Abstract
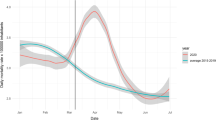
Resettlers (in German: (Spät-)Aussiedler) form one of the biggest migrant groups in Germany. It is known that migrants have different mortality patterns compared to the autochthon population. In this paper, we combined data from three resettler cohorts and examined differences in mortality from non-communicable diseases among resettlers in Germany and the German population. Furthermore, we investigated time trends of cause-specific mortality for 20 years of follow-up and compared it with the German mortality rates. To assess differences in cause-specific mortality between resettlers and the general German population, we calculated standardized mortality ratios (SMRs). To ascertain mortality trends, cause-specific age-standardized mortality rates were calculated and modeled with Poisson regression and fractional polynomials. During the observation period, the study population accumulated almost 800,000 person-years and 5572 deaths were observed. All-cause mortality among resettlers was lower (SMR = 0.91, 95% CI = 0.89–0.94) compared to the general German population, as well as cardiovascular diseases (CVD) mortality (SMR = 0.82, 95% CI = 0.79–0.86). Results for cancer mortality varied considerably by cancer site. Analyses of time trends showed that all-cause and CVD mortality were decreasing over time in resettlers, as well as in the general German population. Lower all-cause mortality among resettlers is mainly explained by lower CVD mortality. Cancer-site specific mortality showed different results. Converging mortality rates may indicate an adaption of lifestyle behavior. However, there are no data on individual risk factors in this study.


Similar content being viewed by others
References
Worbs S, Bund E, Kohls M, Babka von Gostomski C. (Spät-) Aussiedler in Deutschland. Eine Analyse aktueller Daten und Forschungsergebnisse. Nürnberg: Bundesamt für Migration und Flüchtlinge; 2013.
Razum O, Wenner J. Social and health epidemiology of immigrants in Germany: past, present and future. Public Health Rev. 2016;37(1):4.
Bray F, Parkin DM. Descriptive Studies. In: Ahrens W, Pigeot I, editors. Handbook of Epidemiology. 2nd ed. New York: Springer; 2014. p. 187–258.
Marmot MG, Syme SL. Acculturation and coronary heart disease in Japanese–Americans. Am J Epidemiol. 1976;104(3):225–47.
Razum O, Zeeb H, Gerhardus A. Cardiovascular mortality of Turkish nationals residing in West Germany. Ann Epidemiol. 1998;8(5):334–41.
Frisbie WP, Cho Y, Hummer RA. Immigration and the health of Asian and Pacific Islander adults in the United States. Am J Epidemiol. 2001;153(4):372–80.
Deckert A, Winkler V, Paltiel A, Razum O, Becher H. Time trends in cardiovascular disease mortality in Russia and Germany from 1980 to 2007-are there migration effects? BMC Public Health. 2010;10(1):1.
Winkler V, Ott JJ, Holleczek B, Stegmaier C, Becher H. Cancer profile of migrants from the Former Soviet Union in Germany: incidence and mortality. Cancer Causes Control. 2009;20(10):1873–9.
Kyobutungi C, Ronellenfitsch U, Razum O, Becher H. Mortality from external causes among ethnic German immigrants from former Soviet Union countries, in Germany. Eur J Public Health. 2006;16(4):376–82.
Volodina A, Bertsche T, Kostev K, Winkler V, Haefeli WE, Becher H. Drug utilization patterns and reported health status in ethnic German migrants (Aussiedler) in Germany: a cross-sectional study. BMC Public Health. 2011;11(1):1.
Ronellenfitsch U, Kyobutungi C, Becher H, Razum O. All-cause and cardiovascular mortality among ethnic German immigrants from the Former Soviet Union: a cohort study. BMC Public Health. 2006;6(1):1.
Becher H, Razum O, Kyobutungi C, Laki J, Ott JJ, Ronellenfitsch U, et al. Mortalität von Aussiedlern aus der ehemaligen Sowjetunion. Deutsches Aerzteblatt. 2007;104(23):1655–61.
