Abstract
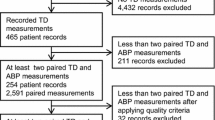
We know that a 10 cm departure from the reference level of pressure transducer position is equal to a 7.5 mmHg change of invasive hemodynamic pressure monitoring in a fluid-filled system. However, the relationship between the site level of a variable arterial pressure transducer and the pulse contour-derived parameters has yet to be established in critically ill patients. Moreover, the related quantitative analysis has never been investigated. Forty-two critically ill patients requiring PiCCO-Plus cardiac output monitoring were prospectively studied. The phlebostatic axis was defined as the zero reference level; the arterial pressure transducer was then vertically adjusted to different positions (+5, +10, +15, +20, −20, −15, −10, −5 cm) of departure from the zero reference site. The pulse contour waveform-derived parameters were recorded at each position. Elevation of the pressure transducer caused significantly positive changes in the continuous cardiac index (+CCI), stroke volume index (+SVI), and stroke volume variation (+SVV), and negative changes in the rate of left ventricular pressure rise during systole (−dP/dtmax), the systemic vascular resistance index (−SVRI), and vice versa. At the 5 cm position, the SVRI changes reached statistical significance with error. At the 10 cm position, the changes in CCI and dP/dtmax reached statistical significance with error, while the change in SVV reached statistical significance at 15 cm. The change rate of CCI was more than 5 % at the 15 cm position and approximately 10 % at the 20 cm position. On average, for every centimeter change of the transducer, there was a corresponding 0.014 L/min/m2 CCI change and 0.36 % change rate, a 1.41 mmHg/s dP/dtmax change and 0.13 % change rate, and a 25 dyne/s/cm5 SVRI change and 1.2 % change rate. The variation of arterial transducer position can result in inaccurate measurement of pulse contour waveform-derived parameters, especially when the transducer’s vertical distance is more than 10 cm from the phlebostatic axis. These findings have clinical implications for continuous hemodynamic monitoring.


Similar content being viewed by others
References
Rauen CA, Makic MBF, Bridges E. Practice evidence-based practice habits: transforming research into bedside. Crit Care Nurse. 2009;29:46–59.
Winsor T, Burch G. Phlebostatic level: reference level for venous pressure measurement in man. Proc Soc Exp Biol Med. 1945;58:165–9.
McCann UG II, Schiller HJ, Carney DE, Kilpatrick J, Gatto LA, Paskanik AM, Nieman GF. Invasive arterial BP monitoring in trauma and critical care. Chest. 2001;120:1322–6.
Tagami T, Kushimoto S, Tosa R, et al. The precision of PiCCO® measurements in hypothermic post-cardiac arrest patients. Anaesthesia. 2012;67:236–43.
de Wilde RB, Schreuder JJ, van den Berg PC, Jansen JR. An evaluation of cardiac output by five arterial pulse contour techniques during cardiac surgery. Anaesthesia. 2007;62:760–8.
Perner A, Haase N, Wiis J, White JO, Delaney A. Central venous oxygen saturation for the diagnosis of low cardiac output in septic shock patients. Acta Anaesthesiol Scand. 2010;54:98–102.
Scolletta Sabino, Bodson Laurent, Donadello Katia, Taccone Fabio S, Devigili Alessandro, Vincent Jean-Louis, De Backer Daniel. Assessment of left ventricular function by pulse wave analysis in critically ill patients. Intensive Care Med. 2013;39:1025–33.
He H, Liu D, Long Y, Wang X, Yuan Y, Li X, Guo H, Cai J, Fang N. The relationship between arterial transducer level and pulse contour waveform-derived measurements. Crit Care. 2015;19:31.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–8295.
Kleinman B, Powell S, Kumar P, Gardner RM. The fast flush test measures the dynamic response of the entire blood pressure monitoring system. Anesthesiology. 1992;77:1215–20.
Watanabe H, Yagi S, Namiki A. Recommendation of a clinical impulse response analysis for catheter calibration-dumping coefficient and natural frequency are incomplete parameters for clinical evaluation. J Clin Monit Comput. 2006;20:37–42.
Roy A. Estimating correlation coefficient between two variables with repeated observations using mixed effects model. Biom J. 2006;48:286–301.
McCulloch CE, Searle SR. Generalized, linear, and mixed models. London: Wiley; 2000.
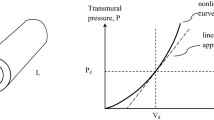
Wesseling KH, de Wit B, Weber JAP, Smith NT. A simple device for the continuous measurement of cardiac output. Adv Cardiovasc Phys. 1983;5:16–52.
