Abstract
Primary care physicians are often the first contact for people with mental health concerns. Moreover, many patients with mental health concerns are parents caring for dependent children. The aim of this study was to investigate the family focused practices of a group of primary care physicians when working with patients who are parents and experience mental health concerns. A sequential mixed method design (questionnaire followed by interviews) was employed, early 2015, in general medical settings across six Australian states. Twenty one primary care physicians (12 female, 9 male) across different medical settings completed the Family Focused Mental Health Practice Questionnaire; nine of these were interviewed. Participants reported a moderate amount of family focused practice when working with patients who are parents with mental health issues. Many acknowledged the importance of working with patients on family issues but reported barriers in doing so. Clear guidelines, including the recording of parenting status, need to be in place for primary care physicians working with patients who are parents.
Similar content being viewed by others
References
American Academy of Family Physicians (2001) Mental health care services by family physicians (position paper). http://www.aafp.org/online/en/home/policy/policies/m/mentalhealthcareservices.html. Accessed 1 Apr, 2016.
Bibou-Nakou, I. (2003). ‘Troubles talk’ among professionals working with families facing parental mental illness. Journal of Family Studies, 9, 248–266.
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101.
Britt, H., Miller, G. C., Henderson, J., Charles, J., Valenti, L., & Harrison, C., et al. (2012). General practice activity in Australia 2011–12. General practice series no.31. Sydney: Sydney University Press.
Brockington, I., Chandra, P., Dubowitz, H., Jones, D., Moussa, S., Nakku, J., & Ferre, I. Q. (2011). WPA guidance on the protection and promotion of mental health in children of persons with severe mental disorders. World Psychiatry, 10(2), 93–102.
Carlat, D. J. (1998). The psychiatric review of symptoms: a screening tool for family physicians. American Family Physician, 58(7), 1617–1624.
Creswell, J. W. (2003). Research design. Qualitative, quantitative and mixed method approaches. London: Sage.
Foster, K., Maybery, D., Reupert, A., Gladstone, B., Grant, A., Ruud, T., Falkov, A., & Kowalenko, N. (2016). Family-focused practice in mental health care: an integrative review. Child & Youth Services, 37(2), 129–155.
Gullbrå, F., Smith-Sivertsen, T., Rortveit, G., Anderssen, N., & Hafting, M. (2014). To give the invisible child priority: Children as next of kin in general practice. Scandinavian Journal of Primary Health Care, 32, 17–23.
Hooper, L., Tomek, S., & Newman, C. (2012). Using attachment theory in medical settings: Implications for primary care physicians. Journal of Mental Health, 21(1), 23–37.
Hosman, C., van Doesum, K., & van Santvoort, F. (2009). Prevention of emotional problems and psychiatric risks in children of parents with a mental illness in the Netherlands. Advances in Mental Health, 8, 250–263.
Lid, T. G., & Malterud, K. (2012). General practitioners’ strategies to identify alcohol problems: A focus group study. Scandinavian Journal of Primary Health Care, 30, 64–69.
Leinonen, J., Solantaus, T., & Runamäki, R. -L. (2003). Parental mental health and children’s adjustment: The quality of marital interaction and parenting as mediating factors. Journal of Child Psychology & Psychiatry, 44(2), 227–241.
Lucena, R. J., Lesage, A., Elie, R., Lamontagne, Y., & Corbière, M. (2002). Strategies of collaboration between general practitioners and psychiatrists: a survey of practitioners’ opinions and characteristics. Canadian Journal of Psychiatry, 47(8), 750–758.
Magliano, L., Fiorillo, A., Malangone, C., De Rosa, C., Favata, G., & Sasso, A., et al. (2006). Family psychoeducational interventions for schizophrenia in routine settings: impact on patients’ clinical status and social functioning and on relatives’ burden and resources. Epidemiologia e Psichiatria Sociale, 15, 219–227.
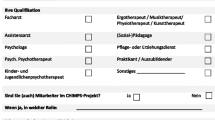
Maybery, D., Goodyear, M., & Reupert, A. (2012). The family focused mental health practice questionnaire. Archives of Psychiatric Nursing, 26(2), 135–144.
Maybery, D., Reupert, A., Patrick, K., Goodyear, M., & Crase, L. (2009). Prevalence of children whose parents have a mental illness. Psychiatric Bulletin, 33(1), 22–26.
Nicholson, J., Reupert, A. E., Grant, A., Lees, R., Maybery, D. J., Mordoch, E., Skogoy, B. E., Stavnes, K. A., & Diggins, M. (2015). The policy context and change for families living with parental mental illness. In A. Reupert, D. Maybery, J. Nicholson, M. Gopfert, M. Seeman (Eds.), Parental psychiatric disorder: Distressed parents and their families (pp. 354–364). Cambridge, UK: Cambridge University Press.
Oldroyd, J., Proudfoot, J., Infante, F. A., Powell Davies, G., Bubner, T., Holton, C., Beilby, J. J., & Harris, M. (2003). Healthcare for people with chronic illness: the views of Australian GPs. Medical Journal of Australia, 179, 30–33.
Pincus, H. A., Tanielian, T. L., Marcus, S. C., Olfson, M., Zarin, D., Thompson, J., & Magno Zito, J. (1998). Prescribing trends in psychotropic medications: primary care, psychiatry, and other medical specialties. Journal of the American Association, 279(7), 526–531.
Reupert, A., & Maybery, D. (2016). What do we know about families where a parent has a mental illness: A systematic review. Child & Youth Services, 37(2), 98–111.
Reupert, A., Morgan, B., & Maybery, D. (2015). The family focused practice of primary care clinicians: A case of missed opportunities. Journal of Mental Health, 24(6), 357–362.
Schwenk, T. L. (2000). Screening for depression in primary care. Journal of the American Medical Association, 284(11), 1379–1380.
Siegenthaler, E., Munder, T., & Egger, M. (2012). Effect of preventive interventions in mentally ill parents on the mental health of the offspring: Systematic review and meta-analysis. Journal of American Child & Adolescent Psychiatry, 51, 8–17.
Skirbekk, H., Middelthon, A. L., Hjortdahl, P., & Finset, A. (2011). Mandates of trust in the doctor-patient relationship. Qualitative Health Research, 21, 1182–1190.
Solantaus, T., Reupert, A., & Maybery, D. (2015). Working with parents who have a psychiatric disorder. In A. Reupert, D. Maybery, J. Nicholson, M. Göpfert, M. Seeman (Eds.), Parental psychiatric disorder: distressed parents and their families (pp. 238–247). London: Cambridge University Press.
The Ambulatory and Hospital Care Statistics Branch of the Centers for Disease Control and Prevention’s National Center for Health Statistics (2008). National ambulatory medical care survey: 2008 summary tables. Available from http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2008_namcs_web_tables.pdf. Accessed 1 Apr 2016.
Williams, J., & Hassett, B. (1996). Sharing the care. General practitioners and public mental health services. Melbourne, Victoria: Department of Human Services.
Funding
This study was supported by the Children of Parents with a Mental Illness national initiative which is funded by the Australian Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Rights and permissions
About this article
Cite this article
Reupert, A., Williamson, C. & Maybery, D. How Family Orientated are Primary Care Physicians?. J Child Fam Stud 26, 329–335 (2017). https://doi.org/10.1007/s10826-016-0558-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-016-0558-7