Abstract
The aim of this study was to describe the type of risk-reducing gynaecologic surgery (RRGS) and the extent of pathological evaluation being undertaken for Australasian women at high familial risk of pelvic serous cancer. Surgical and pathology reports were reviewed for women with BRCA1/BRCA2 mutations, or a family history of breast and ovarian cancer, who underwent RRGS between 1998 and 2008. “Adequate” surgery was defined as complete removal of all ovarian and extra-uterine fallopian tube tissue. “Adequate” pathology was defined as paraffin embedding of all removed ovarian and tubal tissue. Predictors of adequacy were assessed using logistic regression. There were 201 women, including 173 mutation carriers, who underwent RRGS. Of these, 91% had adequate surgery and 23% had adequate pathology. Independent predictors of adequate surgery were surgeon type (OR = 20; 95% CI 2–167; P = 0.005 for gynaecologic oncologists versus general gynaecologists), more recent surgery (OR = 1.33/year; 95% CI 1.07–1.67; P = 0.012) and younger patient age (OR = 0.93/year of age; 95% CI 0.87–0.99; P = 0.028). Independent predictors of adequate pathology were more recent surgery (OR = 1.26/year; 95% CI 1.06–1.49; P = 0.008) and surgeon type (OR = 3.1; 95% CI 1.4–6.7; P = 0.004 for gynaecologic oncologists versus general gynaecologists). Four serous ovarian cancers and one endometrioid endometrial cancer were detected during surgery or pathological examination. In conclusion Australasian women attending a specialist gynaecologic oncologist for RRGS are most likely to have adequate surgery and pathological examination. Additional education of clinicians and consumers is needed to ensure optimal surgery and pathology in these women.
Similar content being viewed by others
Introduction
Women carrying a mutation in the breast cancer predisposition genes BRCA1 or BRCA2 have a 40–85% cumulative risk of invasive breast cancer to age 70 and a 15–65% cumulative risk of invasive pelvic serous cancer to age 70 [1–5]. The term “pelvic serous cancer” is used because the majority of BRCA1- and BRCA2-associated gynaecologic cancers appear to originate in the fimbrial end of the fallopian tube rather than the ovary, although they resemble, and have typically been labelled as “serous ovarian cancer” at diagnosis [6]. Women with a family history of breast and “ovarian” cancer, but no identified BRCA1 or BRCA2 mutation in the family, are also considered to be at an elevated risk of pelvic serous cancer [7]. This risk increases as the number of “ovarian” cancer cases in the family increases [8].
Risk-reducing salpingo-oophorectomy (RRSO) is the most effective method of reducing pelvic serous cancer risk in women at high familial risk [9–11] and it is the most effective means available of decreasing gynaecologic cancer mortality [12, 13]. In BRCA1 and BRCA2 mutation carriers RRSO is estimated to reduce the risk of pelvic serous cancers by 80% and the risk of breast cancer by 50% [14]. Because there is no adequate screening strategy for pelvic serous cancers, RRSO is recommended for women at high familial risk once they have completed child bearing [15–17].
The recommended risk-reducing surgery involves complete resection of the ovaries and fallopian tubes up to their insertion into the cornua of the uterus [15, 17–20] as well as inspection of the peritoneal cavity for macroscopic evidence of malignancy. Removal of the uterus is optional and there have been no reports of malignant transformation in the intramural portion of the fallopian tube when the uterus has not been removed [21, 22]. Peritoneal lavage is not routinely recommended for risk-reducing procedures; however, cytological evaluation of peritoneal washings may increase the chance of detecting malignancy [12, 23, 24].
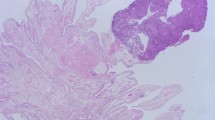
There is no universal protocol for the pathological evaluation of specimens from RRSO. Sectioning and microscopic examination of both fallopian tubes and ovaries in toto by an experienced gynaecological pathologist is recommended [12, 15–18, 20, 25–27]. There is no universal recommendation regarding the number of sections although embedding the ovaries and tubes in their entirety and cutting at least one section from each 2–3 mm paraffin block maximises the detection of occult cancer [16, 25, 27, 28]. In mutation carriers up to 85% of the malignancies detected at RRSO are located in the fallopian tubes, especially in the fimbria, and complete removal and thorough evaluation of these regions is important [25, 29].