Deckert A, Winkler V, Meisinger C, Heier M, Becher H. Myocardial infarction incidence and ischemic heart disease mortality: overall and trend results in repatriates, Germany. Eur J Public Health. 2014;24(1):127–33.
Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe: epidemiological update. Eur Heart J. 2013;34(39):3028–34.
Ronellenfitsch U, Kyobutungi C, Becher H, Razum O. Large-scale, population-based epidemiological studies with record linkage can be done in Germany. Eur J Epidemiol. 2004;19(12):1073–4.
Hammer GP. Makros zur Berechnung von Personenjahren in epidemiologischen Studien. In: Proceedings der 15 Konferenz der SAS-Anwender in Forschung und Entwicklung. 2011; 223–232.
Greenland S, Rothman KJ. Introduction to Stratified Analysis. In: Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 258–82.
World Health Organization. WHO mortality database. 2015. http://www.who.int/healthinfo/mortality_data/en/ Accessed 05 May 2016.
Gaber E, Wildner M. Themenheft 52 “Sterblichkeit, Todesursachen und regionale Unterschiede”. 2011.
Rittgen W, Becker N. SMR Analysis of Historical Follow-Up Studies with Missing Death Certificates. Biometrics. 2000;56(4):1164–9.
Pace M, Lanzieri G, Glickman M, Zupanič T. Revision of the European Standard Population: report of Eurostat’s task force. Publications Office of the European Union; 2013.
Sauerbrei W, Royston P. Building multivariable prognostic and diagnostic models: transformation of the predictors by using fractional polynomials. J R Stat Soc Ser A (Statistics in Society). 1999;162(1):71–94.
Krieger V, Kampen H, Paulsen N, Kopp L, Schleicher J, Kampen J. Deutsche aus Russland gestern und heute: Volk auf dem Weg. Landsmannschaft der Deutschen aus Russland eV.; 2006.
Razum O, Geiger I, Zeeb H, Ronellenfitsch U. Gesundheitsversorgung von Migranten. Dtsch Arztebl. 2004;101(43):43.
Reiss K, Spallek J, Razum O. ‘Imported risk’or’health transition’? Smoking prevalence among ethnic German immigrants from the Former Soviet Union by duration of stay in Germany-analysis of microcensus data. Int J Equity Health. 2010;9(1):15.
Antecol H, Bedard K. Unhealthy assimilation: why do immigrants converge to American health status levels? Demography. 2006;43(2):337–60.
Turra CM, Elo IT. The impact of salmon bias on the Hispanic mortality advantage: new evidence from social security data. Popul Res Policy Rev. 2008;27(5):515–30.
Gesellschaft der epidemiologischen Krebsregister in Deutschland. GEKID Atlas—C33–C34 Lungenkrebs Mortalität Männer. 2013. http://www.gekid.de/Atlas/CurrentVersion/atlas.html. Accessed 03 Feb 2017.
Kibele EU. Appendices of Regional mortality differences in Germany. In: Kibele EU, editor. Regional mortality differences in Germany. Springer Science & Business Media; 2012. p. 217-71.
Statistische Ämter des Bundes und der Länder. Zensus 2011—Methoden und Verfahren. Wiesbaden: Statistisches Bundesamt; 2015.
Bundesamt für Migration und Flüchtlinge. Migrationsbericht des Bundesamtes für Migration und Flüchtlinge im Auftrag der Bundesregierung. 2016.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016:ehw106.
Kuhrs E, Winkler V, Becher H. Risk factors for cardiovascular and cerebrovascular diseases among ethnic Germans from the former Soviet Union: results of a nested case–control study. BMC Public Health. 2012;12(1):1.
Ganna A, Magnusson PK, Pedersen NL, de Faire U, Reilly M, Ärnlöv J, et al. Multilocus genetic risk scores for coronary heart disease prediction. Arterioscler Thromb Vasc Biol. 2013;33(9):2267–72.
Havulinna AS, Kettunen J, Ukkola O, Osmond C, Eriksson JG, Kesäniemi YA, et al. A blood pressure genetic risk score is a significant predictor of incident cardiovascular events in 32 669 individualsnovelty and significance. Hypertension. 2013;61(5):987–94.
