Abstract
Peritoneal dissemination is diagnosed in 10–25 % of colorectal cancer patients. Selected patients are treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. For these patients, earlier diagnosis, optimised selection criteria and a personalised approach are warranted. Biomarkers could play a crucial role here. However, little is known about possible candidates. Considering tumour cell adhesion as a key step in peritoneal dissemination, we aim to provide an overview of the functional importance of adhesion molecules in peritoneal dissemination and discuss the prognostic, diagnostic and therapeutic options of these candidate biomarkers. A systematic literature search was conducted according to the PRISMA guidelines. In 132 in vitro, ex vivo and in vivo studies published between 1995 and 2013, we identified twelve possibly relevant adhesion molecules in various cancers that disseminate peritoneally. The most studied molecules in tumour cell adhesion are integrin α2β1, CD44 s and MUC16. Furthermore, L1CAM, EpCAM, MUC1, sLex and Lex, chemokine receptors, Betaig-H3 and uPAR might be of clinical importance. ICAM1 was found to be less relevant in tumour cell adhesion in the context of peritoneal metastases. Based on currently available data, sLea and MUC16 are the most promising prognostic biomarkers for colorectal peritoneal metastases that may help improve patient selection. Different adhesion molecules appear expressed in haematogenous and transcoelomic spread, indicating two different attachment processes. However, our extensive assessment of available literature reveals that knowledge on metastasis-specific genes and their possible candidates is far from complete.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third most common cancer worldwide [1]. Approximately half of CRC patients develop distant metastasis, mainly through haematogenous dissemination to the liver [2, 3]. 10–25 % of CRC patients eventually develop peritoneal metastases (PM) [3, 4] and in up to 25 % of these patients the peritoneum is the only site of metastasis [4, 5]. Typically, untreated PM are associated with poor survival rates, even when treated with modern systemic chemotherapy [6–8].
Macroscopic complete cytoreductive surgery (CRS) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) is the preferred therapeutic strategy for patients with isolated PM [9, 10], resulting in a 5 year survival rate equal to that of patients undergoing resection for colorectal liver metastases (35–45 %) [11, 12] and a median survival of 33 months [6, 13, 14].
Despite the success of CRS and HIPEC, this treatment has morbidity and mortality rates of 15–34 and 5 % respectively [5, 6, 11, 15]. Therefore, selection of those patients that will benefit most from this treatment is of utmost importance. Other challenges in this field are earlier diagnosis and a more personalised approach, indicating that the choice of treatment should depend on a cancer’s specific biology instead of a ‘one size fits all’ approach [16]. Based on the hypothesis that the clinical behaviour of PM in CRC is dictated by biological mechanisms, read-outs of biological information (i.e., biomarkers) are very promising aids in addressing these clinical needs.
More specifically, understanding molecular mechanisms entails knowledge on molecules contributing to peritoneal dissemination. Peritoneal dissemination is considered to be a multistep process in which tumour cells must detach from their primary tumour, gain motility and evade anoikis. Once a viable, free cancer cell is present in the peritoneal cavity, adherence to the peritoneal surface is required in order to ultimately invade the peritoneum, proliferate and form PM [16].
Accordingly, the presence of free-floating cancer cells in the peritoneal cavity is known to increase the risk of peritoneal dissemination [9, 17–20]. Hence, exfoliation of cancer cells into the peritoneal cavity might lead to PM formation in patients presenting with CRC growing through the serosa (T4 stage) [9, 21, 22]. Also patients undergoing abdominal surgery have an increased risk of PM formation, possibly through the combination of surgery-induced tumour spill and upregulation of adhesion molecules due to post-operative inflammation [9, 20, 23]. Thus, in several groups of patients, tumour cell adhesion to the peritoneum appears to be pivotal in peritoneal dissemination. Molecules responsible for adhesion might therefore be promising biomarkers that can be used in diagnosis, prognosis and therapy of PM. Considering tumour cell adhesion as a key step in the formation of PM [16, 24], we aimed to provide an overview of the functional importance of several attachment markers and to subsequently evaluate their roles in diagnosis, prognosis and therapy.
Methods
Literature search
A systematic literature search was conducted using the PubMed database of the U.S. National library of Medicine (medline and pre-medline). Table 1 shows the breakdown of search terms and Boolean combinations.
Inclusion- and exclusion criteria
All full-text papers, in English, published between January 1995 and January 2013 were considered in order to identify as many important adhesion molecules as possible. For this purpose, in vitro, ex vivo and in vivo studies on PM from colorectal, ovarian, gastric and pancreatic cancer as well as pseudomyxoma peritonei (PMP) were assessed. These types of cancer all disseminate to the peritoneum and can be treated with CRS and HIPEC. Literature on PM from CRC is scarce. As such, literature on other malignancies disseminating to the peritoneum may contain important information. Irrespective of the specific epithelial malignancy, cancer cells disseminate to the peritoneum theoretically following the same stepwise process [16]. Although the first steps, i.e. detachment from the primary tumour, gaining motility and evading anoikis, might differ between these cancers in respect to several molecules, cancer cells of these types of cancer have to attach to the peritoneal surface to form a peritoneal deposit [16]. Accordingly, the same molecular mechanisms might be important in these cancers and the same interventions might be useful in preventing peritoneal dissemination. No reviews and case-reports were included. Other papers were incorporated by manually cross-referencing from publications retrieved in the initial search.
An additional review was conducted when deemed necessary. When studies overlapped or were duplicated, the articles with the most complete data on tumour cell adhesion to the peritoneum were retained. Figure 1 depicts the literature search and the selection process.
PRISMA flow chart for inclusion of the studies [152]
Results
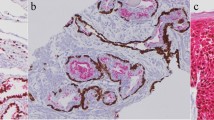
The key mechanism in PM formation is adherence of malignant cells to the peritoneal surface. Figure 2 illustrates the process of peritoneal dissemination. Figure 3 depicts the main interactions responsible for tumour cell adhesion to the peritoneum. Below, the functional and clinical importance of the adhesion molecules will be discussed.
