Abstract
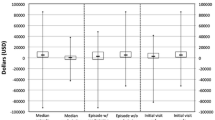
This paper is an examination of hospital 30-day readmission costs using data from 119 acute care hospitals operated by the U.S. Veterans Administration (VA) in fiscal year 2011. We applied a two-part model that linked readmission probability to readmission cost to obtain patient level estimates of expected readmission cost for VA patients overall, and for patients discharged for three prevalent conditions with relatively high readmission rates. Our focus was on the variable component of direct patient cost. Overall, managers could expect to save $2140 for the average 30-day readmission avoided. For heart attack, heart failure, and pneumonia patients, expected readmission cost estimates were $3432, $2488 and $2278. Patient risk of illness was the dominant driver of readmission cost in all cases. The VA experience has implications for private sector hospitals that treat a high proportion of chronically ill and/or low income patients, or that are contemplating adopting bundled payment mechanisms.
Similar content being viewed by others
Notes
Both of these models are drawn from the GLM class. The logistic distribution has heavier tails than the normal distribution on which the probit model is based; however, the two models produce very similar results in practice over a very wide range of values.
Retransformation from the log scale to the natural scale requires exponentiating the log scale error term. This usually does not exponentiate to one, so that the exponentiated predicted values are misleading [21]. Suitable retransformation techniques have been developed [22]; however, serious bias results in subsequent inference unless heteroscedasticity is properly characterized and applied to the retransformation process [3, 21, 23]. This process is generally not practical when there are continuous variables or there is heteroscedasticity across multiple factors.
In order to account for hospital-level clustering, we used the generalized estimating equation (GEE) technique [24] to estimate the GLM parameters for both parts of the 2PM. GEE focuses on estimating the average response over the population rather than predictions for individual patients.
The DCG approach maps 15,000 ICD-9-CM codes to clinically homogeneous diagnostic groups which are further aggregated into 184 clinically and expenditure-similar categories. It then places the groups into body system/clinical condition specific hierarchies called Hierarchical Condition Categories (HCCs). Patients are classified into multiple HCCs based on their respective ICD-9 codes. Each HCC is weighted and aggregated into a patient specific risk score.
The number of chronic conditions is limited to one per category as defined by the AHRQ Clinical Classifications Software (CCS), a tool for clustering ICD-9-CM diagnosis and procedure codes into a manageable number of clinically meaningful categories.
We conducted exploratory analysis to examine the extent of collinearity in our data. The Belsley Kuh Welsch diagnostics [27] indicated a very weak collinear relationship between DCG risk and high severity.
We dropped outpatient visits and weekend discharge based on unstable coefficient signs on these variables, a classic symptom of multicollinearity.
The GEE method is not a likelihood based method, hence the AIC (Akaike’s Information Criterion) statistic is not supported. Rather, we used the QIC (Quasi-likelihood under the Independence model Criterion) statistic [28] to compare models using different working correlation structures. Our results are based on the exchangeability structure, which implies that all distinct members of a cluster are equally correlated with each other.
