ABSTRACT
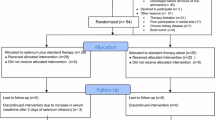
Ischemia/reperfusion injury (IRI) contributes to morbidity and mortality after cardiovascular surgery requiring cardiopulmonary bypass (CPB) and deep hypothermic circulatory arrest (DHCA). Multi-organ damage is associated with substantial decreases of blood selenium (Se) levels in patients undergoing cardiac surgery with CPB. We compared the influence of a dietary surplus of Se and pretreatment with ebselen, a mimic of the selenoenzyme glutathione peroxidase, on IRI-induced tissue damage and inflammation. Male Wistar rats were fed either a Se-adequate diet containing 0.3 ppm Se or supplemented with 1 ppm Se (as sodium selenite) for 5 weeks. Two other groups of Se-adequate rats received intraperitoneal injection of ebselen (30 mg/kg) or DMSO (solvent control) before surgery. The animals were connected to a heart-lung-machine and underwent 45 min of global ischemia during circulatory arrest at 16 °C, followed by re-warming and reperfusion. Selenite and ebselen suppressed IRI-induced leukocytosis and the increase in plasma levels of tissue damage markers (AST, ALT, LDH, troponin) during surgery but did not prevent the induction of proinflammatory cytokines (IL-6, TNF-α). Both Se compounds affected phosphorylation and expression of proteins related to stress response and inflammation: Ebselen increased phosphorylation of STAT3 transcription factor in the heart and decreased phosphorylation of ERK1/2 MAP kinases in the lungs. Selenite decreased ERK1/2 phosphorylation and HSP-70 expression in the heart. Pretreatment with selenite or ebselen protected against acute IRI-induced tissue damage during CPB and DHCA. Potential implications of their different actions with regard to molecular stress markers on the recovery after surgery represent promising targets for further investigation.







Similar content being viewed by others
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CPB:
-
Cardiopulmonary bypass
- DHCA:
-
Deep hypothermic circulatory arrest
- EFSA:
-
European food safety authority
- ERK1/2:
-
Extracellular-regulated kinases-1/2
- GPx:
-
Glutathione peroxidase
- HO-1:
-
Heme oxygenase-1
- HSP-70:
-
Heat shock protein-70
- IL:
-
Interleukin
- IRI:
-
Ischemia/reperfusion injury
- LDH:
-
Lactate dehydrogenase
- LPS:
-
Lipopolysaccharide
- NAC:
-
N-acetyl cysteine
- ROS/RNS:
-
Reactive oxygen and nitrogen species
- SIRS:
-
Systemic inflammatory response syndrome
- STAT3:
-
Signal transducer and activator of transcription-3
- TNF-α:
-
Tumor necrosis factor-α
REFERENCES
Svyatets, M., K. Tolani, M. Zhang, G. Tulman, and J. Charchaflieh. 2010. Perioperative management of deep hypothermic circulatory arrest. Journal of Cardiothoracic and Vascular Anesthesia 24: 644–655.
Luehr, M., J. Bachet, F.W. Mohr, and C.D. Etz. 2014. Modern temperature management in aortic arch surgery: the dilemma of moderate hypothermia. European Journal of Cardio-Thoracic Surgery 45: 27–39.
Tsai, J.Y., W. Pan, S.A. Lemaire, P. Pisklak, V.V. Lee, A.W. Bracey, M.A. Elayda, O. Preventza, M.D. Price, C.D. Collard, and J.S. Coselli. 2013. Moderate hypothermia during aortic arch surgery is associated with reduced risk of early mortality. Journal of Thoracic and Cardiovascular Surgery 146: 662–667.
Hall, R. 2013. Identification of inflammatory mediators and their modulation by strategies for the management of the systemic inflammatory response during cardiac surgery. Journal of Cardiothoracic and Vascular Anesthesia 27: 983–1033.
Rayman, M.P. 2012. Selenium and human health. Lancet 379: 1256–1268.
