Abstract
Purpose
Recent studies have explored the relationship between ABO blood type and serum markers of ovarian reserve, specifically follicle-stimulating hormone (FSH) and anti-mullerian hormone (AMH). The primary objective of this study is to investigate whether there is an association between ABO blood type and ovarian stimulation response in patients with serum markers of diminished ovarian reserve (DOR).
Methods
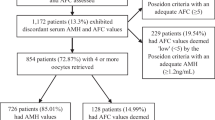
This is a retrospective study of all patients undergoing controlled ovarian stimulation (COS) for in vitro fertilization (IVF) between May 2010 and July 2013. Patients were sub-grouped, a priori, based on serum AMH levels: ≤1 ng/mL, ≤0.5 ng/mL and ≤0.16 ng/mL. Within each sub-group, demographic, baseline IVF characteristics and COS response parameters based on ABO blood types were compared. The number of mature oocytes retrieved was considered the primary outcome. Analysis of variance (ANOVA) and Chi-square tests were used to compare means and percentages between ABO blood types within groups.
Results
Complete data was available for 2575 patients. The mean (± SD) age and BMI of the study cohort was 38.9 (±3.97) years, 23.4 (±5.91) kg/m2, respectively. The distribution of ABO blood types in the cohort was as follows: 36.8 % (A), 6.56 % (AB), 17.3 % (B), and 39.3 % (O). The demographics and baseline IVF characteristics were comparable among patients with blood types A, AB, B, and O within each AMH group. Within each AMH sub-group, no difference was found in the total days of COS, total gonadotropins administered, peak estradiol level, or number of mature oocytes retrieved based on blood type.
Conclusions
Our results suggest no association between ABO blood type and ovarian stimulation response in patients with DOR. The predictive value of ABO blood type in determining ovarian stimulation response in such patients is currently limited.

Similar content being viewed by others
References
Ovarian reserve testing. Committee Opinion No. 618. American College of Obstetricians and Gynecologists. Obstet Gynecol 2015;125:268–73.
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB. A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update. 2006;12(6):685–718.
Scott RT, Toner JP, Muasher SJ, Oehninger S, Robinson S, Rosenwaks Z. Follicle-stimulating hormone levels on cycle day 3 are predictive of in vitro fertilization outcome. Fertil Steril. 1989;51:651–4.
Toner JP, Philput CB, Jones GS, Muasher SJ. Basal follicle-stimulating hormone level is a better predictor of in vitro fertilization performance than age. Fertil Steril. 1991;55:784–91.
Yih MC, Spandorfer SD, Rosenwaks Z. Egg production predicts a doubling of in vitro fertilization pregnancy rates even within defined age and ovarian reserve categories. Fertil Steril. 2005;83(1):24–9.
Reichman DE, Goldschlag D, Rosenwaks Z. Value of antimüllerian hormone as a prognostic indicator of in vitro fertilization outcome. Fertil Steril. 2014;101(4):1012–8.e1.
Nejat EJ, Jindal S, Berger D, Buyuk E, Lalioti M, Pal L. Implications of blood type for ovarian reserve. Hum Reprod. 2011;26(9):2513–7.
de Mouzon J, Hazout A, Cohen-Bacrie M, Belloc S, Cohen-Bacrie P. Blood type and ovarian reserve. Hum Reprod. 2012;27(5):1544–5.
Timberlake KS, Foley KL, Hurst BS, Matthews ML, Usadi RS, Marshburn PB. Association of blood type and patient characteristics with ovarian reserve. Fertil Steril. 2013;100(6):1735–9.
Sengül O, Dilbaz B, Yerebasmaz N, Dede S, Altınbaş S, Erkaya S. Only female age, and not blood type, is associated with ovarian reserve. Int J Fertil Steril. 2014;8(2):143–6.
Lin S, Li R, Chi H, Huang S, Zhang H, Zheng X, et al. Effect of ABO blood type on ovarian reserve in Chinese women. Fertil Steril. 2014;102(6):1729–32.e2.
Pereira N, Elias RT, Levine BA, Lekovich JP, Rosenwaks Z, Spandorfer SD. Association of ABO blood type with ovarian reserve. J Nat Sci. 2015;1(2), e40.
Jayaprakasan K, Campbell B, Hopkisson J, Johnson I, Raine-Fenning N. A prospective, comparative analysis of anti-Müllerian hormone, inhibin-B, and three-dimensional ultrasound determinants of ovarian reserve in the prediction of poor response to controlled ovarian stimulation. Fertil Steril. 2010;93(3):855–64.
Nardo LG, Gelbaya TA, Wilkinson H, Roberts SA, Yates A, Pemberton P, et al. Circulating basal anti-Mullerian hormone levels as predictor of ovarian response in women undergoing ovarian stimulation for in vitro fertilization. Fertil Steril. 2009;92(5):1586–93.
Gleicher N, Weghofer A, Barad DH. Defining ovarian reserve to better understand ovarian aging. Reprod Biol Endocrinol. 2011;9:23.
Matalliotakis I, Cakmak H, Goumenou A, Sifakis S, Ziogos E, Arici A. ABO and Rh blood groups distribution in patients with endometriosis. Arch Gynecol Obstet. 2009;280:917–9.
Yuzhalin AE, Kutikhin AG. ABO and Rh blood groups in relation to ovarian, endometrial and cervical cancer risk among the population of South-East Siberia. Asian Pac J Cancer Prev: APJCP. 2012;13:5091–6.
Binder H, Flegel WA, Emran J, Muller A, Cupisti S, Beckmann MW, et al. Blood group A: an overseen risk factor for early-onset ovarian hyperstimulation syndrome? Reprod Biomed Online. 2008;17:185–9.
Fanchin R, Schonäuer LM, Righini C, Guibourdenche J, Frydman R, Taieb J. Serum anti-Müllerian hormone is more strongly related to ovarian follicular status than serum inhibin B, estradiol, FSH and LH on day 3. Hum Reprod. 2003;18(2):323–7.
Barad DH, Weghofer A, Gleicher N. Comparing anti-Mullerian hormone (AMH) and follicle-stimulating hormone (FSH) as predictors of ovarian function. Fertil Steril. 2009;91(4 Suppl):1553–5.
Spitzer D, Corn C, Stadler J, Wirleitner B, Schuff M, Vanderzwalmen P, et al. Implications of blood type for ovarian reserve and infertility - impact on oocyte yield in IVF patients. Geburtshilfe Frauenheilkd. 2014;74(10):928–32.
Conflict of interest
There is no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Additional information
Summary capsule
Our findings suggest no association between ABO blood type and ovarian stimulation response in patients with diminished ovarian reserve.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Table 1
(DOC 45 kb)
Supplemental Table 2
(DOC 46 kb)
Supplemental Table 3
(DOC 45 kb)
Supplemental Table 4
(DOC 45 kb)
Rights and permissions
About this article
Cite this article
Pereira, N., Hutchinson, A.P., Bender, J.L. et al. Is ABO blood type associated with ovarian stimulation response in patients with diminished ovarian reserve?. J Assist Reprod Genet 32, 985–990 (2015). https://doi.org/10.1007/s10815-015-0485-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-015-0485-3