Reported rates for occult malignancy of the ovaries and/or fallopian tubes following RRSO range from 0.6 to 18.5%. [9, 10, 18, 24, 26, 27, 29–31] This variability may be due to differences between the studies in terms of sample size, proportion of mutation carriers in the sample, age of included women, extent of pathological evaluation and type of surgery.
We sought to describe the type of surgery and the extent of pathological evaluation performed in Australasian BRCA1 and BRCA2 mutation carriers and other women at high familial risk of “ovarian cancer” who undergo risk-reducing gynaecologic surgery (RRGS) and to document the frequency of occult carcinomas.
Patients and methods
Participants were females enrolled in the Kathleen Cuningham Foundation Consortium for Research into Familial Breast Cancer (kConFab), a resource of data and biospecimens from multiple-case breast cancer families [32, 33]. Eligibility criteria are available on the website [32]. Families are recruited via 16 Family Cancer Clinics in Australia and New Zealand. At enrolment, blood is drawn for possible future BRCA mutation analysis and epidemiology and family history questionnaires are completed. A separately funded and run follow-up study updates cancer events, epidemiological and lifestyle risk factors and uptake of preventative strategies on all female participants every 3 years using a mailed self-administered questionnaire [34]. Cancer events and surgeries are verified where possible with pathology and surgical reports. All participants provide written informed consent and the study has ethics approval at all recruitment sites.
Women were eligible for the current study if they had: undergone RRGS after enrolment in kConFab, completed at least one round of three-yearly follow-up, a documented deleterious mutation in BRCA1 or BRCA2 or a strong family history of breast cancer and at least one case of “ovarian cancer”, no personal history of gynaecological cancer and, both an operation report and a pathology report available from their surgery. Women with a personal history of breast cancer, without evidence of distant metastatic disease at the time of RRGS, were included. Non-carriers within a BRCA1 or BRCA2 mutation-carrying family were excluded.
Date and type of surgery, type of surgeon and macroscopic findings at surgery were determined from operation reports where possible, or from surgical correspondence and pathology reports. Reason for surgery was determined from self report by the women and from operation reports. Surgeries were performed by the surgeon of the woman’s choice at multiple sites throughout Australia and New Zealand and often in institutions not linked with the Family Cancer Centre that the woman had attended. The term “adequate” was used to describe surgical procedures where all ovarian and extra-uterine fallopian tube tissue was completely removed.
For the purposes of this study, we defined surgeon type as follows: general surgeons were registered fellows of the Royal Australasian College of Surgeons; general gynaecologists were registered fellows of the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG); gynaecologic oncologists were gynaecologists who also held the Certification or Diploma in Gynaecologic Oncology of the RANZCOG [35].
Details of the pathological evaluation, the presence of occult cancers and the information communicated from surgeon to pathologist were abstracted from pathology reports. The term “adequate” was used to describe pathological examinations where all removed ovarian and tubal tissue was paraffin embedded. In the absence of a universal protocol, we did not define a minimum number of sections to be cut and examined.
New primary gynaecological cancers following RRGS were self-reported and/or reported by enrolled family members in the three-yearly follow-up questionnaire and verified where possible from pathology reports. The duration of follow-up was calculated from the date of RRGS to the date of death or last contact.
Statistical analysis
Differences in the proportion of patients receiving adequate surgery, by surgeon type were tested for using Fisher′s Exact Test. Odds ratios and their 95% confidence intervals and associated P-values were estimated by logistic regression. All multivariable models included age at RRGS (continuous), year of RRGS (continuous) and surgeon type. Due to lack of evidence of independent association in the final multivariable models we did not include as covariables the type of surgery performed (for the evaluation of adequacy of surgery) and whether or not it was noted in the pathology request form that the sample was from a woman at high risk (for the evaluation of adequacy of pathology). Additional covariates considered for both evaluations were mutation status (mutation carrier versus non-carrier or untested), prior personal history of breast cancer and first degree relatives with ovarian cancer.