Fairweather-Tait, S.J., Y. Bao, M.R. Broadley, R. Collings, D. Ford, J.E. Hesketh, and R. Hurst. 2011. Selenium in human health and disease. Antioxidants and Redox Signaling 14: 1337–1383.
Steinbrenner, H., and H. Sies. 2009. Protection against reactive oxygen species by selenoproteins. Biochimica et Biophysica Acta 1790: 1478–1485.
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies), 2014. Scientific opinion on dietary reference values for selenium. EFSA Journal. 12:3846, doi:10.2903/j.efsa.2014.3846 (2014)
Huang, Z., A.H. Rose, and P.R. Hoffmann. 2012. The role of selenium in inflammation and immunity: from molecular mechanisms to therapeutic opportunities. Antioxidants and Redox Signaling 16: 705–743.
Gandhi, U.H., N. Kaushal, K.C. Ravindra, S. Hegde, S.M. Nelson, V. Narayan, H. Vunta, R.F. Paulson, and K.S. Prabhu. 2011. Selenoprotein-dependent up-regulation of hematopoietic prostaglandin D2 synthase in macrophages is mediated through the activation of peroxisome proliferator-activated receptor (PPAR) gamma. Journal of Biological Chemistry 286: 27471–27482.
Steinbrenner, H., S. Al-Quraishy, M.A. Dkhil, F. Wunderlich, and H. Sies. 2015. Dietary selenium in adjuvant therapy of viral and bacterial infections. Advances in Nutrition 6: 1–10.
Stoppe, C., G. Schälte, R. Rossaint, M. Coburn, B. Graf, J. Spillner, G. Marx, and S. Rex. 2011. The intraoperative decrease of selenium is associated with the postoperative development of multiorgan dysfunction in cardiac surgical patients. Critical Care Medicine 39: 1879–1885.
Bar-Or, D., and R.E. Garrett. 2011. Is low plasma selenium concentration a true reflection of selenium deficiency and redox status in critically ill patients? Critical Care Medicine 39: 2000–2001.
Angstwurm, M.W., L. Engelmann, T. Zimmermann, C. Lehmann, C.H. Spes, P. Abel, R. Strauss, A. Meier-Hellmann, R. Insel, J. Radke, J. Schüttler, and R. Gärtner. 2007. Selenium in intensive care (SIC): results of a prospective randomized, placebo-controlled, multiple-center study in patients with severe systemic inflammatory response syndrome, sepsis, and septic shock. Critical Care Medicine 35: 118–126.
Sakr, Y., V.P. Maia, C. Santos, J. Stracke, M. Zeidan, O. Bayer, and K. Reinhart. 2014. Adjuvant selenium supplementation in the form of sodium selenite in postoperative critically ill patients with severe sepsis. Critical Care 18: R68. doi:10.1186/cc13825.
Schomburg, L. 2014. Selenium in sepsis—substitution, supplementation or pro-oxidative bolus? Critical Care 18: 444. doi:10.1186/cc13963.
Forceville, X. 2013. The effect of selenium therapy on mortality in patients with sepsis syndrome: simple selenium supplementation or real (5 H2O)·Na2SeO3 pharmacological effect? Critical Care Medicine 41: 1591–1592.
Guo, F., N. Monsefi, A. Moritz, and A. Beiras-Fernandez. 2012. Selenium and cardiovascular surgery: an overview. Current Drug Safety 7: 321–327.
Schewe, T. 1995. Molecular actions of ebselen—an antiinflammatory antioxidant. General Pharmacology 26: 1153–1169.
Parnham, M.J., and H. Sies. 2013. The early research and development of ebselen. Biochemical Pharmacology 86: 1248–1253.
Wang, X., J.W. Yun, and X.G. Lei. 2014. Glutathione peroxidase mimic ebselen improves glucose-stimulated insulin secretion in murine islets. Antioxidants and Redox Signaling 20: 191–203.
