in critically ill patients. Br J Anaesth. 2013;111:961–6. doi:10.1093/bja/aet282.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Jong-Hwan Lee and Soo Joo Choi have contributed equally as co-corresponding authors.
Rights and permissions
About this article
Cite this article
Min, J.J., Lee, JH., Hong, K.Y. et al. Utility of stroke volume variation measured using non-invasive bioreactance as a predictor of fluid responsiveness in the prone position. J Clin Monit Comput 31, 397–405 (2017). https://doi.org/10.1007/s10877-016-9859-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9859-z