Adhesive interactions mediating tumour cell adhesion to the peritoneum. a Especially α2β1 expressed on colorectal [46], ovarian [26, 27, 33–42, 149], gastric [28, 31, 43–45, 150] and pancreatic [30, 47, 151] cancer cells; b especially CD44 and CD44 s expressed on colorectal [64], ovarian [27, 34, 65–67, 70, 76, 77, 90], gastric [28, 29, 78] and pancreatic [30] cancer cells; c expressed on colorectal, ovarian and pancreatic cancer cells [95]; d expressed on ovarian cancer cells [98–100]; e expressed on ovarian [40, 93, 122, 123] and pancreatic [122] cancer cells; f expressed on ovarian cancer cells [141]; g expressed on ovarian cancer cells [55]; h expressed on ovarian cancer cells [93, 105]
Integrins and integrin ligands
Integrins
Integrins belong to the superfamily of cell adhesion receptors. This family consists of 24 members, each of which is a heterodimer composed of α and β subunits [25]. In particular, integrin β1 [26–30] and integrin α2 [26–29, 31, 32] chains were shown to be upregulated in cancer cells with high peritoneal seeding potential. Multiple in vitro and ex vivo blocking experiments with ovarian [26, 27, 33–42], gastric [28, 31, 43–45], colon [46] and pancreatic [30, 47] cancer cells further endorse the roles of integrin α2β1 in cancer cell attachment to the peritoneum. Besides mediating adhesion of free-floating tumour cells, integrin α2β1 might also be important in the adhesion of ovarian cancer cell aggregates (i.e. spheroids) to the peritoneum, in this way promoting PM formation [40, 41].
The above-mentioned studies not only support the role of integrin α2β1 in tumour cell attachment to the peritoneum, but also suggest that integrin blocking might be a useful strategy for prevention and treatment of PM. In vivo studies suggested a role for antibodies against integrin β1 chains in prevention of colorectal [46], gastric [28, 45] and pancreatic [47] tumour cell adhesion to (traumatised) peritoneum. Furthermore, the NF-κB inhibitor dehydroxymethylepoxyquinomicin (DHMEQ) reduced expression of integrin β1 and α2 chains and was effective, both in vitro and in vivo, in preventing PM formation from gastric cancer [48]. For this purpose, other compounds that diminish integrin β1 chain expression, such as phospholipids [49], endostatin and simvastatin [42, 50] might be effective as well and are interesting to pursue further.
Although some studies describe a less prominent role for integrin β1 chains in PM formation [38, 51, 52], the majority of published literature showed the opposite. Literature on several other subunits only concerns their roles in vitro [34, 39–41, 47, 53, 54]. Their roles in vivo, therefore, remain unclear.
Integrin ligands
Multiple in vitro studies have indicated that the main mesothelial ligands participating in the interaction with integrins are the extracellular matrix (ECM) components vitronectin [39, 47, 52, 54, 55], fibronectin [27, 30, 34, 40, 41, 45], laminin [27, 30, 34, 40, 41, 44, 45, 56, 57] and collagen I and IV [27, 30, 34, 40, 41, 45]. Adherence of tumour cells to ECM components occurs in several ways. First, free tumour cells might enter the submesothelial compartment at places of peritoneal discontinuity, for example places that consist of milky spots [58] or places where discontinuity is induced by surgery [23, 46, 59]. Secondly, tumour cells can induce apoptosis of mesothelial cells [59]. Also, the ECM might be exposed after inflammatory mediators induce contraction of mesothelial cells and disruption of intercellular junctions [59]. These ECM components might serve as treatment targets as well, since blocking them with antibodies and peptide sequences can reduce tumour cell adhesion. For example, the fibronectin amino acid sequence RGDS and the laminin sequence YIGSR inhibited in vitro and in vivo peritoneal dissemination from gastric and ovarian cancer [26, 57, 60]. Another possible therapeutic option in gastric cancer is coupling of adriamycin to the laminin-5 peptide sequence SWKLPPS, as it increased its in vitro anticancer activity [61].
Proteoglycans
CD44
The CD44 molecule is a cell-surface proteoglycan participating in cell–cell interaction, cell adhesion and cell migration [62]. In particular, CD44 isoforms originating from alternative splicing are thought to be important in tumour metastasis. The molecule is expressed on mesothelial cells and several types of cancer cells (Fig. 3). Its overexpression in gastric [29], ovarian [27] and in pancreatic [30, 63] cancer with high peritoneal seeding potential indicates a putative role for CD44 in PM formation. In vitro and ex vivo blocking experiments in several types of cancer illustrated the role of CD44 as adhesion molecule in PM formation [44, 64–70] and particularly indicated a role for the CD44 s splice variant [28, 30, 70]. Concluding from in vitro, ex vivo and in vivo studies, this molecule predominantly acts by binding to the ECM proteoglycan hyaluronan [28, 64, 65, 67, 71].
CD44 and CD44 s mediated adhesion to hyaluronan might partially be responsible for augmented cancer cell adhesion during post-operative inflammatory conditions. During this response, reactive oxygen species (ROS) [72, 73] and cytokines, for example TGF-β1, IL-1b and TNF-α [72, 74], are generated that upregulate CD44 expression and may also be responsible for the expression of other adhesion molecules [69].
Due to its suggested function in PM, CD44 s and its ligands hyaluronan are theoretically attractive therapeutic targets. In vivo blocking of CD44 s prevented PM in ovarian, gastric and pancreatic cancer [28, 30, 60, 68]. Other molecules contributing to CD44 mediated cell adhesion might also serve as therapeutic targets, e.g. urokinase plasminogen activator (uPA), multidrug resistance 1 polypeptide (MDR1) and multidrug resistance protein 2 (MRP2) [75]. A third option is inhibiting CD44 glycosylation, because this process is possibly involved in CD44 mediated adhesion [66]. The CD44 s splice variant has, despite its role in PM, an uncertain prognostic and diagnostic value [76–80].