M. Engels, E. Bilgic, A. Pinto, E. Vasquez, L. Wollschläger, H. Steinbrenner, K. Kellermann, P. Akhyari, A. Lichtenberg, U. Boeken. A cardiopulmonary bypass with deep hypothermic circulatory arrest rat model for the investigation of the systemic inflammation response and induced organ damage. J. Inflamm. (Lond). 11, 26. doi: 10.1186/s12950-014-0026-3 (2014).
Barnes, K.M., J.K. Evenson, A.M. Raines, and R.A. Sunde. 2009. Transcript analysis of the selenoproteome indicates that dietary selenium requirements of rats based on selenium-regulated selenoprotein mRNA levels are uniformly less than those based on glutathione peroxidase activity. Journal of Nutrition 139: 199–206.
Jungwirth, B., G.B. Mackensen, M. Blobner, F. Neff, B. Reichart, E.F. Kochs, and G. Nollert. 2006. Neurologic outcome after cardiopulmonary bypass with deep hypothermic circulatory arrest in rats: description of a new model. Journal of Thoracic and Cardiovascular Surgery 131: 805–812.
Pinto, A., D.T. Juniper, M. Sanil, L. Morgan, L. Clark, H. Sies, M.P. Rayman, and H. Steinbrenner. 2012. Supranutritional selenium induces alterations in molecular targets related to energy metabolism in skeletal muscle and visceral adipose tissue of pigs. Journal of Inorganic Biochemistry 114: 47–54.
Cheng, W.H., Y.S. Ho, B.A. Valentine, D.A. Ross, G.F. Combs Jr., and X.G. Lei. 1998. Cellular glutathione peroxidase is the mediator of body selenium to protect against paraquat lethality in transgenic mice. Journal of Nutrition 128: 1070–1076.
Oster, O., G. Schmiedel, and W. Prellwitz. 1988. The organ distribution of selenium in German adults. Biological Trace Element Research 15: 23–45.
Armstrong, S.C. 2004. Protein kinase activation and myocardial ischemia/reperfusion injury. Cardiovascular Research 61: 427–436.
Boengler, K., D. Hilfiker-Kleiner, H. Drexler, G. Heusch, and R. Schulz. 2008. The myocardial JAK/STAT pathway: from protection to failure. Pharmacology and Therapeutics 120: 172–185.
Willis, M.S., and C. Patterson. 2010. Hold me tight: role of the heat shock protein family of chaperones in cardiac disease. Circulation 122: 1740–1751.
Yoshida, T., N. Maulik, Y.S. Ho, J. Alam, and D.K. Das. 2001. H(mox-1) constitutes an adaptive response to effect antioxidant cardioprotection: a study with transgenic mice heterozygous for targeted disruption of the Heme oxygenase-1 gene. Circulation 103: 1695–1701.
Maulik, N., and D.K. Das. 2002. Redox signaling in vascular angiogenesis. Free Radical Biology and Medicine 33: 1047–1060.
Baker, W.L., M.W. Anglade, E.L. Baker, C.M. White, J. Kluger, and C.I. Coleman. 2009. Use of N-acetylcysteine to reduce post-cardiothoracic surgery complications: a meta-analysis. European Journal of Cardio-Thoracic Surgery 35: 521–527.
Venardos, K., G. Harrison, J. Headrick, and A. Perkins. 2004. Selenium supplementation and ischemia-reperfusion injury in rats. Redox Report 9: 317–320.
Brüning, C.A., M. Prigol, C. Luchese, C.R. Jesse, M.M. Duarte, S.S. Roman, and C.W. Nogueira. 2012. Protective effect of diphenyl diselenide on ischemia and reperfusion-induced cerebral injury: involvement of oxidative stress and pro-inflammatory cytokines. Neurochemical Research 37: 2249–2258.
Stoedter, M., K. Renko, A. Hög, and L. Schomburg. 2010. Selenium controls the sex-specific immune response and selenoprotein expression during the acute-phase response in mice. Biochemistry Journal 429: 43–51.
