Abstract
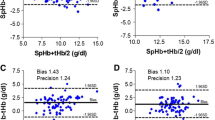
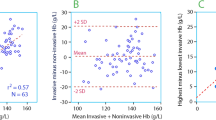
In pediatric fluid therapy it would be preferable to describe distribution and elimination a fluid bolus based on repetitive hemoglobin (Hb) according to kinetic principles. Pulse CO-Oximetry is a recent advancement in patient monitoring that allows for the continuous noninvasive measurement of Hb (SpHb). The aim of this study was to describe the distribution and elimination of hydroxyethylstarch (HES) 130/0.4 in combination with crystalloids using a noninvasive Hb monitor in two cohorts of young children undergoing minor surgeries under general anesthesia. Two cohorts, 16 children aged 1–3 years and 12 aged 4–6 years, were investigated during anesthesia and minor surgical procedures. They were given a maintenance solution of lactated Ringer’s and a fluid bolus of HES 130/0.4, 6 mL/kg over a period of 20 min. The whole procedure lasted 120 min, and SpHb values were measured every 10 min. The SpHb values were used to calculate plasma dilution, net volume, and mean residence time (MRT) of the infused fluid. A total of 377 measured SpHbs generated individual dilution plots that showed variability, particularly for the older cohort. Distribution and elimination rates of the infused fluid were calculated. Mean dilution plots were generated. There were no significant differences in dilution, net volume or MRT between groups. A non invasive Hb analyzer could be used to calculate fluid distribution. The variability in the data can probably be explained by reactions to anesthetic drugs, variability in measurement technique, variability in generating the complex capillary signals, and individual variability in baseline fluid status. The latter finding is important because this is a prerequisite for perioperative fluid planning for each individual.



Similar content being viewed by others
References
Schwarz U. Intraoperative fluid therapy in infants and young children. Anaesthesist. 1999;48(1):41–50.
Standl T, Lochbuehler H, Galli C, Reich A, Dietrich G, Hagemann H. HES 130/0.4 (Voluven) or human albumin in children younger than 2 yr undergoing non-cardiac surgery. A prospective, randomized, open label, multicentre trial. Eur J Anaesthesiol. 2008;25(6):437–45.
Hahn RG. Volume kinetics for infusion fluids. Anesthesiology. 2009;113:470–81.
Shamir MY, Avramovich A, Smaka T. The current status of continuous noninvasive measurement of total, carboxy, and methemoglobin concentration. Anesthesia Analgesia. 2012;114(5):972–8.
Frasca D, Dahyot-Fizelier C, Catherine K, Levrat Q, Debaene B, Mimoz O. Accuracy of a continuous noninvasive hemoglobin monitor in intensive care unit patients. Crit Care Med. 2011;39(10):2277–82.
Hahn RG, Li Y, Zdolsek J. Non-invasive monitoring of blood haemoglobin for analysis of fluid volume kinetics. Acta Anaesthesiol Scand. 2010;54(10):1233–40.
Park YH, Lee JH, Song HG, Byon HJ, Kim HS, Kim JT. The accuracy of noninvasive hemoglobin monitoring using the radical-7 pulse CO-oximeter in children undergoing neurosurgery. Anesth Analg. 2012;115(6):1302–7.
Bergek C, Zdolsek JH, Hahn RG. Accuracy of noninvasive haemoglobin measurement by pulse oximetry depends on the type of infusion fluid. Eur J Anaesthesiol. 2012;29(12):586–92.
Nguyen BV, Vincent JL, Nowak E, Coat M, Paleiron N, Gouny P, et al. The accuracy of noninvasive hemoglobin measurement by multiwavelength pulse oximetry after cardiac surgery. Anesth Analg. 2011;113(5):1052–7.
Svensen C, Olsson J, Rodhe P, Boersheim E, Aarsland A, Hahn RG. Arteriovenous differences in plasma dilution and the kinetics of lactated ringer′s solution. Anesth Analg. 2009;108:128–33.
Karol MD. Mean residence time and the meaning of AUMC/AUC. Biopharm Drug Dispos. 1990;11(2):179–81.
Skelton VA, Wijayasinghe N, Sharafudeen S, Sange A, Parry NS, Junghans C. Evaluation of point-of-care haemoglobin measuring devices: a comparison of Radical-7 pulse Co-Oximetry, HemoCue(®) and laboratory haemoglobin measurements in obstetric patients. Anaesthesia. 2013;68(1):40–5.
Miller RD, Ward TA, Shiboski SC, Cohen NH. A comparison of three methods of hemoglobin monitoring in patients undergoing spine surgery. Anesth Analg. 2011;112(4):858–63.
Macknet MR, Allard M, Applegate RL 2nd, Rook J. The accuracy of noninvasive and continuous total hemoglobin measurement by pulse CO-Oximetry in human subjects undergoing hemodilution. Anesth Analg. 2010;111:1424–6.
Morey TE, Gravenstein N, Rice MJ. Let’s think clinically instead of mathematically about device accuracy. Anesth Analg. 2011;113(1):89–91.
Sjöstrand F, Rodhe P, Berglund E, Lundström N, Svensen C. The use of a noninvasive hemoglobin monitor for volume kinetic analysis in an emergency room setting. Anesth Analg. 2013;116(2):337–42.
Paul M, Dueck M, Joachim Herrmann H, Holzki J. A randomized, controlled study of fluid management in infants and toddlers during surgery: hydroxyethyl starch 6% (HES 70/0.5) versus lactated Ringer’s solution. Paediatr Anaesth. 2003;13(7):603–8.
Chong Sung K, Kum Suk P, Mi Ja Y, Kyoung Ok K. Effects of intravascular volume therapy using hydroxyethyl starch (130/0.4) on post-operative bleeding and transfusion requirements in children undergoing cardiac surgery: a randomized clinical trial. Acta Anaesthesiol Scand. 2006;50(1):108–11.
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Åneman A, et al. Hydroxyethyl starch 130/0.4 versus ringer’s acetate in severe sepsis. N Eng J Med. 2012;367:124–34.
Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367:1901–11.
Akkucuk FG, Kanbak M, Ayhan B, Celebioglu B, Aypar U, et al. The effect of HES (130/0.4) usage as the priming solution on renal function in children undergoing cardiac surgery. Renal Fail. 2013;35(2):210–5
Acknowledgments
Authors recieved Funding from Department of Health, Zhejiang Province, WKJ2010-2-017 to Qingquan Lian and 2012RCA044 to Ruifeng Zeng; Department of Science and Technology, Zhejiang Province, 2011C33042 to Wangning Shangguan; Fund for Natural Science, Zhejiang Province, Y2110380 to Huacheng Liu. This manuscript was screened for plagiarism using http://www.dustball.com/cs/plagiarism.checker.
Ethical standard
An ethical permit (#2011–10) was issued by the Second Hospital & Yuying Children’s Hospital of Wenzhou Medical College Research Ethics Committee. This study was conducted with written informed consent from the parents of the study subjects. The experiments performed in this study comply with the laws of the People′s Republic of China.
Conflict of interest
Christer Svensen consulted for Masimo Inc. and received research funding from Masimo Inc. He served in 2009 as an adviser at a scientific meeting for Masimo in Milan, Italy, during the ESA for which he received an honorarium.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lian, Q., Li, H., Zeng, R. et al. The use of a noninvasive hemoglobin monitor for determining fluid distribution and elimination in pediatric patients undergoing minor surgery. J Clin Monit Comput 29, 41–46 (2015). https://doi.org/10.1007/s10877-014-9566-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9566-6