Although—theoretically—blocking the CD44 ligand hyaluronan might prevent peritoneal dissemination, its therapeutic value is controversial: both tumour promoting and tumour repressing effects were reported after blocking CD44 intraperitoneally with hyaluronan [81–83]. Intraperitoneal application of the hyaluronan-degrading enzyme hyaluronidase, however, does yield promising in vitro results [28, 34, 64, 65]. Hyaluronidase possibly acts by degradation of mesothelial-associated hyaluronan, thereby preventing hyaluronan from interacting with CD44 on tumour cells. Another strategy is improving chemotherapeutic agent delivery to malignant cells by coupling them to hyaluronan. In vivo, promising results were seen for intraperitoneal use of hyaluronan bound cisplatin [84] and hyaluronate (ONCOFID-P) [85] bound to paclitaxel in ovarian cancer and for hyaluronan (ONCOFID-S) bound to camptothecin (SN38) in CRC [86]. Lastly, in vitro and in vivo experiments indicated a possible role for adhesion barriers, such as seprafilm and hyalurobarrier, in inhibiting peritoneal dissemination [82, 87–89].
Other proteoglycans
Several other proteoglycans have been described in tumour cell adhesion to the peritoneum. The proteoglycans syndecan-1, syndecan-2, syndecan-4, glypican-1 and glypican-3 were upregulated in gastric cancer with high in vitro and in vivo peritoneal seeding potential [90], suggesting a role for these molecules in peritoneal dissemination. Considering that several compounds blocking heparan sulfate and chondroitin sulfate proteoglycans, such as heparin, heparin sulfate, dermatan sulfate, chondroitin glycosaminoglycans, heparitinase, chondroitinase ABC, or methylumbelliferyl xyloside, inhibit ovarian [27, 28, 53, 90] and colorectal [91] cancer cell adhesion to ECM components, blocking these proteoglycans could be a promising therapeutic option.
Immunoglobulin superfamily
The immunoglobulin superfamily is a large group of cell adhesion proteins, which include intercellular adhesion molecule 1 (ICAM 1), vascular cell adhesion molecule 1 (VCAM 1) and L1 cell adhesion molecule (L1CAM) [2, 92].
ICAM1
ICAM1 is a cell surface molecule typically expressed on endothelial cells, cells of the immune system, cancer cells [42, 69, 72, 74, 93, 94] and mesothelial cells [69, 72–74, 93, 94]. Ziprin et al. [95] demonstrated in vitro tumour cell adhesion to the peritoneum to be mediated by the interaction between mesothelial ICAM1 and CD43 (sialophorin) on colorectal, ovarian and pancreatic cancer cells. This interaction might be important under postoperative inflammatory conditions, as the inflammatory mediators TNFα [69, 72, 74, 94], IL-1α [72], IL-1β [72], IL-6 [69] and ROS [73] enhanced ICAM1 expression and stimulated PM formation. Thus, theoretically, anti-ICAM1 antibodies [42, 69] or ICAM1 downregulation with heparin [94] and simvastatin treatment [42] may be used in prevention of PM under inflammatory conditions. However, several in vitro studies on the role of ICAM1 as an adhesion molecule in PM did not show reproducible findings [42, 69, 73, 94]. Surprisingly, an in vivo study in gastric cancer even indicated that ICAM1 possibly inhibits PM formation due to ICAM1/LFA1 mediated mononuclear cell recruitment [96]. These contradictory findings make ICAM1 a dubious therapeutic target.
VCAM1
The membrane protein VCAM1 mediates leukocyte-endothelial cell adhesion and signal transduction [97]. The mesothelial VCAM1 is possibly responsible for tumour cell adhesion by interacting with integrin α1β1 and α4β7 on tumour cells [93]. Enhanced VCAM1 expression induced by TNF-α, ILβ [72, 74] and ROS [73] might contribute to the increased risk of PM formation after surgery. Accordingly, downregulating this molecule with anti-VCAM1 antibodies [42, 71] or simvastatin [42] might prevent peritoneal dissemination.
L1CAM
L1CAM is described in various processes contributing to tumour progression, such as differentiation, proliferation, migration, invasion and tumour cell adhesion [98]. Its upregulation on ovarian cancer cells with high peritoneal seeding potential indicates a role for L1CAM in PM formation. In this process, as suggested by in vitro and in vivo ovarian cancer experiments, it probably mediates adhesion to the peritoneum by interacting with mesothelial neuropilin 1 (NRP1) [99]. Although L1CAM has not yet been proven to be valuable in the prognostic and diagnostic field [100], several therapeutic strategies targeting this molecule might be promising. One option might be antibody treatment, which reduced in vivo PM formation from ovarian cancer without producing side effects [98]. Another in vivo ovarian cancer study indicated possible therapeutic relevance for radioimmunotherapy combining anti-L1CAM antibodies (chCE7 and L1-11A) with 67Cu-radiotherapy [101].
Blood group antigen proteins
Several blood group antigens and related structures are expressed on tumour cells [28, 30, 102–104], including sialyl Lewis a (sLea, a blood group antigen), Lewis x and sialyl Lewis x (Lex and sLex, two blood group antigen related structures). However, only Lex [93, 105] and sLex [28, 30, 33, 106] appear to mediate tumour cell adhesion by interacting with mesothelial E-selectin [106]. Although in vitro and in vivo antibody experiments made the contribution of sLea unlikely [28, 30, 33, 102], in vivo PM formation from pancreatic cancer was inhibited after decreasing sLex and sLea biosynthesis by blocking fucosyltransferase 3 (FUT3) [107].