All P-values were two sided, and those less than 0.05 were considered statistically significant. All statistical analyses were carried out using Stata: Release 10 [36].
Results
From February 1998 to March 2008, 403 women enrolled in kConFab and completing at least one round of follow-up, had undergone RRGS. Of these, 202 were not eligible for the present study (135 had no documented gene mutation and no family history of ovarian cancer; 13 had a personal history of gynaecological cancer; for 18 an operation report was not available; 1 had no available pathology report; 35 were non-carriers within a mutation carrier family). Characteristics of the remaining 201 women are described in Table 1. There were 102 BRCA1 mutation carriers and 71 BRCA2 mutation carriers.
Tables 2 and 3 summarise the characteristics of the surgeries and pathological examinations, respectively. Overall 20% of women had both adequate surgery and adequate pathological examination. Adequate surgery was performed in 182 women (91%). The remaining women had neither fallopian tube (10 women) or only one tube (9 women) removed. General gynaecologists and general surgeons performed 18 of the 19 inadequate surgeries. Peritoneal washings were collected in 44 women (22%) and the cytology was abnormal in one woman who was diagnosed with ovarian cancer. Based on the pathology reports, 23% of women had adequate pathological evaluation.
Tables 4 and 5 present a summary of the characteristics of the women by the adequacy of surgery and pathology review, respectively, and the results of univariable and multivariable analyses exploring the associations between them. Multivariable analysis confirmed that the independent predictors of adequate surgery were surgeon type, year of surgery and younger patient age. Gynaecologic oncologists were more likely to perform adequate surgery than general gynaecologists (OR = 20; 95% CI 2,167; P = 0.005) and general surgeons (OR = 89; 95% CI 8,1031; P < 0.001). Regardless of surgeon type, more recent surgery was also more likely to be adequate (OR = 1.33 per year; 95% CI 1.07,1.67; P = 0.012). Only 3 of the 19 inadequate surgeries were performed after 2004. The independent predictors of adequate pathological examination were more recent surgery (OR = 1.26; 95% CI 1.06,1.49; P = 0.008) and surgeon type. Surgeries performed by gynaecologic oncologists were more likely to be associated with adequate pathology than surgeries performed by general gynaecologists (OR = 3.12; 95% CI 1.4,6.7; P = 0.004).
All women who had a hysterectomy had adequate surgery. There was no difference between abdominal or laparoscopic surgery in terms of adequacy. Clinical notes provided by the surgeon on the pathology request form, were included in 188 pathology reports. Of these 80% documented the woman’s elevated risk for “ovarian” cancer. There was no significant difference between the three surgeon types in documenting the high risk status. Although documenting high risk status predicted for adequate pathology in the univariable analysis it was not an independent predictor of adequate pathology.
Four (2%) pelvic serous cancers were detected at surgery (Table 6). All were in mutation carriers and all were reported as ovarian in origin although there was little detail in any about the degree of pathological scrutiny of the fallopian tubes. Tubal carcinoma in situ was not reported in any of the 201 cases. The youngest age at cancer diagnosis was 40 years in a BRCA1 mutation carrier. One endometrioid adenocarcinoma of the uterus was diagnosed in a woman with no documented genetic mutation but a past history of breast cancer and tamoxifen-related post-menopausal bleeding.
During the follow-up period (median 35 months) one peritoneal adenocarcinoma was reported in a 70-year-old BRCA1 mutation carrier, 8 years after RRGS. She had undergone adequate surgery but inadequate pathological examination. Six deaths were reported during follow-up and all were attributed to metastatic breast cancer.
Discussion
This prospective study of RRGS in Australasian women at high familial and genetic risk for pelvic serous cancer has revealed the majority had adequate surgery, the minority had adequate pathological evaluation, and the detection rate for occult cancers (2%) was relatively low. Because many pelvic serous cancers in mutation carriers are believed to originate in the tubal fimbria [6,] it is particularly concerning that 9% of operations left extra-uterine fallopian tubes in situ. As expected, more recent year of surgery was associated with more adequate surgery and pathology reflecting improved knowledge of the surgeons and pathologists over time.