References
Jencks SF, Williams MV, Coleman EA (2009) Rehospitalizations among patients in the medicare fee-for-service program. N Engl J Med 360:1418–1428
Cutler DM (2010) How health care reform must bend the cost curve. Health Aff 29:1131–1135
Mullahy J (1998) Much ado about two: reconsidering retransformation and the two-part model in health econometrics. J Health Econ 17:247–281
McCullagh P, Nelder JA (1989) Generalized linear models. Chapman & Hall, London
Carey K, Stefos T (2011) Measuring the cost of hospital adverse patient safety events. Health Econ 20:1417–1430
Manning WG, Mullahy J (2001) Estimating log models: to transform or not to transform? J Health Econ 20:461–494
Barnett PG (2009) An improved set of standards for finding cost for cost-effectiveness analysis. Med Care 47:S82–S88
Behnood B, Wayda B, Bao H, Ross JS, Xu X, Chaudhry S, Spertus JA, Bernheim SM, Lindenauer PK, Krumholz HM (2014) Place of residence and outcomes of patients with heart failure. Circ Cardiovasc Qual Outcomes. doi:10.1161/CIRCOUTCOMES.113.000911
Hu J, Gonsahn MD, Nerenz DR (2014) Socioeconomic status and readmission: evidence from an urban teaching hospital. Health Aff 33:1–8
Medicare Payment Advisory Commission. June (2013). Refining the hospital readmission reduction program. In: report to the congress: medicare and the health care delivery system
Ash AS, Ellis RP, Pope GC, Ayanian JZ, Bates DW, Burstin H, Iezzoni LI, MacKay E, Yu W (2000) Using diagnoses to describe populations and predict costs. Health Care Financ Rev 21:7–28
Ellis RP, Pope GC, Iezzoni LI et al (1996) Diagnosis-based risk adjustment for medicare capitation payments. Health Care Financ Rev 17:101–128
Friedman B, Jiang HJ, Elixhauser A, Segal A (2006) hospital inpatient costs for adults with multiple chronic conditions. Med Care Res Rev 63:327–346
Friedman B, Jiang J, Elixhauser A (2008) Costly hospital readmissions and complex chronic illness. Inquiry 45:408–421
Kaboli PJ, Go JT, Hockenberry J, Glasgow JM, Johnson SR, Rosenthal GE, Jones MP, Vaughn-Sarrazin M (2012) Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals. Ann Intern Med 157:837–45
Carey K (2014) Measuring the hospital length of stay/readmission cost trade-off under a bundled payment mechanism. Health Econ. doi:10.1002/hec.3061
Coleman EA, Parry C, Chalmers S et al (2006) The care transitions intervention: results of a randomized controlled trial. Arch Intern Med 166:1822–1828
Kind AJ, Smith MA, Frytak JR et al (2007) Bouncing back: patterns and predictors of complicated transitions 30 days after hospitalizations for acute ischemic stroke. J Am Geriatr Soc 55:365–373
Carey K (2000) A multilevel modeling approach to analysis of patient costs under managed care. Health Econ 9:435–446
O’Brien W, Chen Q, Hull HJ, Shwartz M, Borzecki AM, Hanchate A, Rosen AK (2014) What is the value of adding medicare data in estimating VA hospital readmission rates? Health Serv Res. doi:10.1111/1475-6773.12207
Manning WG (1998) The logged dependent variable, heteroscedasticity, and the retransformation problem. J Health Econ 17:283–295
Duan N (1983) Smearing estimate: a nonparametric retransformation method. J Am Stat Assoc 78:605–610
Blough DK, Ramsey SD (2000) Using generalized linear models to assess medical care costs. Health Serv Outcome Res Methodol 1:185–202
Liang KY, Zeger SL (1986) Longitudinal data analysis using generalized linear models. Biometrika 73:13–22
Kahn JM, Werner RM, Carson SS, Iwashyna TJ (2012) Variation in long-term acute care hospital use after intensive care. Med Care Res Rev 69:339–350
Medicare Payment Advisory Commission. June (2004). Defining long-term care hospitals. In: report to the congress: new approaches in medicare
Belsley DA, Kuh E, Welsch RE (1980) Regression diagnostics: identifying influential data and sources of collinearity. Wiley, New York
Pan W (2001) Akaike’s information criterion in generalized estimating equations. Biometrics 57:120–125
Acknowledgments
Funding for this study was provided by the VA Office of Quality, Safety and Value. The authors also acknowledge Eileen Moran, Peter Almenoff, and the efforts of the VA Office of Productivity, Efficiency and Staffing in support of this work. The opinions are solely those of the authors, and do not necessarily reflect those of the U.S. Department of Veterans Affairs or Boston University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carey, K., Stefos, T. The cost of hospital readmissions: evidence from the VA. Health Care Manag Sci 19, 241–248 (2016). https://doi.org/10.1007/s10729-014-9316-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-014-9316-9