Despite its debatable role in tumour cell adhesion to the peritoneum, sLea detection using immunohistochemistry [104], immunocytology [103] or immunoassays in serum [108] correlated to the presence of PM, peritoneal recurrence [109, 110] and poor prognosis [103, 108–112]. In the diagnostic and prognostic field, especially serum and peritoneal lavage levels of CA19-9, a monoclonal antibody against sLea, were shown to be predictive. However, due to its low sensitivity and contradictory results in patients with gastric cancer, CRC and PMP [80, 103, 104, 108, 109, 111–120], CA19-9 is not yet qualified for clinical use as a single marker. Nevertheless, CA19-9 levels are possibly valuable in combination with other markers, for example CEA [118–120].
Mucins
Members of the mucin family are either present as secreted or as transmembrane proteins. Both forms are believed to be involved in inflammation and cancer [121]. When it comes to peritoneal spread, Mucin 16 (MUC16) is considered the most important member of this family. In vitro and in vivo studies suggested that cancer cell adhesion to the peritoneum partly relies on the interaction between MUC16 on ovarian cancer cells and mesothelin on mesothelial cells [122–126]. This interaction is probably mediated by the N-linked oligosaccharides of MUC16. Theoretically, blocking these oligosaccharides with lectins is an attractive therapeutic option [123]. In diagnosing PM, preoperative MUC16 serum levels in gastric cancer patients showed sensitivities ranging from 38.6 to 55 % and specificities between 93.9 and 100 % [113–115, 127, 128]. However, the prognostic value of MUC16 remains inconclusive [80, 127–129].
MUC1 is another mucin described in PM and is expressed on cancer cells [130–133]. It is questionable as to whether this mucin has a role in the attachment phase, since it does not bind mesothelin [122]. Accordingly, the role of MUC1 in clinical settings is so far not convincing [133, 134].
Epithelial cell adhesion molecule (EPCAM)
EpCAM is a homotypic calcium independent cell adhesion molecule not belonging to one of the previously mentioned groups of molecules [135]. Its expression on cancer cells [98] and its upregulation in PM from gastric cancer [136] suggest a function for this molecule in PM. Its role as adhesion molecule in PM, however, was not confirmed by in vivo antibody experiments in ovarian cancer [98].
In contrast, studies on the therapeutic value of EpCAM were promising, indicating that this molecule might promote peritoneal dissemination through other functions. This is illustrated by treatment with the bispecific antibody anti-EpCAM × anti-CD3 that eradicated PM from ovarian cancer in mice by reactivating tumour-resident T-cells [137]. The bispecific (anti-EpCAM x anti-CD3) trifunctional antibody Catumaxomab was investigated as monotherapy in a phase I/II study, in which this compound was shown to be relatively safe and possibly effective in gastric, colorectal and pancreatic cancer [138]. Concerning its possible diagnostic and prognostic value, data on EpCAM is inconsistent [103, 139].
Other molecules of interest
Several less frequently studied molecules possibly contribute to tumour cell adhesion as well. These are chemokine receptors, transforming growth factor beta induced gene-h3 (beta ig-h3) and urokinase receptor (uPAR). Although literature on the molecules described in this section suggest that they contribute to cancer cell adhesion to the peritoneum, further research should confirm this assumption.
The chemokine (C-X3-C motif) receptor 1 (CX3CR1) is expressed by ovarian cancer cells and was shown to mediate in vitro tumour cell adhesion to mesothelial cells by interacting with mesothelial chemokine (C-X3-C motif) ligand 1 (CX3CL1) [140]. Expression of another chemokine, chemokine (C-X-C) motif receptor 4 (CXCR4), is expressed on both mesothelial and cancer cells and correlates to worse survival rates in ovarian cancer patients. In vitro and in vivo blocking of CXCR4 with its antagonist ADM3100 was thereby shown to inhibit PM formation [141].
uPAR might also be relevant in PM formation and is detected at the interaction sites of ovarian carcinoma cells and mesothelial cells. In vitro experiments indicated that uPAR mediates tumour cell adhesion by interacting with mesothelial vitronectin [55].
Lastly, beta ig-h3 is an adhesion molecule expressed on mesothelial cells. Upregulation is associated with increased in vitro gastric cancer cell adhesion and the presence of PM [142], suggesting a role for this molecule in PM. Furthermore, in an in vitro ovarian cancer model, peritoneal cells—but not tumour cells—showed high beta ig-h3 levels. This molecule thereby significantly increased ovarian cancer cell adhesion to peritoneal cells, which could be blocked with a beta ig-h3 neutralising antibody [143].
Discussion
The present study was designed to identify molecules from literature that mediate tumour cell adhesion to the peritoneum and to evaluate their roles in diagnosis, prognosis and therapy of PM. Targeting adhesion molecules may not only prevent tumour cell adhesion and eventually tumour outgrowth in patients at high risk for peritoneal dissemination but the expression of adhesion molecules on tumour cells also allows us to use therapies targeting adhesion molecules in existing peritoneal carcinomatosis (Table 2; Fig. 4). Hence, advancing studies on the therapeutic and diagnostic value of adhesion molecules seems a very promising and rational way for optimising and personalising treatment of patients presenting with peritoneally metastasised CRC.
