Abstract
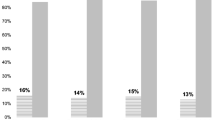
Currently, most breast cancer (BC) patients receive face-to-face genetic counseling (DNA-intake) prior to BRCA-mutation testing, with generic information regarding hereditary BC and BRCA-mutation testing. This prospective study evaluated a novel format: replacing the intake consultation with telephone, written and digital information sent home, and face-to-face contact following BRCA-mutation testing (DNA-direct). From August 2011 to February 2012, 161 of 233 eligible BC patients referred to our Human Genetics department chose between DNA-direct (intervention) or DNA-intake (control). Exclusion criteria were psychological problems (n = 33), difficulty with Dutch text (n = 5), known BRCA-family (n = 3), non-BRCA-referral (n = 1). 30 declined genetic counseling or study participation. Participants received questionnaires including satisfaction and psychological distress. 59 % chose DNA-direct (p = 0.03), of whom 90 % were satisfied and would choose DNA-direct again (including 6/8 BRCA-mutation carriers); although 27 % hesitated to recommend DNA-direct to other patients. General distress (GHQ-12, p = 0.001) and heredity-specific distress (IES, p = 0.02) scored lower in DNA-direct than DNA-intake, both at baseline and follow-up 2 weeks after BRCA-result disclosure; all scores remained below clinical relevance. DNA-direct participants reported higher website use (53 vs. 32 %, p = 0.01), more referrer information about personal consequences (41 vs. 20 %, p = 0.004) and lower decisional conflict (median 20 [0–88] vs. 25 [0–50], p = 0.01). Processing time in DNA-direct was reduced by 1 month. Mutation detection rate was 8 % in both groups. All BRCA-mutation carriers fulfilled current testing criteria. In conclusion, more BC patients preferred DNA-direct over intake consultation prior to BRCA-mutation testing, the majority being strongly to moderately satisfied with the procedure followed, without increased distress.

Similar content being viewed by others
References
Salemink S, Dekker N, Kets CM, van der Looij E, van Zelst-Stams WA, Hoogerbrugge N (2013) Focusing on patient needs and preferences may improve genetic counseling for colorectal cancer. J Genet Couns 22(1):118–124. doi:10.1007/s10897-012-9519-5
Antoniou A, Pharoah PD, Narod S, Risch HA, Eyfjord JE, Hopper JL, Loman N, Olsson H, Johannsson O, Borg A, Pasini B, Radice P, Manoukian S, Eccles DM, Tang N, Olah E, nton-Culver H, Warner E, Lubinski J, Gronwald J, Gorski B, Tulinius H, Thorlacius S, Eerola H, Nevanlinna H, Syrjakoski K, Kallioniemi OP, Thompson D, Evans C, Peto J, Lalloo F, Evans DG, Easton DF (2003) Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 72(5):1117–1130
Chen S, Parmigiani G (2007) Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 25(11):1329–1333
King MC, Marks JH, Mandell JB (2003) Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 302(5645):643–646
Trainer AH, Lewis CR, Tucker K, Meiser B, Friedlander M, Ward RL (2010) The role of BRCA mutation testing in determining breast cancer therapy. Nat Rev Clin Oncol 7(12):708–717
van der Velde NM, Mourits MJ, Arts HJ, de Vries J, Leegte BK, Dijkhuis G, Oosterwijk JC, de Bock GH (2009) Time to stop ovarian cancer screening in BRCA1/2 mutation carriers? Int J Cancer 124(4):919–923
Bylund CL, Fisher CL, Brashers D, Edgerson S, Glogowski EA, Boyar SR, Kemel Y, Spencer S, Kissane D (2012) Sources of uncertainty about daughters’ breast cancer risk that emerge during genetic counseling consultations. J Genet Couns 21(2):292–304. doi:10.1007/s10897-011-9400-y
Kurian AW, Sigal BM, Plevritis SK (2010) Survival analysis of cancer risk reduction strategies for BRCA1/2 mutation carriers. J Clin Oncol 28(2):222–231
Henselmans I, Sanderman R, Smink A, Ranchor AV, de Vries J (2010) Waiting times in breast disease clinics and psychological well-being: speedy care is better care. Ned Tijdschr Geneeskd 154:B491
van Oostrom I, Tibben A (2004) A counselling model for BRCA1/2 genetic susceptibility testing. Hered Cancer Clin Pract 2(1):19–23
Hilgart JS, Coles B, Iredale R (2012) Cancer genetic risk assessment for individuals at risk of familial breast cancer. Cochrane Datab Syst Rev 2:CD003721. doi:10.1002/14651858.CD003721.pub3
Kessels RP (2003) Patients’ memory for medical information. J R Soc Med 96(5):219–222
Overbeek LI, Hermens RP, van Krieken JH, Adang EM, Casparie M, Nagengast FM, Ligtenberg MJ, Hoogerbrugge N (2010) Electronic reminders for pathologists promote recognition of patients at risk for Lynch syndrome: cluster-randomised controlled trial. Virchows Arch 456(6):653–659
Landsbergen KM, Prins JB, Brunner HG, Hoogerbrugge N (2011) Shortened time interval between colorectal cancer diagnosis and risk testing for hereditary colorectal cancer is not related to higher psychological distress. Fam Cancer 10(1):51–57
Sie AS, Spruijt L, van Zelst-Stams WA, Mensenkamp AR, Ligtenberg MJ, Brunner HG, Prins JB, Hoogerbrugge N (2012) DNA-testing for BRCA1/2 prior to genetic counselling in patients with breast cancer: design of an intervention study, DNA-direct. BMC Womens Health 12:12. doi:10.1186/1472-6874-12-12