Surgery performed by a specialised gynaecologic oncologist was more likely to be adequate. This may reflect greater awareness of the high cancer risk for these women and the importance of complete removal of both ovaries and tubes. Surgeries performed by gynaecologic oncologists were also more likely to be associated with adequate pathology, possibly because gynaecologic oncologists are more likely to practice within large teaching hospitals with academic pathology departments performing better quality examinations.
Only 23% of pathology reports documented that ovarian and tubal tissues were embedded in toto. Ensuring all tissue is embedded maximises the ability to detect microscopic occult cancers and, because only the embedded tissue is saved, it allows repeat examination of tissues at a later date if required. Our result compares poorly with others in the literature. In one recent multi-institutional study of RRSO in BRCA1/2 mutation carriers, pathology reports from 385 women were centrally reviewed and 59% documented embedding and examining the ovaries and fallopian tubes in toto [37]. Two other smaller series reported full sectioning of the ovaries and fallopian tubes in 74% [24] and 33% of women, respectively [18]. In the former series all cases with full sectioning had surgery performed at one specialised institution while none of the cases where surgery was performed by outside institutions had full sectioning performed [24]. The fact that surgical procedures in our study were performed at numerous centres across Australia and New Zealand, each with a different pathology laboratory, may have contributed to our result.
Four serous ovarian cancers, one endometrioid endometrial cancer and no fallopian tube cancers were diagnosed at RRGS. Three of the serous ovarian cancers were in BRCA1 mutation carriers. This is consistent with the literature where the majority of reported occult carcinomas arise in BRCA1 mutation carriers [18, 29, 38]. Our “occult cancer” rate of 2% was at the lower end of the reported range (0.6–18.5%) [9, 10, 18, 24, 26, 27, 29–31] but was comparable to the 2.5% rate recently reported in a review of 647 mutation carriers [37] and to the 0.6% rate from another review of 175 mutation carriers [31]. Our apparent low cancer rate may be a result of the majority of patients having inadequate pathological examinations. Cancer detection rates of 1–3% are reported for confirmed mutation carriers in series without documentation of pathological technique [10, 39], but much higher rates of 10–26% are reported when thorough pathological examination with serial sectioning is mandated [16, 40]. For example, in one series of 67 BRCA1/2 mutation carriers undergoing RRGS, a protocol of complete removal and 2 mm serial sectioning of both ovaries and fallopian tubes was the strongest predictor of occult cancer detection, and was more important than age and mutation type [16].
Most pathology reports in this study did not document the number of sections taken from each ovary and tube. Pathology reports should be improved to include details of how the tissue was processed and examined so that physicians caring for high risk women can be assured that the tissue has been thoroughly examined. We believe a standardised tissue processing and reporting protocol is required to ensure all women have the same extent of pathological examination and to ensure early stage malignancies are not missed. Many “ovarian cancers” in mutation carriers are now thought to originate in the tubal fimbriae [41, 42] and pathologists must be made aware of this to ensure the tubes and fimbria are fully embedded and thoroughly sectioned and examined.
Although communication of high cancer risk from surgeon to pathologist was not an independent predictor of adequate pathology, educating surgeons to include this information on the pathology request form is still important. Ovaries and fallopian tubes removed for reasons other than cancer risk reduction do not require the same extent of pathological evaluation. Without appropriate communication from the surgeon it is difficult for pathologists to determine the specimens needing to be fully embedded and thoroughly examined. It may also be helpful for surgeons to request all tissue be embedded.
Despite our concern that microscopic cancers were missed due to inadequate pathology, only one cancer was diagnosed during follow up. This is consistent with the rates of 1–3% reported in the literature following RRSO. [10, 16, 31, 39] One explanation for this is that any cancers not detected were of early stage and the risk-reducing surgery alone was curative. If true, it could be argued that complete pathological evaluation of removed tissues is of academic interest only and is unlikely to change patient outcomes. Alternatively, our follow-up time may be too short for cancers to manifest. There is insufficient information on the long term clinical consequences of early pelvic serous cancers and further research is required. Thorough pathological evaluation of removed tissue will be important to gather information to enable such research. Women in whom early cancers are detected should be given the options of additional surgical staging, chemotherapy and closer follow-up. Important preventative and therapeutic implications for the future could result from detecting and studying these early cancers.