Hoffmann, F.W., A.C. Hashimoto, L.A. Shafer, S. Dow, M.J. Berry, and P.R. Hoffmann. 2010. Dietary selenium modulates activation and differentiation of CD4 + T cells in mice through a mechanism involving cellular free thiols. Journal of Nutrition 140: 1155–1161.
Takada, M., K.C. Nadeau, G.D. Shaw, K.A. Marquette, and N.L. Tilney. 1997. The cytokine-adhesion molecule cascade in ischemia/reperfusion injury of the rat kidney. Inhibition by a soluble P-selectin ligand. J. Clin. Invest. 99: 2682–2690.
Zhang, F., W. Yu, J.L. Hargrove, P. Greenspan, R.G. Dean, E.W. Taylor, and D.K. Hartle. 2002. Inhibition of TNF-alpha induced ICAM-1, VCAM-1 and E-selectin expression by selenium. Atherosclerosis 161: 381–386.
Montgomery, J.B., J.J. Wichtel, M.G. Wichtel, M.A. McNiven, J.T. McClure, F. Markham, and D.W. Horohov. 2012. Effects of selenium source on measures of selenium status and immune function in horses. Canadian Journal of Veterinary Research 76: 281–291.
Liu, H., Q. Lu, and K. Huang. 2010. Selenium suppressed hydrogen peroxide-induced vascular smooth muscle cells calcification through inhibiting oxidative stress and ERK activation. Journal of Cellular Biochemistry 111: 1556–1564.
Bell, R.M., S.P. Kunuthur, C. Hendry, D. Bruce-Hickman, S. Davidson, and D.M. Yellon. 2013. Matrix metalloproteinase inhibition protects CyPD knockout mice independently of RISK/mPTP signalling: a parallel pathway to protection. Basic Research in Cardiology 108: 331.
Santos, N.C., J. Figueira-Coelho, J. Martins-Silva, and C. Saldanha. 2003. Multidisciplinary utilization of dimethyl sulfoxide: pharmacological, cellular, and molecular aspects. Biochemical Pharmacology 65: 1035–1041.
Zou, W., R.A. Roth, H.S. Younis, L.D. Burgoon, and P.E. Ganey. 2010. Oxidative stress is important in the pathogenesis of liver injury induced by sulindac and lipopolysaccharide cotreatment. Toxicology 272: 32–38.
Acknowledgments
We thank A. Borchardt and T. Becher (Institute for Biochemistry and Molecular Biology I) for the excellent technical assistance. The authors are grateful for the continuous support of Dr. M. Sager and Dr. E. Engelhardt (Central animal care facility).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by a grant (F/07/12) of Deutsche Stiftung für Herzforschung (Frankfurt a.M., Germany) to Dr. Bilgic, Dr. Boeken, and Dr. Steinbrenner and by a grant (STE 1782/2-2) of Deutsche Forschungsgemeinschaft (DFG; Bonn, Germany) to Dr. Steinbrenner and by the generous support of the S. Bunnenberg Foundation.
Disclosures
The authors declare that they have no conflict of interest.
Ethical Approval
All applicable international, national, and institutional guidelines for the care and use of animals were followed.
The study (approval number 87-51.04.2010.A334) was approved by the local authority LANUV (Landesamt für Natur, Umwelt und Verbraucherschutz NRW) and carried out in accordance with German and European guidelines of laboratory animal care.
Additional information
Drs. Akhyari and Lichtenberg are co-senior authors of this work.
Holger Steinbrenner and Esra Bilgic contributed equally to this work.
ELECTRONIC SUPPLEMENTARY MATERIAL
Below is the link to the electronic supplementary material.
Supplementary Figure S1
(PPT 173 kb)
Supplementary Table 1
(DOC 116 kb)
Rights and permissions
About this article
Cite this article
Steinbrenner, H., Bilgic, E., Pinto, A. et al. Selenium Pretreatment for Mitigation of Ischemia/Reperfusion Injury in Cardiovascular Surgery: Influence on Acute Organ Damage and Inflammatory Response. Inflammation 39, 1363–1376 (2016). https://doi.org/10.1007/s10753-016-0368-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-016-0368-5