Abstract
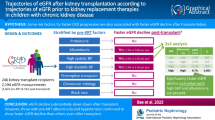
In renal transplantation, serum creatinine (SCr) is the main biomarker routinely measured to assess patient’s health, with chronic increases being strongly associated with long-term graft failure risk (death with a functioning graft or return to dialysis). Joint modeling may be useful to identify the specific role of risk factors on chronic evolution of kidney transplant recipients: some can be related to the SCr evolution, finally leading to graft failure, whereas others can be associated with graft failure without any modification of SCr. Sample data for 2749 patients transplanted between 2000 and 2013 with a functioning kidney at 1-year post-transplantation were obtained from the DIVAT cohort. A shared random effect joint model for longitudinal SCr values and time to graft failure was performed. We show that graft failure risk depended on both the current value and slope of the SCr. Deceased donor graft patient seemed to have a higher SCr increase, similar to patient with diabetes history, while no significant association of these two features with graft failure risk was found. Patient with a second graft was at higher risk of graft failure, independent of changes in SCr values. Anti-HLA immunization was associated with both processes simultaneously. Joint models for repeated and time-to-event data bring new opportunities to improve the epidemiological knowledge of chronic diseases. For instance in renal transplantation, several features should receive additional attention as we demonstrated their correlation with graft failure risk was independent of the SCr evolution.

Similar content being viewed by others

References
Asar Ö, Ritchie J, Kalra PA, Diggle PJ. Joint modelling of repeated measurement and time-to-event data: an introductory tutorial. Int J Epidemiol. 2015;44(1):334–44.
Rizopoulos D. Joint models for longitudinal and time-to-event data: with applications in R. Boca Raton: CRC Press; 2012. p. 279.
Wulfsohn MS, Tsiatis AA. A joint model for survival and longitudinal data measured with error. Biometrics. 1997;53(1):330–9.
Leffondre K, Boucquemont J, Tripepi G, Stel VS, Heinze G, Dunkler D. Analysis of risk factors associated with renal function trajectory over time: a comparison of different statistical approaches. Nephrol Dial Transplant. 2015;30(8):1237–43.
Ibrahim JG, Molenberghs G. Missing data methods in longitudinal studies: a review. Test Madr Spain. 2009;18(1):1–43.
Tsiatis AA, Davidian M. joint modeling of longitudinal and time-to-event data: an overview. Stat Sin. 2004;14:809–34.
Rizopoulos D, Takkenberg JJM. Tools & techniques–statistics: dealing with time-varying covariates in survival analysis–joint models versus Cox models. EuroIntervention. 2014;10(2):285–8.
Andrinopoulou E-R, Rizopoulos D, Jin R, Bogers AJJC, Lesaffre E, Takkenberg JJM. An introduction to mixed models and joint modeling: analysis of valve function over time. Ann Thorac Surg. 2012;93(6):1765–72.
Kalbfleisch JD, Prentice RL. The statistical analysis of failure time data. New York: Wiley; 2011. p. 464.
Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139(2):137–47.
Galichon P, Xu-Dubois Y-C, Finianos S, Hertig A, Rondeau E. Clinical and histological predictors of long-term kidney graft survival. Nephrol Dial Transplant. 2013;28(6):1362–70.
Foucher Y, Daguin P, Akl A, Kessler M, Ladriere M, Legendre C, et al. A clinical scoring system highly predictive of long-term kidney graft survival. Kidney Int. 2010;78(12):1288–94.
Ferro CJ, Hodson J, Moore J, McClure M, Tomson CRV, Nightingale P, et al. Bayesian analysis of glomerular filtration rate trajectories in kidney transplant recipients: a pilot study. Transplantation. 2015;99(3):533–9.
Marcén R, Morales JM, Fernández-Rodriguez A, Capdevila L, Pallardó L, Plaza JJ, et al. Long-term graft function changes in kidney transplant recipients. NDT Plus. 2010;3(Suppl_2):ii2–8.
Pascual M, Theruvath T, Kawai T, Tolkoff-Rubin N, Cosimi AB. Strategies to improve long-term outcomes after renal transplantation. N Engl J Med. 2002;346(8):580–90.
Debout A, Foucher Y, Trébern-Launay K, Legendre C, Kreis H, Mourad G, et al. Each additional hour of cold ischemia time significantly increases the risk of graft failure and mortality following renal transplantation. Kidney Int. 2015;87(2):343–9.
de Bruijne MHJ, Sijpkens YWJ, Paul LC, Westendorp RGJ, van Houwelingen HC, Zwinderman AH. Predicting kidney graft failure using time-dependent renal function covariates. J Clin Epidemiol. 2003;56(5):448–55.