Most promising therapeutic options in prevention (left) and treatment (right) of peritoneal dissemination: 1 anti-integrin α2β1 antibodies; 2 peptide sequences; 3 anti-CD44 antibodies; 4 hyaluronan bound to cytostatic agents; 5 catumaxomab, a trifunctional antibody with binding sites for EpCAM, T-cells and accessory cells. (Color figure online)
In PM formation, the roles of CD44 s, integrin α2β1 and MUC16 appeared to be well investigated. Interestingly, integrin α2β1 is not the typical integrin that binds to ECM components. There might be several explanations for this discrepancy. First, according to the available literature tumour cells show upregulation of mainly the α2β1 subunits, meaning that the overall expression profile of integrin subunits might be different from the profile expressed by non-cancer cells. Consequently, interactions observed between tumour cells and mesothelial cells might differ as well. Secondly, as described in the result sections, literature on several other subunits only concerns their roles in vitro. Their roles in vivo, therefore, remain unclear. Due to their in vitro and ex vivo adhesive functions, L1CAM, proteoglycans, betaig-H3 and uPAR might contribute to peritoneal dissemination as well. However, their exact functions and clinical possibilities have to be elucidated. Accordingly, in vitro, ex vivo and in vivo antibody experiments should be developed to assess their adhesive potential. Furthermore, while two systematic reviews support our findings on most adhesion molecules [16, 59], most literature regarding the involvement of adhesion molecules in PM yields contradictory findings. This may be related to heterogeneity of published methods and varying sample sizes. In diagnosis and prognosis of PM, detection of MUC16 and blood group antigens might be useful. Prior to clinical implementation, however, extensive validation of these molecules is necessary. Validation in well-defined patient cohorts is also required for EpCAM, integrin α2β1 and CD44, molecules that have emerged as possibly useful therapeutic targets (Table 2; Fig. 4). Remarkably, while EpCAM showed therapeutic significance in ex vivo and in vivo experiments, its role in in vitro adhesion to the peritoneum was not confirmed. This discrepancy might be attributable to the finding that EpCAM carries out multiple functions, including cell adhesion, cellular signaling, migration, proliferation and differentiation [135, 144–146]. As such, the combination of these mechanisms, as opposed to only a single function (i.e. adhesion), might be of greater importance in promoting PM.
The role of adhesion in haematogenous metastases has been described in several literature studies. Bird et al. (2006) [2] focused on the development of liver metastases from CRC. In both haematogenous spread and spread across the peritoneal cavity—i.e. transcoelomic spread, cancer cells first must detach from the primary tumour to enter the circulation or the peritoneal cavity respectively. Cancer cells, carried by the blood stream or floating in the peritoneal cavity must evade immune defences in order to reach their host organ. At the site of the host organ, adhesive interactions between the organ and cancer cells are required for the development of a metastasis [2, 16, 59]. To disseminate to the liver, tumour cells have to adhere to endothelial cells lining the hepatic sinusoids. Interactions between tumour cells and endothelial cells that are thought to be important for liver dissemination consist of CD44 binding to hyaluronan, the blood group antigens sLea and sLex binding to selectins and mucins binding to ECM molecules [2]. This review, however, did not identify blood group antigens and E-selectin to be important in peritoneal dissemination. Additionally, L1CAM, proteoglycans, betaig-H3 and uPAR might contribute to PM formation, although these molecules were not described in the formation of liver metastases. Thus, we propose that haematogenous and transcoelomic spread differ in respect to several adhesion molecules. So far, no literature has described the exact differences between the mechanisms resulting in liver metastases from CRC and PM from CRC. Difference in adhesion mechanisms can be assumed, since cancer cells have to attach to different kind of cells: to mesothelial cells in peritoneal dissemination and to endothelial cells in hepatic spread. These different cells may express different molecules, making different cell–cell interactions necessary for adhesion. Expression of molecules depends on signalling molecules present in the environment, and thus may differ between the peritoneal surface and the hepatic sinusoids. For example, one study showed insulin-like growth factor 1 (IGF-1) and hypoxia-inducible factor 1-alpha (HIF-1α) to be exclusively overexpressed in PM and not in liver metastases [147]. Difference in growth factors and angiogenic factors might induce different expression patterns in endothelial and mesothelial cells.
Several studies stress the importance of new molecular targets to improve therapy and selection of patients with PM of CRC [8, 13, 14]. The adhesion molecules EpCAM, α2β1 and CD44 s were seen to mediate tumour cell adhesion to the peritoneum and might be particularly useful in the prevention of minimal residual disease in high-risk patients, such as patients with T4 colon tumours [21, 22]. In addition, blocking tumour cell adhesion in the perioperative period may be effective in preventing peritoneal dissemination [23]. A preventive HIPEC procedure might possibly be of additional value in high stage CRC [13]. With respect to a more personalised approach, blocking specific interactions between the mesothelial lining and tumour cell could be of even greater benefit in patients at high risk of peritoneal tumour spread. After blocking interactions between the peritoneal surface and tumour cells, tumours cells may die because of anoikis [16]. Furthermore, most tumour cells circulating in the peritoneal cavity are rapidly removed by the immune system [23]. Accordingly, once adhesion to the mesothelial lining is blocked, the tumour cell may be removed by the body’s own defence mechanisms [23]. This is supported by the observation that the presence of free-floating tumour cells in the peritoneal cavity does not necessarily lead to PM [18, 19].
This extensive assessment of available literature reveals that knowledge on metastasis-specific genes and their possible clinical implications is far from complete. An ‘–omics’ approach, synchronously assessing multiple biomarkers, might help to identify more biomarker candidates since it enables discovery-based research. Ideally, the first step in identifying new biomarker candidates would be the use of mass spectrometry-based proteomics in ex vivo models. In this way, protein expression on both CRC cell lines and patient derived peritoneum can be assessed, enabling comparison of molecules expressed on cancer cells and mesothelial cells. Next, the same proteomic approach in adhesion assays should assess the specific molecules required for adhesion, a process that could be visualised using green fluorescent protein. The previously described steps should be repeated in an environment reminiscing a surgery-induced environment by addition of interleukins. In this way, several possible candidates can be identified that mediate tumour-mesothelial adhesion in both a surgical and non-surgical setting. These candidates should be further studied using antibody blocking in functional assays and animal models. Prior to clinical implication, potential diagnostic, prognostic and therapeutic value of the identified markers should be validated in well-defined patient cohorts. Further studies should reduce the risk of bias associated with evaluation of molecular markers, for example by minimising differences in sample handling. It is thereby important to increase the reproducibility of individual studies using a split-sample for independent validation [148]. Ultimately, increasing reproducibility of genome-wide studies and extensive validation of possible biomarkers could lead to major advances in our understanding of metastasis-specific genes and their clinical possibilities. For CRC patients with PM, the gained knowledge on the diagnostic and therapeutic options of biomarkers will potentially lead to earlier diagnosis and a more personalised, or even preventive, approach and ultimately to better outcomes.