Muka T, Koromani F, Portilla E, O’Connor A, Bramer WM, Troup J, et al. The role of epigenetic modifications in cardiovascular disease: a systematic review. Int J Cardiol. 2016;212:174–83.
Andreassi MG. Metabolic syndrome, diabetes and atherosclerosis: influence of gene–environment interaction. Mutat Res/Fundam Mol Mech Mutagen. 2009;667(1):35–43.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
World Cancer Research Fund International & American Insitute for Cancer Research. Continuous update project report: diet, nutrition, physical activity, and prostate cancer. 2014.
Agudo A, Bonet C, Travier N, González CA, Vineis P, Bueno-de-Mesquita HB, et al. Impact of cigarette smoking on cancer risk in the European prospective investigation into cancer and nutrition study. J Clin Oncol. 2012;30(36):4550–7.
Boffetta P, Hashibe M, La VC, Zatonski W, Rehm J. The burden of cancer attributable to alcohol drinking. Int J Cancer. 2006;119(4):884–7.
World Bank. Fertility rate, total (births per woman). 2016. http://data.worldbank.org/indicator/SP.DYN.TFRT.IN?end=2014&start=1990&view=chart. Accessed 10 Aug 2016.
Hirte L, Nolte E, Bain C, McKee M. Breast cancer mortality in Russia and Ukraine 1963–2002: an age-period-cohort analysis. Int J Epidemiol. 2007;36(4):900–6.
Aparicio ML, Döring A, Mielck A, Holle R. Unterschiede zwischen Aussiedlern und der übrigen deutschen Bevölkerung bezüglich Gesundheit, Gesundheitsversorgung und Gesundheitsverhalten: eine vergleichende Analyse anhand des KORA-Surveys 2000. Sozial-und Präventivmedizin. 2005;50(2):107–18.
Wang F, Meng W, Wang B, Qiao L. Helicobacter pylori-induced gastric inflammation and gastric cancer. Cancer Lett. 2014;345(2):196–202.
Tsukanov VV, Butorin NN, Maady AS, Shtygasheva OV, Amelchugova OS, Tonkikh JL, et al. Helicobacter pylori infection, intestinal metaplasia, and gastric cancer risk in Eastern Siberia. Helicobacter. 2011;16(2):107–12.
Jaehn P, Holleczek B, Becher H, Winkler V. Histologic types of gastric cancer among migrants from the former Soviet Union and the general population in Germany: what kind of prevention do we need? Eur J Gastroenterol Hepatol. 2016;28(8):863–70.
Plummer M, de Martel C, Vignat J, Ferlay J, Bray F, Franceschi S. Global burden of cancers attributable to infections in 2012: a synthetic analysis. Lancet Glob Health. 2016;4(9):e609–16.
Cornberg M, Razavi HA, Alberti A, Bernasconi E, Buti M, Cooper C, et al. A systematic review of hepatitis C virus epidemiology in Europe, Canada and Israel. Liver Int. 2011;31(s2):30–60.
Wichmann H-E, Kaaks R, Hoffmann W, Jöckel K-H, Greiser K, Linseisen J. Die Nationale Kohorte. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz. 2012;55(6–7):781–9.
Acknowledgement
We want to thank to Dr. Amit Gulati, Institute of Medical Biometry and Epidemiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany for valuable comments which improved the paper.
Funding
Volker Winkler and Simone Kaucher were funded by the Deutsche Krebshilfe (Grant number 111232). Heiko Becher and Valentina Leier were supported by the German Federal Ministry of Education and Research (Grant Number 01ER1306 PERGOLA).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Simone Kaucher and Valentina Leier are joint first authors.
Volker Winkler and Heiko Becher are joint senior authors.
Rights and permissions
About this article
Cite this article
Kaucher, S., Leier, V., Deckert, A. et al. Time trends of cause-specific mortality among resettlers in Germany, 1990 through 2009. Eur J Epidemiol 32, 289–298 (2017). https://doi.org/10.1007/s10654-017-0240-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-017-0240-4