Kasiske BL, Andany MA, Danielson B. A thirty percent chronic decline in inverse serum creatinine is an excellent predictor of late renal allograft failure. Am J Kidney Dis. 2002;39(4):762–8.
Daher Abdi Z, Essig M, Rizopoulos D, Le Meur Y, Prémaud A, Woillard JB, et al. Impact of longitudinal exposure to mycophenolic acid on acute rejection in renal-transplant recipients using a joint modeling approach. Pharmacol Res. 2013;72:52–60.
Moranne O, Maillard N, Fafin C, Thibaudin L, Alamartine E, Mariat C. Rate of renal graft function decline after one year is a strong predictor of all-cause mortality. Am J Transplant. 2013;13(3):695–706.
Rizopoulos D, Ghosh P. A Bayesian semiparametric multivariate joint model for multiple longitudinal outcomes and a time-to-event. Stat Med. 2011;30(12):1366–80.
Garre FG, Zwinderman AH, Geskus RB, Sijpkens YWJ. A joint latent class changepoint model to improve the prediction of time to graft failure. J R Stat Soc Ser A Stat Soc. 2008;171(1):299–308.
Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function-measured and estimated glomerular filtration rate. N Engl J Med. 2006;354(23):2473–83.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–70.
Nankivell BJ, Gruenewald SM, Allen RD, Chapman JR. Predicting glomerular filtration rate after kidney transplantation. Transplantation. 1995;59(12):1683–9.
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41.
Buron F, Hadj-Aissa A, Dubourg L, Morelon E, Steghens J-P, Ducher M, et al. Estimating glomerular filtration rate in kidney transplant recipients: performance over time of four creatinine-based formulas. Transplantation. 2011;92(9):1005–11.
White CA, Akbari A, Doucette S, Fergusson D, Knoll GA. Estimating glomerular filtration rate in kidney transplantation: Is the new chronic kidney disease epidemiology collaboration equation any better? Clin Chem. 2010;56(3):474–7.
Gaspari F, Ferrari S, Stucchi N, Centemeri E, Carrara F, Pellegrino M, et al. Performance of different prediction equations for estimating renal function in kidney transplantation. Am J Transplant. 2004;4(11):1826–35.
Aalen OO, Farewell VT, De Angelis D, Day NE, Gill ON. A Markov model for HIV disease progression including the effect of HIV diagnosis and treatment: application to AIDS prediction in England and Wales. Stat Med. 1997;16(19):2191–210.
R Development Core Team. R: a language and environment for statistical computing [Internet]. Computing RF for S, éditeur. Vienna, Austria; 2010. Disponible sur: http://www.R-project.org/.
Rizopoulos D. JM: an R package for the joint modelling of longitudinal and time-to-event data. J Stat Softw. 2010;35(9):1–33.
Kasiske BL, Israni AK, Snyder JJ, Skeans MA, Peng Y, Weinhandl ED. A simple tool to predict outcomes after kidney transplant. Am J Kidney Dis. 2010;56(5):947–60.
Lenihan CR, O’Kelly P, Mohan P, Little D, Walshe JJ, Kieran NE, et al. MDRD-estimated GFR at one year post-renal transplant is a predictor of long-term graft function. Ren Fail. 2008;30(4):345–52.
Hariharan S, McBride MA, Cherikh WS, Tolleris CB, Bresnahan BA, Johnson CP. Post-transplant renal function in the first year predicts long-term kidney transplant survival. Kidney Int. 2002;62(1):311–8.
Acknowledgments
We wish to thank the DIVAT scientific board (C. Legendre, H. Kreis, L. Rostaing, N. Kamar, E. Morelon, G. Mourad, V. Garrigue, M. Kessler and M. Ladrière) as well as members of the clinical research assistant team (S. Le Floch, A. Petit, J. Posson, C. Scellier, V. Eschbach, K. Zurbonsen, C. Dagot, F. M’Raiagh, V. Godel, X. Longy and P. Przednowed). The DIVAT cohort is partially supported by Roche Laboratory since 1994.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix 1: Mathematical formulation of the shared random effect joint model
Let Y be the longitudinal marker and tij the time of measurement of the jth (j = 1, …, ni) measure for the patient i (i = 1, …, N). Let h(·) denotes the instantaneous risk function of graft failure. The joint model combines a linear mixed model (Eq. 1) with a parametric regression model (Eq. 2). They share the random effects (b0i; b1i).