Abbreviations
- CRC:
-
Colorectal carcinoma
- PM:
-
Peritoneal metastases
- PMP:
-
Pseudomyxoma peritonei
- ECM:
-
Extracellular matrix
- uPA:
-
Urokinase plasminogen activator
- MDR1:
-
Multidrug resistance 1 polypeptide
- MRP2:
-
Multidrug resistance protein 2
- ICAM1:
-
Intercellular adhesion molecule
- VCAM1:
-
Vascular cell adhesion molecule
- L1CAM:
-
L1 cell adhesion molecule
- NRP1:
-
Neuropilin 1
- sLea :
-
Sialyl Lewis a
- Lex :
-
Lewis x
- sLex :
-
Sialyl Lewis x
- MUC16:
-
Mucin 16
- MUC1:
-
Mucin 1
- EpCAM:
-
Epithelial cell adhesion molecule
- CXCR4:
-
Chemokine (C-X-C) motif receptor 4
- uPAR:
-
Urokinase receptor
- Beta ig-h3:
-
Beta induced gene-h3
- CX3CL1:
-
Chemokine (C-X3-C motif) ligand 1
- IGF-1:
-
Insulin-like growth factor 1
- HIF-1α:
-
Hypoxia-inducible factor 1-alpha
References
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55(2):74–108
Bird NC, Mangnall D, Majeed AW (2006) Biology of colorectal liver metastases: a review. J Surg Oncol 94(1):68–80
Koppe MJ, Boerman OC, Oyen WJ, Bleichrodt RP (2006) Peritoneal carcinomatosis of colorectal origin: incidence and current treatment strategies. Ann Surg 243(2):212–222
Jayne DG, Fook S, Loi C, Seow-Choen F (2002) Peritoneal carcinomatosis from colorectal cancer. Br J Surg 89(12):1545–1550
Maggiori L, Bretagnol F, Ferron M, Chevalier Y, Panis Y (2011) Laparoscopic colorectal anastomosis using the novel Chex((R)) circular stapler: a case-control study. Colorectal Dis 13(6):711–715
Cao Y, Tan A, Gao F, Liu L, Liao C, Mo Z (2009) A meta-analysis of randomized controlled trials comparing chemotherapy plus bevacizumab with chemotherapy alone in metastatic colorectal cancer. Int J Colorectal Dis 24(6):677–685
Klaver YL, Simkens LH, Lemmens VE, Koopman M, Teerenstra S, Bleichrodt RP, de Hingh IH, Punt CJ (2012) Outcomes of colorectal cancer patients with peritoneal carcinomatosis treated with chemotherapy with and without targeted therapy. Eur J Surg Oncol 38(7):617–623
Franko J, Shi Q, Goldman CD, Pockaj BA, Nelson GD, Goldberg RM, Pitot HC, Grothey A, Alberts SR, Sargent DJ (2012) Treatment of colorectal peritoneal carcinomatosis with systemic chemotherapy: a pooled analysis of north central cancer treatment group phase III trials N9741 and N9841. J Clin Oncol 30(3):263–267
Sugarbaker PH (1995) Patient selection and treatment of peritoneal carcinomatosis from colorectal and appendiceal cancer. World J Surg 19(2):235–240
Sugarbaker PH, Jablonski KA (1995) Prognostic features of 51 colorectal and 130 appendiceal cancer patients with peritoneal carcinomatosis treated by cytoreductive surgery and intraperitoneal chemotherapy. Ann Surg 221(2):124–132
Verwaal VJ, van Ruth S, de Bree E, van Sloothen GW, van Tinteren H, Boot H, Zoetmulder FA (2003) Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol 21(20):3737–3743
Verwaal VJ, Kusamura S, Baratti D, Deraco M (2008) The eligibility for local-regional treatment of peritoneal surface malignancy. J Surg Oncol 98(4):220–223
Elias D, Gilly F, Boutitie F, Quenet F, Bereder JM, Mansvelt B, Lorimier G, Dube P, Glehen O (2010) Peritoneal colorectal carcinomatosis treated with surgery and perioperative intraperitoneal chemotherapy: retrospective analysis of 523 patients from a multicentric French study. J Clin Oncol 28(1):63–68
Kuijpers AM, Mirck B, Aalbers AG, Nienhuijs SW, de Hingh IH, Wiezer MJ, van Ramshorst B, van Ginkel RJ, Havenga K, Bremers AJ, de Wilt JH, te Velde EA et al (2013) Cytoreduction and HIPEC in the Netherlands: nationwide long-term outcome following the Dutch protocol. Ann Surg Oncol 20(13):4224–4230
Verwaal VJ, Zoetmulder FA (2004) Follow-up of patients treated by cytoreduction and chemotherapy for peritoneal carcinomatosis of colorectal origin. Eur J Surg Oncol 30(3):280–285
de Cuba EM, Kwakman R, van Egmond M, Bosch LJ, Bonjer HJ, Meijer GA, te Velde EA (2012) Understanding molecular mechanisms in peritoneal dissemination of colorectal cancer: future possibilities for personalised treatment by use of biomarkers. Virchows Arch 461(3):231–243
Nakanishi H, Kodera Y, Yamamura Y, Ito S, Kato T, Ezaki T, Tatematsu M (2000) Rapid quantitative detection of carcinoembryonic antigen-expressing free tumor cells in the peritoneal cavity of gastric-cancer patients with real-time RT-PCR on the lightcycler. Int J Cancer 89(5):411–417
Kanellos I, Demetriades H, Zintzaras E, Mandrali A, Mantzoros I, Betsis D (2003) Incidence and prognostic value of positive peritoneal cytology in colorectal cancer. Dis Colon Rectum 46(4):535–539
