Abstract
Purpose
The influence of left atrial (LA) enlargement on the efficacy of steerable sheath usage during pulmonary vein (PV) isolation is poorly understood. Here, we compared the catheter–tissue contact force (CF) and clinical outcomes between steerable and non-steerable sheaths among patients with different severities of LA enlargement.
Methods
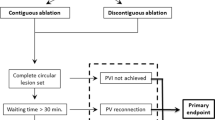
In this prospective observational study, 90 consecutive atrial fibrillation patients scheduled for PV isolation (paroxysmal, 67 %) were enrolled and divided into tertiles of the LA volume (LA1, <124 cm3; LA2, 124 to 145 cm3; LA3, ≥146 cm3). An ipsilateral PV isolation was completed using either a steerable (n = 57) or non-steerable sheath (n = 33).
Results
The average CF of each ipsilateral PV was lower in the LA3 group (right 13.8 ± 5.8 g; left 9.7 ± 5.2 g) than LA1 (right 15.6 ± 6.8 g, p = 0.005; left 12.5 ± 5.6 g, p < 0.0001) or LA2 (right 15.2 ± 7.3 g, p = 0.04; left 12.6 ± 5.3 g, p < 0.0001) groups. In total, the average CF around the left PVs was significantly higher with steerable sheaths than without (12.7 ± 5.5 vs. 10.2 ± 4.9 g, p = 0.03). Subgroup analysis revealed that a tendency toward higher CF around the left PVs was observed in the LA3 group (12.3 ± 7.3 vs. 8.5 ± 3.9 g, p = 0.08) but was not in the LA1 and LA2 groups. Further, in the LA3 group, steerable sheath usage showed better clinical outcomes: shorter procedural (55 ± 29 min vs. 81 ± 39 min, p = 0.04) and fluoroscopic times (27 ± 11 min vs. 37 ± 17 min, p = 0.045) and a tendency toward a lower 1-year AF recurrence rate (39 vs. 12 %, p = 0.09).
Conclusions
The beneficial effects of using steerable sheaths were more prominent in patients with severe LA enlargement.





Similar content being viewed by others
References
Rajappan K, Baker V, Richmond L, Kistler PM, Thomas G, Redpath C, et al. A randomized trial to compare atrial fibrillation ablation using a steerable vs. a non-steerable sheath. Europace. 2009;11:571–5.
Piorkowski C, Eitel C, Rolf S, Bode K, Sommer P, Gaspar T, et al. Steerable versus nonsteerable sheath technology in atrial fibrillation ablation: a prospective, randomized study. Circ Arrhythm Electrophysiol. 2011;4:157–65.
Yokoyama K, Nakagawa H, Shah DC, Lambert H, Leo G, Aeby N, et al. Novel contact force sensor incorporated in irrigated radiofrequency ablation catheter predicts lesion size and incidence of steam pop and thrombus. Circ Arrhythm Electrophysiol. 2008;1:354–62.
Reddy VY, Shah D, Kautzner J, Schmidt B, Saoudi N, Herrera C, et al. The relationship between contact force and clinical outcome during radiofrequency catheter ablation of atrial fibrillation in the TOCCATA study. Heart Rhythm. 2012;9:1789–95.
Andrade JG, Monir G, Pollak SJ, Khairy P, Dubuc M, Roy D, et al. Pulmonary vein isolation using “contact force” ablation: the effect on dormant conduction and long-term freedom from recurrent atrial fibrillation—a prospective study. Heart Rhythm. 2014;11:1919–24.
Neuzil P, Reddy VY, Kautzner J, Petru J, Wichterle D, Shah D, et al. Electrical reconnection after pulmonary vein isolation is contingent on contact force during initial treatment: results from the EFFICAS I study. Circ Arrhythm Electrophysiol. 2013;6:327–33.
Kimura T, Takatsuki S, Oishi A, Negishi M, Kashimura S, Katsumata Y, et al. Operator-blinded contact force monitoring during pulmonary vein isolation using conventional and steerable sheaths. Int J Cardiol. 2014;177:970–6.
Ullah W, Hunter RJ, McLean A, Dhinoja M, Earley MJ, Sporton S, et al. Impact of steerable sheaths on contact forces and reconnection sites in ablation for persistent atrial fibrillation. J Cardiovasc Electrophysiol. 2015;26:266–73.
Sotomi Y, Kikkawa T, Inoue K, Tanaka K, Toyoshima Y, Oka T, et al. Regional difference of optimal contact force to prevent acute pulmonary vein reconnection during radiofrequency catheter ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 2014;25:941–7.
Kumar S, Morton JB, Lee J, Halloran K, Spence SJ, Gorelik A, et al. Prospective characterization of catheter-tissue contact force at different anatomic sites during antral pulmonary vein isolation. Circ Arrhythm Electrophysiol. 2012;5:1124–9.
Hof I, Chilukuri K, Arbab-Zadeh A, Scherr D, Dalal D, Nazarian S, et al. Does left atrial volume and pulmonary venous anatomy predict the outcome of catheter ablation of atrial fibrillation? J Cardiovasc Electrophysiol. 2009;20:1005–10.
Abecasis J, Dourado R, Ferreira A, Saraiva C, Cavaco D, Santos KR, et al. Left atrial volume calculated by multi-detector computed tomography may predict successful pulmonary vein isolation in catheter ablation of atrial fibrillation. Europace. 2009;11:1289–94.
Schluermann F, Krauss T, Biermann J, Hartmann M, Trolese L, Pache G, et al. In vivo contact force measurements and correlation with left atrial anatomy during catheter ablation of atrial fibrillation. Europace. 2015;17:1526–32.
le Polain de Waroux JB, Weerasooriya R, Anvardeen K, Barbraud C, Marchandise S, De Meester C, et al. Low contact force and force-time integral predict early recovery and dormant conduction revealed by adenosine after pulmonary vein isolation. Europace. 2015;17:877–83.
Kautzner J, Neuzil P, Lambert H, Peichl P, Petru J, Cihak R, et al. EFFICAS II: optimization of catheter contact force improves outcome of pulmonary vein isolation for paroxysmal atrial fibrillation. Europace. 2015;17:1229–35.
Acknowledgments
The authors would like to thank Kimoto M, Sakai K, Tagami S, Tamiya I, and Yamaguchi M for their help in collecting the data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Masuda, M., Fujita, M., Iida, O. et al. Steerable versus non-steerable sheaths during pulmonary vein isolation: impact of left atrial enlargement on the catheter–tissue contact force. J Interv Card Electrophysiol 47, 99–107 (2016). https://doi.org/10.1007/s10840-016-0135-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-016-0135-4