with (b0i; b1i)T ~MVN(0,B), B an unstructured variance–covariance matrix, X1i a vector of baseline covariates influencing the baseline value of longitudinal marker, X2i another vector of baseline covariates that may change marker evolution over time and β0, β1 two scalars defining the referential value of the baseline level and the slope of the longitudinal biomarker Y(·) respectively, and β2, β3 two p-vectors of the same dimension as X1 and X2 respectively. The evolution of the measurements Yij(tij) are defined by the sum of a subject specific trend mi(tij) plus an error term εij ~ N(0, σ 2ε ). For the instantaneous risk function of graft failure, h0(t) denotes the baseline risk function, and X3i is a vector of baseline covariates that could influence the graft failure risk, with a corresponding vector of fixed regression coefficients γ. g is a function of the true level of the marker mi, which specifies the type of dependence between the longitudinal and the survival processes. Classically, it may be the current level of the marker (g(mi(t)) = αmi(t)), the intensity of marker deterioration during the follow-up i.e. the slope (g(mi(t)) = α2mi′(t)), or both (g(mi(t)) = α1mi(t) + α2mi′(t)) [2]. This latter is the retained association of the model presented in Table 2.
Appendix 2: Clinical interpretations of the joint model parameters
Parameters of the longitudinal process
Due to the log transformation of the longitudinal marker SCr, the parameters in the linear mixed submodel should be interpreted as the log of relative change. The longitudinal equation can be written as follows:
and the SCr evolution can be re-written as:
Qualitative variables
Let Z be a qualitative variable associated with:
-
the 1-year SCr only \(({\text{Z}} \subseteq {\text{X}}_1;\ {\text{Z}}\nsubseteq{\text{X}}_2)\). The excess of SCr for a patient with Z = 1 as compared to the case where Z = 0 for the same patient is:
$$\begin{aligned} {\text{SCr}}({\text{t}}_{\text{ij}} )_{{\left[ {{\text{Z}}_{\text{i}} = 1\,{\text{vs}}\,{\text{Z}}_{\text{i}} = 0} \right]}} & = \frac{{\exp \left( {\upbeta_{0} + {\text{b}}_{{0{\text{i}}}} } \right) \exp \left( {\left( {\upbeta_{1} + {\text{b}}_{{1{\text{i}}}} } \right){\text{t}}_{\text{ij}} } \right)\exp \left( {\upbeta_{2} } \right)}}{{\exp \left( {\upbeta_{0} + {\text{b}}_{{0{\text{i}}}} } \right) \exp \left( {\left( {\upbeta_{1} + {\text{b}}_{{1{\text{i}}}} } \right) {\text{t}}_{\text{ij}} } \right)}} \\ {\text{SCr}}({\text{t}}_{\text{ij}} )_{{\left[ {{\text{Z}}_{\text{i}} = 1\,{\text{vs}}\,{\text{Z}}_{\text{i}} = 0} \right]}} & = \exp \left( {\upbeta_{2} } \right) \\ \end{aligned}$$
This gap of SCr is constant beyond 1-year post-transplantation.
-
Both the 1-year SCr and the SCr increase during the follow-up (Z ⊆ X1; Z ⊆ X2)
$${\text{SCr}}({\text{t}}_{\text{ij}} )_{{\left[ {{\text{Z}}_{\text{i}} = 1\,{\text{vs}}\,{\text{Z}}_{\text{i}} { = }0} \right]}} = \exp \left( {\upbeta_{2} +\upbeta_{3} {\text{t}}_{\text{ij}} } \right)$$
This gap of SCr value is increasing or decreasing during the follow-up according to the sign of β3. For clinical purposes, in the interpretations, we used the time t = 5 to quantify a relative change at 5 years after the first year post-transplantation.
Quantitative variables
Let W1 be a quantitative variable with sdW1 its standard deviation, w a value of W1 and Δ a relevant clinical increase.