Yamamoto S, Akasu T, Fujita S, Moriya Y (2003) Long-term prognostic value of conventional peritoneal cytology after curative resection for colorectal carcinoma. Jpn J Clin Oncol 33(1):33–37
Takebayashi K, Murata S, Yamamoto H, Ishida M, Yamaguchi T, Kojima M, Shimizu T, Shiomi H, Sonoda H, Naka S, Mekata E, Okabe H et al (2014) Surgery-induced peritoneal cancer cells in patients who have undergone curative gastrectomy for gastric cancer. Ann Surg Oncol 21(6):1991–1997
Shepherd NA, Baxter KJ, Love SB (1997) The prognostic importance of peritoneal involvement in colonic cancer: a prospective evaluation. Gastroenterology 112(4):1096–1102
Hompes D, Tiek J, Wolthuis A, Fieuws S, Penninckx F, Van CE, D’Hoore A (2012) HIPEC in T4a colon cancer: a defendable treatment to improve oncologic outcome. Ann Oncol 23(12):3123–3129
van der Bij GJ, Oosterling SJ, Beelen RH, Meijer S, Coffey JC, van Egmond M (2009) The perioperative period is an underutilized window of therapeutic opportunity in patients with colorectal cancer. Ann Surg 249(5):727–734
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Takada Y, Ye X, Simon S (2007) The integrins. Genome Biol 8(5):215
Strobel T, Cannistra SA (1999) Beta1-integrins partly mediate binding of ovarian cancer cells to peritoneal mesothelium in vitro. Gynecol Oncol 73(3):362–367
Casey RC, Oegema TRJ, Skubitz KM, Pambuccian SE, Grindle SM, Skubitz APN (2003) Cell membrane glycosylation mediates the adhesion, migration, and invasion of ovarian carcinoma cells. Clin Exp Metastasis 20(2):143–152
Nakashio T, Narita T, Akiyama S, Kasai Y, Kondo K, Ito K, Takagi H, Kannagi R (1997) Adhesion molecules and TGF-beta1 are involved in the peritoneal dissemination of NUGC-4 human gastric cancer cells. Int J Cancer 70(5):612–618
Nishii T, Yashiro M, Shinto O, Sawada T, Ohira M, Hirakawa K (2009) Cancer stem cell-like SP cells have a high adhesion ability to the peritoneum in gastric carcinoma. Cancer Sci 100(8):1397–1402
Hosono J, Narita T, Kimura N, Sato M, Nakashio T, Kasai Y, Nonami T, Nakao A, Takagi H, Kannagi R (1998) Involvement of adhesion molecules in metastasis of SW1990, human pancreatic cancer cells. J Surg Oncol 67(2):77–84
Kawamura T, Endo Y, Yonemura Y, Nojima N, Fujita H, Fujimura T, Obata T, Yamaguchi T, Sasaki T (2001) Significance of integrin alpha2/beta1 in peritoneal dissemination of a human gastric cancer xenograft model. Int J Oncol 18(4):809–815
Sakakura C, Hagiwara A, Nakanishi M, Shimomura K, Takagi T, Yasuoka R, Fujita Y, Abe T, Ichikawa Y, Takahashi S, Ishikawa T, Nishizuka I et al (2002) Differential gene expression profiles of gastric cancer cells established from primary tumour and malignant ascites. Br J Cancer 87(10):1153–1161
Kishikawa T, Sakamoto M, Ino Y, Kubushiro K, Nozawa S, Hirohashi S (1995) Two distinct patterns of peritoneal involvement shown by in vitro and in vivo ovarian cancer dissemination models. Invasion Metastasis 15(1–2):11–21
Lessan K, Aguiar DJ, Oegema T, Siebenson L, Skubitz AP (1999) CD44 and beta1 integrin mediate ovarian carcinoma cell adhesion to peritoneal mesothelial cells. Am J Pathol 154(5):1525–1537
Moser TL, Pizzo SV, Bafetti LM, Fishman DA, Stack MS (1996) Evidence for preferential adhesion of ovarian epithelial carcinoma cells to type I collagen mediated by the alpha2beta1 integrin. Int J Cancer 67(5):695–701
Matsuoka T, Yashiro M, Nishimura S, Inoue T, Fujihara T, Sawada T, Kato Y, Seki S, Hirakawa YS, Chung K (2000) Increased expression of alpha2beta1-integrin in the peritoneal dissemination of human gastric carcinoma. Int J Mol Med 5(1):21–25
Fishman DA, Kearns A, Chilukuri K, Bafetti LM, O’Toole EA, Georgacopoulos J, Ravosa MJ, Stack MS (1998) Metastatic dissemination of human ovarian epithelial carcinoma is promoted by alpha2beta1-integrin-mediated interaction with type I collagen. Invasion Metastasis 18(1):15–26
Buczek-Thomas JA, Chen N, Hasan T (1998) Integrin-mediated adhesion and signalling in ovarian cancer cells. Cell Signal 10(1):55–63
Ahmed N, Riley C, Rice G, Quinn M (2005) Role of integrin receptors for fibronectin, collagen and laminin in the regulation of ovarian carcinoma functions in response to a matrix microenvironment. Clin Exp Metastasis 22(5):391–402
Burleson KM, Casey RC, Skubitz KM, Pambuccian SE, Oegema TRJ, Skubitz APN (2004) Ovarian carcinoma ascites spheroids adhere to extracellular matrix components and mesothelial cell monolayers. Gynecol Oncol 93(1):170–181
