Abstract
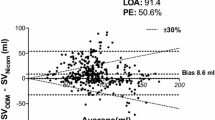
Supra-sternal Doppler (USCOM Ltd., Sydney, Australia) can be used during anaesthesia to measure cardiac output (CO) and related flow parameters. However, before the USCOM can be used routinely, its utility and limitations need to be fully understood and critical information about its use disseminated. In “Window to the Circulation” we use the example of an elderly man undergoing major urological robotic surgery to highlight the utility and limitations of intra-operative USCOM use. USCOM readings were verified against oesophageal Doppler. Despite the lack of major blood loss (<500 ml in 8-h), significant changes in haemodynamics were recorded. CO ranged from 3.2 to 8.3 l/min. The quality of USCOM scans and reliability of data was initially poor, but improved as CO increased as surgery progressed. When USCOM scans became acceptable the correlation with oesophageal Doppler was R2 = 8.0 (p < 0.001). Several characteristic features of the supra-sternal Doppler scans were identified: Aortic and pulmonary flow waves, valve closure, E and A waves, false A-wave and aberrant arterial flow patterns. Their identification helped with identifying the main flow signal across the aortic valve. The USCOM has the potential to monitor changes in CO and related flow parameters intra-operatively and thus help the anaesthetist to more fully understand the patient’s haemodynamics. However, achieving a good quality scan is important as it improves the reliability of USCOM data. The supra-sternal route is rich in flow signals and identifying the aortic valve signal is paramount. Recognizing the other characteristic waveforms in the signal helps greatly.








Similar content being viewed by others
References
Koo KK, Sun JC, Zhou Q, Guyatt G, Cook DJ, Walter SD, Meade MO. Pulmonary artery catheters: evolving rates and reasons for use. Crit Care Med. 2011;39:1613–8.
Marik PE. Noninvasive cardiac output monitors: a state-of the-art review. J Cardiothorac Vasc Anesth. 2013;27:121–34.
Chong SW, Peyton PJ. A meta-analysis of the accuracy and precision of the ultrasonic cardiac output monitor (USCOM). Anaesthesia. 2012;67:1266–71.
Hamilton MA, Cecconi M, Rhodes A. A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth Analg. 2011;112:1392–402.
Critchley LA, Peng ZY, Fok BS, Lee A, Phillips RA. Testing the reliability of a new ultrasonic cardiac output monitor, the USCOM, by using aortic flowprobes in anesthetized dogs. Anesth Analg. 2005;100:748–53.
USCOM. USCOM users manual. Sydney: USCOM Ltd.; 2012.
Dey I, Sprivulis P. Emergency physicians can reliably assess emergency department patient cardiac output using the USCOM continuous wave Doppler cardiac output monitor. Emerg Med Australas. 2005;17:193–9.
Bazett HC. An analysis of the time-relations of electrocardiograms. Heart. 1920;7:353–70.
Smith BE, Madigan VM. Non-invasive method for rapid bedside estimation of inotropy: theory and preliminary clinical validation. Br J Anaesth. (Epub) Aug 1, 2013.
He SR, Sun X, Zhang C, Jian Z, Sun YX, Zheng ML, Liu YM, Madigan VM, Smith BE. Measurement of systemic oxygen delivery and inotropy in healthy term neonates with the ultrasonic cardiac output monitor (USCOM). Early Hum Dev. 2013;89:289–94.
Nidorf SM, Picard MH, Triulzi MO, Thomas JD, Newell J, King ME, Weyman AE. New perspectives in the assessment of cardiac chamber dimensions during development and adulthood. J Am Coll Cardiol. 1992;19:983–8.
Cholley BP, Singer M. Esophageal Doppler: noninvasive cardiac output monitor. Echocardiography. 2003;20:763–9.
Critchley LA. Differences between Cardio-Q and USCOM Doppler cardiac output readings in high risk surgery patients. Br J Anaesth. 2012;108(Suppl 2):113–114 (Abstract).
Huang L, Critchley LA. Comparison of USCOM and CardioQ Doppler cardiac output in high risk surgery. Anaesth Intens Care. 2013;41:(Abstract)(in press).
Derrick J. Monitor software Version 1.1.1b for MacIntosh. http://www.anaesthesia.med.usyd.edu.au/resources/datalogging/monitor.html (2013). Accessed 17 May 2013.
Wolf JS Jr, Monk TG, McDougall EM, McClennan BL, Clayman RV. The extraperitoneal approach and subcutaneous emphysema are associated with greater absorption of carbon dioxide during laparoscopic renal surgery. J Urol. 1995;154:959–63.
Critchley LA, Ho AM. Surgical emphysema as a cause of severe hypercapnia during laparoscopic surgery. Anaesth Intensive Care. 2010;38:1094–100.
Cattermole GNLP, Tang CO, Smith BE, Graham CA, Rainer TH. A new method to score the quality of USCOM scans. Hong Kong J Emerg Med. 2009;16:288.
Critchley LA, Lee A, Ho AM. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111:1180–92.
Perrino AC Jr, Fleming J, LaMantia KR. Transesophageal Doppler cardiac output monitoring: performance during aortic reconstructive surgery. Anesth Analg. 1991;73:705–10.
Phillips RA, Hood SG, Jacobson BM, West MJ, Wan L, May CN. Pulmonary artery catheter (PAC) accuracy and efficacy compared with flow probe and transcutaneous Doppler (USCOM): an ovine cardiac output validation. Crit Care Res Pract. 2012;ID:621496.
