Abstract
Purpose
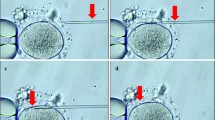
In intracytoplasmic sperm injection (ICSI) of oocytes with a fragile oolemma (fragile oocytes), breakage can occur at injection. In this study, we produced embryos from oocytes with a fragile and normal oolemma (normal oocytes) by ICSI and compared their ability to be fertilized and develop in vitro. We also investigated whether fragile oocyte-derived embryos could implant after blastocyst transfer to determine whether fragile oocytes should be used for assisted reproductive technology treatment.
Methods
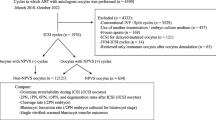
Oocytes were divided into three groups—normal oocytes from cycles containing no fragile oocytes (group A), normal oocytes from cycles containing at least one fragile oocyte (group B), and fragile oocytes (group C), and their fertilization abilities after ICSI and the developmental abilities of resultant embryos were compared.
Results
The fertilization rate in group C (65.3 %) was significantly (P < 0.01) lower than those in groups A (84.6 %) and B (86.9 %), and the degeneration rate in group C (24.2 %) was significantly (P < 0.01) higher than those in groups A (0.71 %) and B (0.28 %). However, there were no significant differences in the blastocyst formation rates (59.7–67.5 %) of embryos among the different groups. In addition, the pregnancy rate after transfer of blastocysts in group C (50.0 %) was not significantly different from those in groups A (35.6 %) and B (45.8 %).
Conclusions
The fertilization ability after ICSI of fragile oocytes is lower than that of normal oocytes but the resultant embryos have the same developmental ability as those of normal oocyte-derived embryos.

Similar content being viewed by others
References
Dumoulin JM, Coonen E, Bras M, Bergers-Janssen JM, Ignoul-Vanvuchelen RC, van Wissen LC, et al. Embryo development and chromosomal anomalies after ICSI: effect of the injection procedure. Hum Reprod. 2001;16:306–12.
Orief Y, Dafopoulos K, Al-Hassani S. Should ICSI be used in non-male factor infertility? Reprod BioMed Online. 2004;9:348–56.
Palermo G, Joris H, Devroey P, Van Steirteghen AC. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992;340:17–8.
Vanderzwalmen P, Bertin G, Lejeune B, Nijs M, Vandamme B, Schoysman R. Two essential steps for a successful intracytoplasmic sperm injection: injection of immobilized spermatozoa after rupture of the oolemma. Hum Reprod. 1996;11:540–7.
Rosen MP, Shen S, Dobson AT, Fujimoto VY, McCulloch CE, Cedars MI. Oocyte degeneration after intracytoplasmic sperm injection: a multivariate analysis to assess its importance as a laboratory or clinical marker. Fertil Steril. 2006;85:1736–43.
Van Steirteghem A, Nagy Z, Joris H, Liu J, Staessen C, Smitz J, et al. High fertilization and implantation rates after intracytoplasmic sperm injection. Hum Reprod. 1993;8:1061–6.
Palermo GD, Alikani M, Bertoli M, Colombero LT, Moy F, Cohen J, et al. Oolemma characteristics in relation to survival and fertilization patterns of oocytes treated by introplasmic sperm injection. Hum Reprod. 1996;11:172–6.
Yanagida K, Katayose H, Suzuki K, Suganuma A, Sat A. Flexibility of oolemma is an important factor for oocyte survival after ICSI. J Mamm Ova Res. 2001;18:93–8.
Nagy ZP, Liu J, Joris H, Bocken G, Desmet B, Van Ranst H, et al. The influence of the site of sperm deposition and mode of oolemma breakage at intracytoplasmic sperm injection of fertilization and embryo developmental rates. Hum Reprod. 1995;10:3171–7.
Cruz M, Gadea B, Garrido N, Pedersen KS, Martínez M, Pérez-Cano I, et al. Embryo quality, blastocyst and ongoing pregnancy rates in oocyte donation patients whose embryos were monitored by time-lapse imaging. J Assist Reprod Genet. 2001;28:569–73.
Zuh D, Zhanq J, Cao S, Zhang J, Heng BC, Huang M, et al. Vitrified-warmed blastocyst cycles yield higher pregnancy and implantation rates compared with fresh blastocyst transfer cycles—time for a new embryo transfer strategy? Fertil Steril. 2011;95:1691–5.
Gardner DK, Lane M, Stevens J, Schlenker T, Schoolcraft WB. Blastocyst score affects implantation and pregnancy outcome: towards a single blastocyst transfer. Fertil Steril. 2000;73:1155–8.