This study was multi-institutional and thus is likely a true reflection of the management of high risk women in Australia and New Zealand. However, the study has some limitations. We relied on the information detailed in operation and pathology reports to determine the adequacy of surgery and pathology. If the operation report did not describe the procedure in sufficient detail to determine what tissues were removed, we assumed that the tissue received by the pathologist represented the tissue removed by the surgeon. If tissue was removed but not submitted for pathology review we may have underestimated the number of adequate surgeries. We also assumed that ovarian and tubal tissue was not fully embedded if the pathology report did not specifically document this. It is possible that some specimens were embedded in toto but not reported as such. This assumption may have led to an underestimation of the rate of adequate pathological examinations. However, our assumption that tissue that was all embedded was also thoroughly sectioned and examined may have caused us to overestimate the proportion of specimens adequately examined.
Australasian BRCA1 and BRCA2 mutation carriers and women at high familial risk of “ovarian” cancer who elect RRSO must receive high quality care that will reduce their risk of gynaecological cancer. This study highlights the need for standardised surgical techniques and tissue processing protocols for RRSO. Clinicians who discuss RRSO with these women should consider referring them to specialist gynaecologic oncologists for their surgery, or at least should discuss the specifics of optimal surgery and pathology with the woman’s existing gynaecologist or general surgeon if he/she is planning to undertake the surgery. High risk women themselves should be educated about the likely pathogenesis of pelvic serous cancers from the fallopian tubes rather than the ovaries and hence the type of surgery that is optimal. Using the term “ovarian cancer” to describe this disease is misleading and arguably should be abandoned to reflect the emerging evidence regarding the pathogenesis of this disease.
Abbreviations
- RRGS:
-
Risk-reducing gynaecologic surgery
- RRSO:
-
Risk-reducing salpingo-oophorectomy
- kConFab:
-
Kathleen Cuningham Foundation Consortium for Research into Familial Breast Cancer
- RANZCOG:
-
Royal Australian and New Zealand College of Obstetricians and Gynaecologists
- DCIS:
-
Ductal carcinoma in situ
- f/up:
-
Follow-up
- FDR:
-
First degree relative
- BC:
-
Breast cancer
- OC:
-
Ovarian cancer
- BO:
-
Bilateral oophorectomy
- TAH-BSO:
-
Total abdominal hysterectomy and bilateral salpingo-oophorectomy
- N/A:
-
Not available
- R:
-
Right
- L:
-
Left
References
Antoniou A, Pharoah PD, Narod S et al (2003) Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 72(5):1117–1130 [erratum appears in Am J Hum Genet. 2003 Sep;73(3):709]
Ford D, Easton DF, Stratton M et al (1998) Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. The Breast Cancer Linkage Consortium. Am J Hum Genet 62(3):676–689
King MC, Marks JH, Mandell JB (2003) Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 302(5645):643–646
Struewing JP, Hartge P, Wacholder S et al (1997) The risk of cancer associated with specific mutations of BRCA1 and BRCA2 among Ashkenazi Jews. N Engl J Med 336(20):1401–1408
Satagopan JM, Offit K, Foulkes W et al (2001) The lifetime risks of breast cancer in Ashkenazi Jewish carriers of BRCA1 and BRCA2 mutations. Cancer Epidemiol Biomarkers Prev 10(5):467–473
Levanon K, Crum C, Drapkin R (2008) New insights into the pathogenesis of serous ovarian cancer and its clinical impact. J Clin Oncol 26(32):5284–5293