-
Let X1 be the standardized version of W1, X2 be null (W1 was associated with the 1-year SCr only).
$$\begin{aligned} {\text{SCr}}\left( {{\text{t}}_{\text{ij}} } \right)\left[ {{\text{W}}_{{1{\text{i}}}} = {\text{w}} + \Delta{\text{ vs W}}_{{1{\text{i}}}}^{{\prime }} = {\text{w}}} \right] & = \frac{{\exp \left( {\upbeta_{0} + {\text{b}}_{{0{\text{i}}}} } \right) \exp \left( {\left( {\upbeta_{1} + {\text{b}}_{{1{\text{i}}}} } \right){\text{t}}_{\text{ij}} } \right) \exp \left( {\upbeta_{2} \left( {\frac{{\left( {{\text{w}} + {{\Delta }}} \right)}}{{{\text{sd}}_{{{\text{W}}1}} }}} \right)} \right)}}{{ \exp \left( {\upbeta_{0} + {\text{b}}_{{0{\text{i}}}} } \right) \exp \left( {\left( {\upbeta_{1} + {\text{b}}_{{1{\text{i}}}} } \right){\text{t}}_{\text{ij}} } \right) \exp \left( {\upbeta_{2} \left( {{\text{w}}/{\text{sd}}_{{{\text{W}}1}} } \right)} \right)}} \\ & = \frac{{ \exp \left( {\upbeta_{2} {\text{w}}/ {\text{sd}}_{{{\text{W}}1}} +\upbeta_{2} {{\Delta }}/ {\text{sd}}_{{{\text{W}}1}} } \right)}}{{ \exp \left( {\upbeta_{2} \left( {{\text{w}}/{\text{sd}}_{{{\text{W}}1}} } \right)} \right)}} \\ & = \exp \left( {\upbeta_{2}\Delta / {\text{sd}}_{{{\text{W}}1}} } \right) \\ \end{aligned}$$ -
Now, let X1 = X2 be the standardized version of W1 (W1 was associated with both the 1-year SCr and the SCr evolution).
$$\begin{aligned} {\text{SCr}}\left( {{\text{t}}_{\text{ij}} } \right)\left[ {{\text{W}}_{{1{\text{i}}}} = {\text{w}} + \Delta{\text{ vs W}}_{{1{\text{i}}}}^{{\prime }} = {\text{w}}} \right] & = \frac{{{ \exp }\left( {{{\upbeta }}_{0} + {\text{b}}_{{0{\text{i}}}} } \right){ \exp }\left( {\left( {\upbeta_{1} + {\text{b}}_{{1{\text{i}}}} } \right){\text{t}}_{\text{ij}} } \right){ \exp }\left( {{{\upbeta }}_{2} \left( {\frac{{\left( {{\text{w}} + {{\Delta }}} \right)}}{{{\text{sd}}_{{{\text{W}}1}} }}} \right)} \right){ \exp }\left( {{{\upbeta }}_{3} {\text{t}}_{\text{ij}} \left( {\frac{{\left( {{\text{w}} + {{\Delta }}} \right)}}{{{\text{sd}}_{{{\text{W}}1}} }}} \right)} \right)}}{{{ \exp }\left( {{{\upbeta }}_{0} + {\text{b}}_{{0{\text{i}}}} } \right){ \exp }\left( {\left( {{{\upbeta }}_{1} + {\text{b}}_{{1{\text{i}}}} } \right){\text{t}}_{\text{ij}} } \right){ \exp }\left( {{{\upbeta }}_{2} \left( {{\text{w}}/{\text{sd}}_{{{\text{W}}1}} } \right)} \right){ \exp }\left( {{{\upbeta }}_{3} {\text{t}}_{\text{ij}} \left( {{\text{w}}/{\text{sd}}_{{{\text{W}}1}} } \right)} \right)}} \\ & = { \exp }\left( {{{\upbeta }}_{2} {{\Delta }}/{\text{sd}}_{{{\text{W}}1}} } \right){ \exp }\left( {{{\upbeta }}_{3} {\text{t}}_{\text{ij}} {{\Delta }}/{\text{sd}}_{{{\text{W}}1}} } \right)) \\ \end{aligned}$$
Hazard ratio for the longitudinal marker
As we have seen in “Appendix 1”, the instantaneous risk function is written as follows:
With \({\text{m}}_{\text{i}} \left( {\text{t}} \right) =\upbeta_{{0{\text{i}}}} +\upbeta_{{1{\text{i}}}} {\text{t}}\) and \(\frac{{\updelta{\text{m}}_{\text{i}} \left( {\text{t}} \right)}}{{\updelta{\text{t}}}} =\upbeta_{{1{\text{i}}}}\)
As we use a log transformation of SCr measurement (Y(t) = log(SCr(t))), the hazard ratio which quantifies the association between the longitudinal marker and the risk of event was expressed for a clinically relevant difference.
