Abstract
Background
In living donor liver transplantation (LDLT), the hepatic hemodynamics plays important roles in graft regeneration, and the hepatic blood inflows are associated with graft size. However, the data of interplay between the hepatic arterial buffer response (HABR) and graft-to-recipient weight ratio (GRWR) in clinical LDLT are lacking.
Aims
To identify the effect of the HABR on the hepatic hemodynamics and recovery of graft function and to evaluate the safe lower limit of the GRWR in carefully selected recipients.
Methods
Portal venous and hepatic arterial blood flow was measured in recipients with ultrasonography, and the graft functional recovery, various complications, and survive states after LDLT were compared.
Results
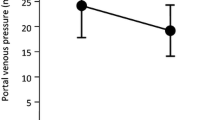
In total, 246 consecutive patients underwent LDLT with right lobe grafts. In total, 26 had a GRWR < 0.7 % (A), 29 had a GRWR between 0.7 and 0.8 % (B), and 181 had a GRWR > 0.8 % (C). For small-for-size syndrome, there was no significant difference (P = 0.176). Graft survival rates at 1, 3, and 5 year were not different (P = 0.710). The portal vein flow and portal vein flow per 100 g graft weight peaks were significantly higher in the A. Hepatic arterial velocity and hepatic arterial flow decreased in all the three groups on postoperative day 1; however, the hepatic arterial flow per 100 g graft weight was close to healthy controls.
Conclusions
HABR played important roles not only in the homeostasis of hepatic afferent blood supply but also in maintaining enough hepatic perfusion to the graft.



Similar content being viewed by others
References
Raia S, Nery JR, Mies S. Liver transplantation from live donors. Lancet. 1989;2:497.
Testa G, Malago M, Broelsch CE. From living related to in situ split liver transplantation: how to reduce waiting-list mortality. Pediatr Transplant. 2001;5:16–20.
Kiuchi T, Kasahara M, Uryuhara K, et al. Impact of graft size mismatching on graft prognosis in liver transplantation from living donors. Transplantation. 1999;67:321–327.
Tanaka K, Ogura Y. “Small-for-size graft” and “small-for-size syndrome” in living donor liver transplantation. Yonsei Med J. 2004;45:1089–1094.
Moon JI, Kwon CH, Joh JW, et al. Safety of small-for-size grafts in adult-to-adult living donor liver transplantation using the right lobe. Liver Transplant. 2010;16:864–869.
Hill MJ, Hughes M, Jie T, et al. Graft weight/recipient weight ratio: how well does it predict outcome after partial liver transplants? Liver Transplant. 2009;15:1056–1062.
Lee SD, Kim SH, Kim YK, et al. Graft-to-recipient weight ratio lower to 0.7 % is safe without portal pressure modulation in right-lobe living donor liver transplantation with favorable conditions. Hepatobiliary Pancreat Dis Int. 2014;13:18–24.
Maetani Y, Itoh K, Egawa H, et al. Factors influencing liver regeneration following living-donor liver transplantation of the right hepatic lobe. Transplantation. 2003;75:97–102.
Kelly DM, Shiba H, Nakagawa S, et al. Hepatic blood flow plays an important role in ischemia-reperfusion injury. Liver Transplant. 2011;17:1448–1456.
Klar E, Angelescu M, Zapletal C, et al. Prediction of primary graft failure by intraoperative quantification of liver perfusion. Transplant Proc. 2001;33:1370–1371.
Jakab F, Sugar I, Rath Z, et al. The relationship between portal venous and hepatic arterial blood flow. I. Experimental liver transplantation. HPB Surg. 1996;10:21–26.
Smyrniotis V, Kostopanagiotou G, Kondi A, et al. Hemodynamic interaction between portal vein and hepatic artery flow in small-for-size split liver transplantation. Transpl Int. 2002;15:355–360.
Liu B, Yan LN, Wang WT, et al. Clinical study on safety of adult-to-adult living donor liver transplantation in both donors and recipients. World J Gastroenterol. 2007;13:955–959.
Bolognesi M, Quaglio C, Bombonato G, et al. Splenic Doppler impedance indices estimate splenic congestion in patients with right-sided or congestive heart failure. Ultrasound Med Biol. 2012;38:21–27.
Imura S, Shimada M, Ikegami T, et al. Strategies for improving the outcomes of small-for-size grafts in adult-to-adult living-donor liver transplantation. J Hepatobiliary Pancreat Surg. 2008;15:102–110.
Henderson JM, Mackay GJ, Kutner MH, Noe B. Volumetric and functional liver blood flow are both increased in the human transplanted liver. J Hepatol. 1993;17:204–207.
Henderson JM, Gilmore GT, Mackay GJ, et al. Hemodynamics during liver transplantation: the interactions between cardiac output and portal venous and hepatic arterial flows. Hepatology. 1992;16:715–718.
Houssin D, Fratacci M, Dupuy P, et al. One week of monitoring of portal and hepatic arterial blood flow after liver transplantation using implantable pulsed Doppler microprobes. Transplant Proc. 1989;21:2277–2278.
Payen DM, Fratacci MD, Dupuy P, et al. Portal and hepatic arterial blood flow measurements of human transplanted liver by implanted Doppler probes: interest for early complications and nutrition. Surgery. 1990;107:417–427.
Marcos A, Olzinski AT, Ham JM, et al. The interrelationship between portal and arterial blood flow after adult to adult living donor liver transplantation. Transplantation. 2000;70:1697–1703.
Dahm F, Georgiev P, Clavien PA. Small-for-size syndrome after partial liver transplantation: definition, mechanisms of disease and clinical implications. Am J Transplant. 2005;5:2605–2610.
Glanemann M, Eipel C, Nussler AK, et al. Hyperperfusion syndrome in small-for-size livers. Eur Surg Res. 2005;37:335–341.
Demetris AJ, Kelly DM, Eghtesad B, et al. Pathophysiologic observations and histopathologic recognition of the portal hyperperfusion or small-for-size syndrome. Am J Surg Pathol. 2006;30:986–993.
Abbasoglu O, Levy MF, Testa G, et al. Does intraoperative hepatic artery flow predict arterial complications after liver transplantation? Transplantation. 1998;66:598–601.
Yanaga K, Shimada M, Makowka L, et al. Significance of blood flow measurement in clinical liver transplantation. Transplant Proc. 1989;21:2330–2331.
Yagi S, Iida T, Taniguchi K, et al. Impact of portal venous pressure on regeneration and graft damage after living-donor liver transplantation. Liver Transplant. 2005;11:68–75.
Acknowledgments
We give great thanks to China Liver Transplant Registry (CLTR, http://www.cltr.org) for data recording.
Funding sources
This study was supported by Grant No. 81170456 from the National Natural Science Foundation of China. The funding source had no involvement, such as the roles of the study design, the collection, analysis, and interpretation of the data, the writing of this manuscript, or the decision to submit this manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Liu, C., Song, Jl., Lu, Ws. et al. Hepatic Arterial Buffer Response Maintains the Homeostasis of Graft Hemodynamics in Patient Receiving Living Donor Liver Transplantation. Dig Dis Sci 61, 464–473 (2016). https://doi.org/10.1007/s10620-015-3881-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3881-8