National Breast and Ovarian Cancer Centre (NBOCC) (2011) Familial Risk Assessment - Breast and Ovarian Cancer (FRA-BOC). http://www.nbocc.org.au/fraboc/
Kerber RA, Slattery ML (1995) The impact of family history on ovarian cancer risk. The Utah Population Database. Arch Intern Med 155(9):905–912
Scheuer L, Kauff N, Robson M et al (2002) Outcome of preventive surgery and screening for breast and ovarian cancer in BRCA mutation carriers. [see comment]. J Clin Oncol 20(5):1260–1268
Rebbeck TR, Lynch HT, Neuhausen SL et al (2002) Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med 346(21):1616–1622
Rutter JL, Wacholder S, Chetrit A et al (2003) Gynecologic surgeries and risk of ovarian cancer in women with BRCA1 and BRCA2 Ashkenazi founder mutations: an Israeli population-based case-control study. J Natl Cancer Inst 95(14):1072–1078
Guillem JG, Wood WC, Moley JF et al (2006) ASCO/SSO review of current role of risk-reducing surgery in common hereditary cancer syndromes. J Clin Oncol 24(28):4642–4660
Domchek SM, Friebel TM, Neuhausen SL et al (2006) Mortality after bilateral salpingo-oophorectomy in BRCA1 and BRCA2 mutation carriers: a prospective cohort study. Lancet Oncol 7(3):223–229
Rebbeck TR, Kauff ND, Domchek SM (2009) Meta-analysis of risk reduction estimates associated with risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst 101(2):80–87
Rosen B, Kwon J, Fung Kee Fung M, Gagliardi A, Chambers A (2004) Systematic review of management options for women with a hereditary predisposition to ovarian cancer. Gynecol Oncol 93(2):280–286
Powell CB, Kenley E, Chen LM et al (2005) Risk-reducing salpingo-oophorectomy in BRCA mutation carriers: role of serial sectioning in the detection of occult malignancy. J Clin Oncol 23(1):127–132
Society of Gynecologic Oncologists (2005) Clinical practice committee statement on prophylactic salpingo-oophorectomy. Gynecol Oncol 98(2):179–181
Colgan TJ, Murphy J, Cole DE, Narod S, Rosen B (2001) Occult carcinoma in prophylactic oophorectomy specimens: prevalence and association with BRCA germline mutation status. Am J Surg Pathol 25(10):1283–1289
Paley PJ, Swisher EM, Garcia RL et al (2001) Occult cancer of the fallopian tube in BRCA-1 germline mutation carriers at prophylactic oophorectomy: a case for recommending hysterectomy at surgical prophylaxis. Gynecol Oncol 80(2):176–180
Karlan BY (2004) Defining cancer risks for BRCA germline mutation carriers: implications for surgical prophylaxis. Gynecol Oncol 92(2):519–520
Kauff ND, Barakat RR (2004) Surgical risk-reduction in carriers of BRCA mutations: where do we go from here? Gynecol Oncol 93(2):277–279
Villella JA, Parmar M, Donohue K, Fahey C, Piver MS, Rodabaugh K (2006) Role of prophylactic hysterectomy in patients at high risk for hereditary cancers. Gynecol Oncol 102(3):475–479
Colgan TJ, Boerner SL, Murphy J, Cole DE, Narod S, Rosen B (2002) Peritoneal lavage cytology: an assessment of its value during prophylactic oophorectomy. Gynecol Oncol 85(3):397–403
Lu KH, Garber JE, Cramer DW et al (2000) Occult ovarian tumors in women with BRCA1 or BRCA2 mutations undergoing prophylactic oophorectomy. J Clin Oncol 18(14):2728–2732
Callahan MJ, Crum CP, Medeiros F et al (2007) Primary fallopian tube malignancies in BRCA-positive women undergoing surgery for ovarian cancer risk reduction. J Clin Oncol 25(25):3985–3990
Olivier RI, van Beurden M, Lubsen MA et al (2004) Clinical outcome of prophylactic oophorectomy in BRCA1/BRCA2 mutation carriers and events during follow-up. Br J Cancer 90(8):1492–1497
Leeper K, Garcia R, Swisher E, Goff B, Greer B, Paley P (2002) Pathologic findings in prophylactic oophorectomy specimens in high-risk women. Gynecol Oncol 87(1):52–56