-
For the current level of the marker, we can rewrite the HR for a difference of 25 % in SCr values at the same time for the same patient and the same slope:
$$\begin{aligned} {\text{HR}}_{{1.25{\text{SCr}}\left( {\text{t}} \right){\text{vs SCr}}\left( {\text{t}} \right)}} & = \frac{{{\text{h}}_{0} \left( {\text{t}} \right){ \exp }\left( {{{\upgamma }}^{\text{T}} {\text{X}}_{{3{\text{i}}}} + {{\upalpha }}_{1} \log \left( {1.25{\text{SCr}}\left( {\text{t}} \right)} \right) + {{\upalpha }}_{2} {\text{m}}_{\text{i}}^{{\prime }} \left( {\text{t}} \right)} \right)}}{{{\text{h}}_{0} \left( {\text{t}} \right){ \exp }\left( {{{\upgamma }}^{\text{T}} {\text{X}}_{{3{\text{i}}}} + {{\upalpha }}_{1} \log \left( {{\text{SCr}}\left( {\text{t}} \right)} \right) + {{\upalpha }}_{2} {\text{m}}_{\text{i}}^{{\prime }} \left( {\text{t}} \right)} \right)}} \\ & = { \exp }({{\upalpha }}_{1} (\log \left( {1.25{\text{SCr}}\left( {\text{t}} \right)} \right) - \log \left( {{\text{SCr}}\left( {\text{t}} \right)} \right))) \\ & = 1.25^{{{{\upalpha }}_{1} }} \\ \end{aligned}$$ -
For the intensity of the marker, the HR which compares the situation in which \(\frac{\updelta }{\updelta t}{ \log }\left( {{\text{SCr}}_{\text{i}} \left( {\text{t}} \right)} \right) = {\text{s}}_{1}\) to another in which \(\frac{\updelta }{\updelta t}{ \log }\left( {{\text{SCr}}_{\text{i}} \left( {\text{t}} \right)} \right) = {\text{s}}_{2}\), for same covariates X3i and level of SCr at time t is equal. HR = exp(α2(s2 − s1)).
Besides, because we assume a linear model, \(\frac{\updelta }{\updelta t}{ \log }({\text{SCr}}_{\text{i}} \left( {\text{t}} \right))\) is constant, that is ∀t, \(\frac{\updelta }{\updelta t}{ \log }({\text{SCr}}_{\text{i}} \left( {\text{t}} \right)) = {\text{s}}\) for some s ∈ℝ. This implies ∀t′ > t:
$${\text{SCr}}_{\text{i}} \left( {{\text{t}}^{\prime}} \right) = {\text{SCr}}_{\text{i}} \left( {\text{t}} \right){ \exp }\left( {{\text{s}}\left( {{\text{t}}^{\prime} - {\text{t}}} \right)} \right).$$If the SCr increases by x % between t-1 and t, then s = log(1 + x/100) because \({\text{s}} = { \log }\left( {\frac{{{\text{SCr}}_{\text{i}} \left( {\text{t}} \right)}}{{{\text{SCr}}_{\text{i}} \left( {{\text{t}} - 1} \right)}}} \right)\)
This leads to: \({\text{HR}} = { \exp }({{\upalpha }}_{2} \left( {\log \left( {1 + {\text{x}}/100} \right) - \log \left( {1 + {\text{y}}/100} \right)} \right))\) which is the HR which compares an increase of x % between t-1 and t to an increase of y %. In our paper, we choose to compare an increase of 25 % compare to the mean evolution (a growth of 3 % each year).
Hazard ratio for the quantitative variables
Because the quantitative variables have been standardized, the HR for these factors were expressed for an increase of one standard deviation. In order to calculate them for an increase of relevant threshold in the variable unit, we can proceed as follows:
Let X1 be the standardization of W1 with sd1 its standard deviation. HRX is the HR obtained for the standardized variable and HRW is the one for an increase of Δ unit of W1.
Rights and permissions
About this article
Cite this article
Fournier, MC., Foucher, Y., Blanche, P. et al. A joint model for longitudinal and time-to-event data to better assess the specific role of donor and recipient factors on long-term kidney transplantation outcomes. Eur J Epidemiol 31, 469–479 (2016). https://doi.org/10.1007/s10654-016-0121-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-016-0121-2