Huang L, Critchley LA. A study to determine the reliability of supra-sternal Doppler (USCOM) during general anaesthesia: effects of scan quality, flow volume and increasing age. Br J Anaesth. (Epub) Jul 23, 2013.
Gainsburg DM. Anesthetic concerns for robotic-assisted laparoscopic radical prostatectomy. Minerva Anestesiol. 2012;78:596–604.
Singer M. Oesophageal Doppler. Curr Opin Crit Care. 2009;15:244–8.
Lee SW, Khaw KS, Ngan Kee WD, Leung TY, Critchley LA. Haemodynamic effects from aortocaval compression at different angles of lateral tilt in non-labouring term pregnant women. Br J Anaesth. 2012;109:950–6.
Armstrong S, Fernando R, Columb M, Jones T. Cardiac index in term pregnant women in the sitting, lateral, and supine positions: an observational, crossover study. Anesth Analg. 2011;113:318–22.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The experiments comply with the current regulations in Hong Kong that local Ethics Committee approval for the study was granted and the patient who’s data is reported agreed to its publication.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
1.1 Explanation of the AV signal
Examination of the supra-sternal USCOM scan reveals several characteristic signals in addition to AV flow (Table 1). Some of these signals are used in the Fremantle and Cattermole scoring systems [7, 18].
There are several flow signals and vibrations that originate within the thorax and the AV flow signal is just one. However, the output of the left ventricle across the AV is directly towards the USCOM probe (AV flow) and provides the maximum and dominant velocity flow signal that the USCOM probe detects. The main objective when using supra-sternal Doppler is to identify and capture this AV flow signal. It can be difficult to locate in the elderly or low CO patients because of low signal intensity [22]. The cross-sectional CT scan shows the origins of some of these additional flow waves (Fig. 4).
-
a.
The pulmonary artery (PA) lies next to the aortic root so blood flow from the right side of the heart must also be detected by the USCOM. However, the direction of its flow in relation to the beam is more tangential which reduces the Doppler flow velocity to around one-third of the AV signal. However, the same volume of blood flow is detected so the intensity, or pixel density, is greater. The problem for beginners is mistaking this intense PA signal for the AV signal. However, the PA signal can also be a very useful guide when focusing the probe on the AV valve, especially in the elderly (Fig. 7).
-
b.
A second late systolic waveform, similar to that the PA triangle, is commonly found in the AV flow signal envelop (Fig. 6). Although not totally sure, we believe it to originates from blood flow in the pulmonary veins and left atrium because of its timing and that the USCOM beam crosses near to these vessels.
-
c.
The valves of the heart can produce loud vibrations when they open and close which are heard as heart sounds. They can also be detected by Doppler and are seen as very distinct vertical lines that herald the beginning and end of systole. The lines become more prominent if the valves are diseased or the heart is contracting strongly (Figs. 7, 8). The presence on a scan of the valves opening or closing is a good indicator that the beam is focused on the AV.
-
d.
Although flow across the AV ceases with the end of systole, blood flow still continues at a lower velocity along the aorta due to elastic recoil, as the aorta becomes distended during systole due to the rise in BP. The CSA of the ascending aorta can increase by up to 25 % from 3 to 4 cm2 accounting for a significant proportion of arterial blood flow. The resulting diastolic flow in the ascending aorta is sometimes seen on the USCOM scan as an early diastolic signal (Figs. 7a), especially if the circulation is hyperdynamic.
-
e.
During diastole the left ventricle is filled with blood from the left atrium. There are two phases, (1) opening of the mitral valve and (2) atrial contraction. The USCOM sometime detects this left ventricular filling. In echocardiography these flows are well described and referred to as the E and A-waves (Fig. 8a). Normally the E-wave is larger.
-
f.
The A-wave can be mistaken for another prominent waveform commonly seen on USCOM scans, the false A-wave (Fig. 7). This waveform coincides with the beginning of ventricular contraction and the pre-ejection phase of systole, before the AV opens. It probably represents movement of the heart as it first starts to contract. Anyone familiar with using Doppler soon realizes that any abrupt movement of the probe will cause a high velocity artifact on the screen.
-
g.
Also there are a number of arterial sources of blood flow around the thoracic inlet that can be confused with AV flow: (1) the right brachiocephalic, (2) left carotid and (3) left subclavian. When tortuous, or the probe is misdirected, flow within these arteries is detected by the USCOM which produces a very intense and homogeneous flow profile with well defined systolic and diastolic components (Fig. 8c).
1.2 The pulmonary valve scan
The USCOM can also be used to measure CO across the pulmonary valve (PV) via the anterior chest wall (Fig. 8b), which can be very useful in verifying ones supra-sternal CO readings. However, success when scanning the PV in the supine position can be unpredictable because the lung edge may interrupt the path of the USCOM beam (Fig. 4). During echocardiography examination of the heart via the sternal edge the patient is positioned usually left lateral to address this problem. In anaesthetized and ventilated patients the PV signal is often difficult to locate because it is obscured by the highly echogenic lung edge. One useful trick if the patient is awake and cooperative is to ask them to exhale maximally. During surgery when the patient is draped, access to the chest wall is often restricted which makes the PV readings more difficult to perform. Thus, the supra-sternal approach is usually preferred. During our robotic case it was impossible to access the chest wall and use the PV approach because of strapping and drapes.
Rights and permissions
About this article
Cite this article
Critchley, L.A.H., Huang, L. USCOM—window to the circulation: utility of supra-sternal Doppler in an elderly anaesthetized patient for a robotic cystectomy. J Clin Monit Comput 28, 83–93 (2014). https://doi.org/10.1007/s10877-013-9499-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-013-9499-5