Eisen A, Rebbeck TR, Wood WC, Weber BL (2000) Prophylactic surgery in women with a hereditary predisposition to breast and ovarian cancer. J Clin Oncol 18(9):1980–1995
Finch A, Shaw P, Rosen B, Murphy J, Narod SA, Colgan TJ (2006) Clinical and pathologic findings of prophylactic salpingo-oophorectomies in 159 BRCA1 and BRCA2 carriers. Gynecol Oncol 100(1):58–64
Carcangiu ML, Peissel B, Pasini B, Spatti G, Radice P, Manoukian S (2006) Incidental carcinomas in prophylactic specimens in BRCA1 and BRCA2 germ-line mutation carriers, with emphasis on fallopian tube lesions: report of 6 cases and review of the literature. Am J Surg Pathol 30(10):1222–1230
Rhiem K, Foth D, Wappenschmidt B et al (2010) Risk-reducing salpingo-oophorectomy in BRCA1 and BRCA2 mutation carriers. Arch Gynecol Obstet. 2010/04/30
Kathleen Cunningham Consortium for Research into Familial Breast Cancer: kConFab. http://www.kconfab.org
Mann GJ, Thorne H, Balleine RL et al (2006) Analysis of cancer risk and BRCA1 and BRCA2 mutation prevalence in the kConFab familial breast cancer resource. Breast Cancer Res 8(1):R12
Phillips KA, Butow PN, Stewart AE et al (2005) Predictors of participation in clinical and psychosocial follow-up of the kConFab breast cancer family cohort. Fam Cancer 4(2):105–113
Australian Society of Gynaecologic Oncologists. http://www.asgo.net.au
StataCorp (2007) Stata statistical software. College Station, Texas, USA
Domchek SM, Friebel TM, Garber JE et al (2010) Occult ovarian cancers identified at risk-reducing salpingo-oophorectomy in a prospective cohort of BRCA1/2 mutation carriers. Breast Cancer Res Treat
Lamb JD, Garcia RL, Goff BA, Paley PJ, Swisher EM (2006) Predictors of occult neoplasia in women undergoing risk-reducing salpingo-oophorectomy. Am J Obstet Gynecol 194(6):1702–1709
Kauff ND, Satagopan JM, Robson ME et al (2002) Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N Engl J Med 346(21):1609–1615
Hirst JE, Gard GB, McIllroy K, Nevell D, Field M (2009) High rates of occult fallopian tube cancer diagnosed at prophylactic bilateral salpingo-oophorectomy. Int J Gynecol Cancer 19(5):826–829
Crum CP, Drapkin R, Kindelberger D, Medeiros F, Miron A, Lee Y (2007) Lessons from BRCA: the tubal fimbria emerges as an origin for pelvic serous cancer. Clin Med Res 5(1):35–44
Folkins AK, Jarboe EA, Roh MH, Crum CP (2009) Precursors to pelvic serous carcinoma and their clinical implications. Gynecol Oncol 113(3):391–396
Acknowledgments
This study was funded by the National Health and Medical Research Council (NHMRC) of Australia (#145684, 288704, 454508) and by the National Breast Cancer Foundation and Cancer Australia (#628333). KA Phillips is the Cancer Council Victoria Dr John Colebatch Clinical Research Fellow. JL Hopper is an Australia Fellow of the NHMRC and Victorian Breast Cancer Research Consortium Group Leader. kConFab is supported by grants from the National Breast Cancer Foundation, the National Health and Medical Research Council of Australia and by the Queensland Cancer Fund, the Cancer Councils of New South Wales, Victoria, Tasmania and South Australia, the Cancer Foundation of Western Australia. We wish to thank Heather Thorne, Eveline Niedermayr, all the kConFab research nurses and staff, and the heads and staff of the Family Cancer Clinics for their contributions to this resource, and the many families who contribute to kConFab.
Conflict of interests
None declared.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Kiely, B.E., Friedlander, M.L., Milne, R.L. et al. Adequacy of risk-reducing gynaecologic surgery in BRCA1 or BRCA2 mutation carriers and other women at high risk of pelvic serous cancer. Familial Cancer 10, 505–514 (2011). https://doi.org/10.1007/s10689-011-9435-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-011-9435-0