Pribenszky C, Matyas S, Kovacs P, Losonczi E, Zadori J, Vajta G. Pregnancy achieved by transfer of a single blastocyst selected by time-lapse monitoring. Reprod BioMed Online. 2010;21:533–6.
Meseguer M, Herrero J, Tejera A, Hilligsøe KM, Ramsing NB, Remohi J. The use of morphokinetics as a predictor of embryo implantation. Hum Reprod. 2011;26:2658–71.
Mizobe Y, Akiyoshi T, Minami S, Matsuo K, Fukushima R, Yamaguchi A, et al. Effect of a time-lapse incubator (EmbryoScope®) on in vitro culture of human embryos. J Mamm Ova Res. 2014;31:40–4.
Kuwayama M, Vajta G, Kato O, Leibo SP. Highly efficient vitrification method for cryopreservation of human oocytes. Reprod BioMed Online. 2005;11:300–8.
Kuwayama M. Highly efficient vitrification for cryopreservation of human oocytes and embryos: the Cryotop method. Theriogenology. 2007;67:73–80.
Joo BS, Park SH, An BM, Kim KS, Moon SE, Moon HS. Serum estradiol levels during controlled ovarian hyperstimulation influence the pregnancy outcome of in vitro fertilization in a concentration-dependent manner. Fertil Steril. 2010;93:442–6.
Otsuki J, Okada A, Morimoto K, Nagai Y, Kubo H. The relationship between pregnancy outcome and smooth endoplasmic reticulum clusters in MII human oocytes. Hum Reprod. 2004;19:1591–7.
Nagy ZP, Oliveira SA, Abdelmassih V, Abdelmassih R. Novel use of laser to assist ICSI for patients with fragile oocytes: a case report. Reprod BioMed Online. 2002;4:27–31.
Abdelmassih S, Cardoso J, Adbelmassih V, Dias JA, Abdelmassih R, Nagy ZP. Laser-assisted ICSI: a novel approach to obtain higher oocyte survival and embryo quality rates. Hum Reprod. 2002;17:2694–9.
Takahahi I, Hatori A, Nakano H. The usefulness of partial thinning of zona pellucida using a laser-assisted hatching system in ICSI. J Mamm Ova Res. 2013;30:49–52.
Katayose H, Yanagida K, Shinoki T, Kawahara T, Horiguchi T, Sato A. Efficient injection of bull spermatozoa into oocytes using a piezo-driven pipette. Theriogenology. 1999;52:1215–24.
Yanagida K, Katayose H, Yazawa H, Kimura Y, Konnai K, Sato A. The usefulness of a piezo-micromanipulator in intracytoplasmic sperm injection in humans. Hum Reprod. 1999;14:448–53.
Hiraoka K, Hiraoka K, Tamaki T, Nada Y, Kiriake C, Yoshie M, et al. Clinical efficiency of an improved piezo-ICSI method using an ultra-thin micropipette. J Mamm Ova Res. 2013;30:53–8.
Mio Y, Maeda K. Time-lapse cinematography of dynamic changes occurring during in vitro development of human embryos. Am J Obstet Gynecol. 2008;199:660.e1–5.
Mio Y, Iwata K, Yumoto K, Kai Y, Sargant HC, Mizoguchi C, et al. Possible mechanism of polyspermy block in human oocytes observed by time-lapse cinematography. J Assis Reprod Genet. 2012;29:951–6.
Palermo G, Munne S, Cohen J. The human zygote inherits its mitotic potential from the male gamete. Hum Reprod. 1994;9:1220–5.
Acknowledgments
We would like to thank the staff of the Aiiku Ladies Clinic (Kagoshima, Japan).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants
This study was approved by the Institutional Review Board of AIIKUKAI Medical Corporation.
Informed consent
Written informed consent for their treatment and for their outcomes to be described was obtained from all patients.
Additional information
Capsule In intracytoplasmic sperm injection (ICSI) of oocytes with fragile oolemma, breakage can occur at injection. We produced embryos by ICSI of oocytes with fragile and normal oolemma, compared fertilization and development in vitro, and implanted fragile oocyte-derived embryos after blastocyst transfer to determine usability of fragile oocytes in assisted reproduction.
Rights and permissions
About this article
Cite this article
Mizobe, Y., Oya, N., Iwakiri, R. et al. Developmental ability of embryos produced from oocytes with fragile oolemma by intracytoplasmic sperm injection. J Assist Reprod Genet 33, 1685–1690 (2016). https://doi.org/10.1007/s10815-016-0811-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-016-0811-4