Pieterse A, van Dulmen S, Ausems M, Schoemaker A, Beemer F, Bensing J (2005) QUOTE-gene(ca): development of a counselee-centered instrument to measure needs and preferences in genetic counseling for hereditary cancer. Psycho-Oncology 14(5):361–375. doi:10.1002/pon.853
Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, Rutter C (1997) The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 27(1):191–197
Horowitz M, Wilner N, Alvarez W (1979) Impact of event scale: a measure of subjective stress. Psychosom Med 41(3):209–218
van der Ploeg E, Mooren TT, Kleber RJ, van der Velden PG, Brom D (2004) Construct validation of the Dutch version of the impact of event scale. Psychol Assess 16(1):16–26
Bottomley A, Aaronson NK (2007) International perspective on health-related quality-of-life research in cancer clinical trials: the European Organisation for Research and Treatment of Cancer experience. J Clin Oncol 25(32):5082–5086
Hopwood P, Shenton A, Lalloo F, Evans DG, Howell A (2001) Risk perception and cancer worry: an exploratory study of the impact of genetic risk counselling in women with a family history of breast cancer. J Med Genet 38(2):139
Lerman C, Daly M, Masny A, Balshem A (1994) Attitudes about genetic testing for breast-ovarian cancer susceptibility. J Clin Oncol 12(4):843–850
Koedoot N, Molenaar S, Oosterveld P, Bakker P, de Graeff A, Nooy M, Varekamp I, de Haes H (2001) The decisional conflict scale: further validation in two samples of Dutch oncology patients. Patient Educ Couns 45(3):187–193
O’Connor AM (2010) User Manual—Decisional Conflict Scale (16 item statement format). http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Decisional_Conflict.pdf
Berg S van de, Gielissen MF, Prins JB (2010) Validation of an empowerment questionnaire in breast cancer survivors. In: 12th World Congress of Psycho-Oncology
van Oostrom I, Meijers-Heijboer H, Lodder LN, Duivenvoorden HJ, van Gool AR, Seynaeve C, van der Meer CA, Klijn JG, van Geel BN, Burger CW, Wladimiroff JW, Tibben A (2003) Long-term psychological impact of carrying a BRCA1/2 mutation and prophylactic surgery: a 5-year follow-up study. J Clin Oncol 21(20):3867–3874
Comprehensive Cancer Centres the Netherlands (2010) Oncoline Guideline: hereditary breast/ovarian cancer
Walsh MC, Trentham-Dietz A, Schroepfer TA, Reding DJ, Campbell B, Foote ML, Kaufman S, Barrett M, Remington PL, Cleary JF (2010) Cancer information sources used by patients to inform and influence treatment decisions. J Health Commun 15(4):445–463. doi:10.1080/10810731003753109
Metcalfe KA, Mian N, Enmore M, Poll A, Llacuachaqui M, Nanda S, Sun P, Hughes KS, Narod SA (2012) Long-term follow-up of Jewish women with a BRCA1 and BRCA2 mutation who underwent population genetic screening. Breast Cancer Res Treat 133(2):735–740. doi:10.1007/s10549-011-1941-0
Rahman B, Meiser B, Watts K, Gleeson M, Saunders C, Mitchell G, Barlow-Stewart K, Kirk J, Tucker K (2012) Evaluation of the efficacy of two models of delivering information about treatment-focused genetic testing among young women newly diagnosed with breast cancer. Paper presented at the European Meeting on Psychosocial Aspects of Genetics 2012, Nuernberg, Germany, June 25 2012
Voorwinden JS, Jaspers JP, ter Beest JG, Kievit Y, Sijmons RH, Oosterwijk JC (2012) The introduction of a choice to learn pre-symptomatic DNA test results for BRCA or Lynch syndrome either face-to-face or by letter. Clin Genet 81(5):421–429. doi:10.1111/j.1399-0004.2011.01811.x
Platten U, Rantala J, Lindblom A, Brandberg Y, Lindgren G, Arver B (2012) The use of telephone in genetic counseling versus in-person counseling: a randomized study on counselees’ outcome. Fam Cancer. doi:10.1007/s10689-012-9522-x
Olaya W, Esquivel P, Wong JH, Morgan JW, Freeberg A, Roy-Chowdhury S, Lum SS (2009) Disparities in BRCA testing: when insurance coverage is not a barrier. Am J Surg 198(4):562–565. doi:10.1016/j.amjsurg.2009.07.003
Van Riel E, Warlam-Rodenhuis CC, Verhoef S, Rutgers EJ, Ausems MG (2010) BRCA testing of breast cancer patients: medical specialists’ referral patterns, knowledge and attitudes to genetic testing. Eur J Cancer Care 19(3):369–376. doi:10.1111/j.1365-2354.2008.01065.x
Acknowledgments
The authors would like to acknowledge M. F. W. J. Ariaans, H. J. van der Looij and M. Voorendt for genetic counseling of patients; P. Manders for statistical expertise; and all the participants for their cooperation. The study is funded by the Radboud University Medical Centre.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Wendy A.G. van Zelst-Stams and Liesbeth Spruijt have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Sie, A.S., van Zelst-Stams, W.A.G., Spruijt, L. et al. More breast cancer patients prefer BRCA-mutation testing without prior face-to-face genetic counseling. Familial Cancer 13, 143–151 (2014). https://doi.org/10.1007/s10689-013-9686-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-013-9686-z