Wesseling KH, Jansen JRC, Settels JJ, Schreuder JJ. Computation of aortic flow from pressure in humans using a nonlinear three-element model. J Appl Physiol. 1984;74(5):2566–73.
Wesseling, KH, Smith, NT, Nichols, WW et al. Beat to beat cardiac output from the arterial pressure pulse contour. In: Boerhave, SJ, Course on measurement in anaesthesia. Leiden: University of Leiden Press; 1974. pp. 150–64.
Godje O, Hoke K, Goetz AE, Felbinger TW, Reuter DA, Reichart B, Friedl R, Hannekum A, Pfeiffer UJ. Reliability of a new algorithm for continuous cardiac output determination by pulse-contour analysis during hemodynamic instability. Crit Care Med. 2002;30:52–8.
Monnet X, Anguel N, Naudin B, Jabot J, Richard C, Teboul JL. Arterial pressure-based cardiac output in septic patients: different accuracy of pulse contour and uncalibrated pressure waveform devices. Crit Care. 2010;14(3):R109.
Parry T, Hirsch N, Fauvel N. Comparison of direct blood pressure measurement at the radial and dorsalis pedis arteries during surgery in the horizontal and reverse Trendelenburg positions. Anaesthesia. 1995;50:553–5.
Chulay M, Holland S. Where should the transducer be leveled for radial or femoral arterial pressure monitoring? Crit Care Nurs. 1996;16:103–7.
Ahrens TS, Taylor LA. Technical considerations in obtaining hemodynamic waveform values. In: Darovic GO, editor. Hemodynamic waveform analysis. Philadelphia: W.B. Saunders press; 1992. p. 222.
Courtois M, Fattal PG, Kovacs SJ, et al. Anatomically and physiologically based reference level for measurement of intracardiac pressures. Circulation. 1995;92:1994–2000.
Whitman G, Howaniak D, Verga T. Comparison of cardiac output measurements in 20-degree supine and 20-degree right and left lateral recumbent positions. Heart Lung. 1982;11:256–7.
Dobbin K, Wallace S, Ahlberg J, Chulay M. Pulmonary artery pressure measurement in patients with elevated pressures: effect of backrest elevation and method of measurement. Am J Crit Care. 1992;1:61–9.
Wilson AE, Bermingham-Mitchell K, Wells N, Zachary K. Effect of backrest position on hemodynamic and right ventricular measurements in critically ill adults. Am J Crit Care. 1996;5:264–70.
Giuliano KK, Scott SS, Brown V, Olson M. Backrest angle and cardiac output measurement in critically ill patients. Nurs Res. 2003;52:242–8.
Grose BL, Woods SL, Laurent DJ. Effect of backrest position on cardiac output measured by the thermodilution method in acutely ill patients. Heart Lung. 1981;10:661–5.
Monnet X, Bataille A, Magalhaes E, Barrois J, Le Corre M, Gosset C, Guerin L, Richard C, Teboul JL. End-tidal carbon dioxide is better than arterial pressure for predicting volume responsiveness by the passive leg raising test. Intensive Care Med. 2013;39:93–100.
Jabot J, Teboul JL, Richard C, Monnet X. Passive leg raising for predicting fluid responsiveness: importance of the postural change. Intensive Care Med. 2009;35:85–90.
He HW, Liu DW. Passive leg raising: influence of blood pressure transducer site. Intensive Care Med. 2013;39(9):1668.
Acknowledgments
This work was supported by the special fund for health-scientific research in the public interest program (Grant Number 201202011, the Ministry of Health of P. R. China). The authors thank for Jing Zhang for her contribution in the review of the manuscript of spelling and grammar. There are no financial disclosure for any of the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Figure 1
Corresponding transducer positions and estimated marginal means of CCI change, CCI change rate. CCI continuous cardiac index (L/min/m2) (TIFF 101 kb)
Supplemental Figure 2
Corresponding transducer positions and estimated marginal means of dP/dtmax change, dP/dtmax change rate. dP/dtmax the rate of left ventricular pressure rise during systole(mmHg/s) (TIFF 105 kb)
Supplemental Figure 3
Corresponding transducer positions and estimated marginal means of SVRI change and SVRI change rate. SVRI systemic vascular resistance index (dyne/sec/cm5) (TIFF 102 kb)
Rights and permissions
About this article
Cite this article
He, Hw., Liu, Dw., Long, Y. et al. The effect of variable arterial transducer level on the accuracy of pulse contour waveform-derived measurements in critically ill patients. J Clin Monit Comput 30, 569–575 (2016). https://doi.org/10.1007/s10877-015-9756-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9756-x