Abstract
Background and Aim
Intestinal and extra-intestinal complications are associated with inflammatory bowel disease (IBD) but their exact incidence is not well known. In order to improve our understanding of their incidence and impact, we assessed the complications associated with ulcerative colitis (UC) and Crohn’s disease (CD) in a population-based study in Medicaid patients.
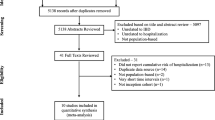
Methods
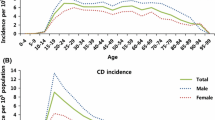
We utilized a retrospective cohort design and identified cases of UC and CD using Medi-Cal, the Medicaid program for the State of California. The disease cohort was age- and gender-matched to four controls each and the intestinal and extra-intestinal complications of CD and UC (analyzed separately) were studied over a period of 5 years following the initial diagnosis.
Results
For UC, the total number of intestinal complications, per 100 cases, was 92 observed compared to 21 expected; the total number of extra-intestinal complications was 42 observed compared to 30 expected. For CD, the number of intestinal complications was 81 observed compared to 20 expected and for extra-intestinal complications, 37 observed compared to 26 expected (all p < 0.001). For both UC and CD, bleeding was the most frequently seen intestinal complication, while the most common extra-intestinal complication was osteoporosis.
Conclusions
IBD is associated with several intestinal and extra-intestinal complications of variable incidence and risk. Success of therapeutic regimens should be measured by decreases in incidence, risks, and costs of these complications, in addition to the usual impact on disease activity.
Similar content being viewed by others
Abbreviations
- CD:
-
Crohn’s disease
- EN:
-
Erythema nodosum
- IBD:
-
Inflammatory bowel disease
- OR:
-
Odds ratio
- UC:
-
Ulcerative colitis
References
Podolsky DK. Inflammatory bowel disease. N Engl J Med. 2002;347:417–429.
National Institute of Diabetes and Digestive and Kidney Diseases. Digestive Diseases in the United States: Epidemiology and Impact. Washington, DC: US Government Printing Office. In; 1994 NIH publication 94–1447.
American Gastroenterological Association. The burden of gastrointestinal diseases. http://www.gastro.org/user-assets/Documents/burden-report.pdf; 1998 Accessed September 10, 2007.
Farmer RG, Hawk WA, Turnbull RB Jr. Clinical patterns in Crohn’s disease: a statistical study of 615 cases. Gastroenterology. 1975;68:627–635.
Greenstein AJ, Janowitz HD, Sachar DB. The extra-intestinal complications of Crohn’s disease and ulcerative colitis: a study of 700 patients. Medicine (Baltimore). 1976;55:401–412.
Monsen U, Sorstad J, Hellers G, Johansson C. Extracolonic diagnoses in ulcerative colitis: an epidemiological study. Am J Gastroenterol. 1990;85:711–716.
Rankin GB, Watts HD, Melnyk CS, Kelley ML Jr. National Cooperative Crohn’s Disease study: extraintestinal manifestations and perianal complications. Gastroenterology. 1979;77:914–920.
Veloso FT, Carvalho J, Magro F. Immune-related systemic manifestations of inflammatory bowel disease. A prospective study of 792 patients. J Clin Gastroenterol. 1996;23:29–34.
Crohn’s & Colitis Foundation of America. http://www.ccfa.org; Accessed October 12, 2007.
California Department of Health Services. Medi-Cal facts and figures. www.chcf.org/documents/policy/MediCalFactsAndFigures2006.pdf; Accessed February 2, 2008.
California Department of Health Services. Medi-Cal payment error study. California Department of Health Services. http://www.dhs.ca.gov/ane/PDF/MPES%20and%20PAM%2001052005.pdf; 2004 Accessed May 17, 2007.
Parc R, Roger V, Penna C. Management of hemorrhage. In: Michelassi F, Milsom JW, eds. Operative strategies in inflammatory bowel disease. New York: Springer; 1999:229–233.
Robert JR, Sachar DB, Greenstein AJ. Severe gastrointestinal hemorrhage in Crohn’s disease. Ann Surg. 1991;213:207–211.
Robert JH, Sachar DB, Aufses AH Jr, Greenstein AJ. Management of severe hemorrhage in ulcerative colitis. Am J Surg. 1990;159:550–555.
Jahnsen J, Falch JA, Mowinckel P, Aadland E. Bone mineral density in patients with inflammatory bowel disease: a population-based prospective two-year follow-up study. Scand J Gastroenterol. 2004;39:145–153.
Schulte C, Dignass AU, Mann K, Goebell H. Reduced bone mineral density and unbalanced bone metabolism in patients with inflammatory bowel disease. Inflamm Bowel Dis. 1998;4:268–275.
Jahnsen J, Falch JA, Aadland E, Mowinckel P. Bone mineral density is reduced in patients with Crohn’s disease but not in patients with ulcerative colitis: a population-based study. Gut. 1997;40:313–319.
Silvennoinen JA, Karttunen TJ, Niemela SE, Manelius JJ, Lehtola JK. A controlled study of bone mineral density in patients with inflammatory bowel disease. Gut. 1995;37:71–76.
Bargiggia S, Maconi G, Elli M, et al. Sonographic prevalence of liver steatosis and biliary tract stones in patients with inflammatory bowel disease: study of 511 subjects at a single center. J Clin Gastroenterol. 2003;36:417–420.
Kratzer W, Haenle MM, Mason RA, von Tirpitz C, Kaechele V. Prevalence of cholelithiasis in patients with chronic inflammatory bowel disease. World J Gastroenterol. 2005;11:6170–6175.
Fraquelli M, Losco A, Visentin S, et al. Gallstone disease and related risk factors in patients with Crohn's disease: analysis of 330 consecutive cases. Arch Intern Med. 2001;161:2201–2204.
Orchard TR, Wordsworth BP, Jewell DP. Peripheral arthropathies in inflammatory bowel disease: their articular distribution and natural history. Gut. 1998;42:387–391.
Salvarani C, Vlachonikolis IG, van der Heijde DM, et al. Musculoskeletal manifestations in a population-based cohort of inflammatory bowel disease patients. Scand J Gastroenterol. 2001;36:1307–1313.
Bernstein CN, Blanchard JF, Rawsthorne P, Yu N. The prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study. Am J Gastroenterol. 2001;96:1116–1122.
Jess T, Gamborg M, Matzen P, Munkholm P, Sorensen TI. Increased risk of intestinal cancer in Crohn’s disease: a meta-analysis of population-based cohort studies. Am J Gastroenterol. 2005;100:2724–2729.
Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48:526–535.
Kappelman MD, Rifas-Shiman SL, Kleinman K, et al. The prevalence and geographic distribution of Crohn’s disease and ulcerative colitis in the United States. Clin Gastroenterol Hepatol. 2007;5:1424–1429.
Competing interests
The authors have no conflicts of interest to declare. This study was sponsored by the Institute of Clinical Outcomes Research and Education (ICORE). In the past 3 years, ICORE has received grant support from Altana, Novartis, Centocor, Pfizer, and Astra-Zeneca.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arora, G., Singh, G., Vadhavkar, S. et al. Incidence and Risk of Intestinal and Extra-intestinal Complications in Medicaid Patients with Inflammatory Bowel Disease: A 5-Year Population-Based Study. Dig Dis Sci 55, 1689–1695 (2010). https://doi.org/10.1007/s10620-010-1236-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-010-1236-z