Casey RC, Burleson KM, Skubitz KM, Pambuccian SE, Oegema TRJ, Ruff LE, Skubitz AP (2001) Beta 1-integrins regulate the formation and adhesion of ovarian carcinoma multicellular spheroids. Am J Pathol 159(6):2071–2080
Wagner BJ, Lob S, Lindau D, Horzer H, Guckel B, Klein G, Glatzle J, Rammensee HG, Brucher BL, Konigsrainer A (2011) Simvastatin reduces tumor cell adhesion to human peritoneal mesothelial cells by decreased expression of VCAM-1 and beta1 integrin. Int J Oncol 39(6):1593–1600
Lin MT, Chang CC, Lin BR, Yang HY, Chu CY, Wu MH, Kuo ML (2007) Elevated expression of Cyr61 enhances peritoneal dissemination of gastric cancer cells through integrin alpha2beta1. J Biol Chem 282(47):34594–34604
Takatsuki H, Komatsu S, Sano R, Takada Y, Tsuji T (2004) Adhesion of gastric carcinoma cells to peritoneum mediated by alpha3beta1 integrin (VLA-3). Cancer Res 64(17):6065–6070
Nishimura S, Chung YS, Yashiro M, Inoue T, Sowa M (1996) Role of alpha 2 beta 1- and alpha 3 beta 1-integrin in the peritoneal implantation of scirrhous gastric carcinoma. Br J Cancer 74(9):1406–1412
Oosterling SJ, van der Bij GJ, Bogels M, ten Raa S, Post JA, Meijer GA, Beelen RHJ, van Egmond M (2008) Anti-beta1 integrin antibody reduces surgery-induced adhesion of colon carcinoma cells to traumatized peritoneal surfaces. Ann Surg 247(1):85–94
Sawai H, Okada Y, Funahashi H, Matsuo Y, Takahashi H, Takeyama H, Manabe T (2006) Interleukin-1alpha enhances the aggressive behavior of pancreatic cancer cells by regulating the alpha6beta1-integrin and urokinase plasminogen activator receptor expression. BMC Cell Biol 7:8
Mino K, Ozaki M, Nakanishi K, Haga S, Sato M, Kina M, Takahashi M, Takahashi N, Kataoka A, Yanagihara K, Ochiya T, Kamiyama T et al (2011) Inhibition of nuclear factor-kappaB suppresses peritoneal dissemination of gastric cancer by blocking cancer cell adhesion. Cancer Sci 102(5):1052–1058
Jansen M, Jansen PL, Otto J, Kirtil T, Neuss S, Treutner KH, Schumpelick V (2006) The inhibition of tumor cell adhesion on human mesothelial cells (HOMC) by phospholipids in vitro. Langenbecks Arch Surg 391(2):96–101
Yokoyama Y, Ramakrishnan S (2007) Binding of endostatin to human ovarian cancer cells inhibits cell attachment. Int J Cancer 121(11):2402–2409
Cannistra SA, Ottensmeier C, Niloff J, Orta B, DiCarlo J (1995) Expression and function of beta 1 and alpha v beta 3 integrins in ovarian cancer. Gynecol Oncol 58(2):216–225
Maubant S, Cruet-Hennequart S, Dutoit S, Denoux Y, Crouet H, Henry-Amar M, Gauduchon P (2005) Expression of alpha V-associated integrin beta subunits in epithelial ovarian cancer and its relation to prognosis in patients treated with platinum-based regimens. J Mol Histol 36(1–2):119–129
Kokenyesi R, Murray KP, Benshushan A, Huntley ED, Kao MS (2003) Invasion of interstitial matrix by a novel cell line from primary peritoneal carcinosarcoma, and by established ovarian carcinoma cell lines: role of cell-matrix adhesion molecules, proteinases, and E-cadherin expression. Gynecol Oncol 89(1):60–72
Fukuda K, Saikawa Y, Yagi H, Wada N, Takahashi T, Kitagawa Y (2012) Role of integrin alpha1 subunits in gastric cancer patients with peritoneal dissemination. Mol Med Rep 5(2):336–340
Heyman L, Kellouche S, Fernandes J, Dutoit S, Poulain L, Carreiras F (2008) Vitronectin and its receptors partly mediate adhesion of ovarian cancer cells to peritoneal mesothelium in vitro. Tumour Biol 29(4):231–244
Carreiras F, Lehmann M, Sichel F, Marvaldi J, Gauduchon P, le Talaer JY (1995) Implication of the alpha v beta 3 integrin in the adhesion of the ovarian-adenocarcinoma cell line IGROV1. Int J Cancer 63(4):530–536
Matsuoka T, Hirakawa K, Chung YS, Yashiro M, Nishimura S, Sawada T, Saiki I, Sowa M (1998) Adhesion polypeptides are useful for the prevention of peritoneal dissemination of gastric cancer. Clin Exp Metastasis 16(4):381–388
Liu J, Geng X, Li Y (2016) Milky spots: omental functional units and hotbeds for peritoneal cancer metastasis. Tumour Biol. Epub ahead of print
Ceelen WP, Bracke ME (2009) Peritoneal minimal residual disease in colorectal cancer: mechanisms, prevention, and treatment. Lancet Oncol 10(1):72–79
Hirabayashi Y, Yamaguchi K, Shiraishi N, Adachi Y, Saiki I, Kitano S (2004) Port-site metastasis after CO2 pneumoperitoneum: role of adhesion molecules and prevention with antiadhesion molecules. Surg Endosc 18(7):1113–1117
Akita N, Maruta F, Seymour LW, Kerr DJ, Parker AL, Asai T, Oku N, Nakayama J, Miyagawa S (2006) Identification of oligopeptides binding to peritoneal tumors of gastric cancer. Cancer Sci 97(10):1075–1081
Aruffo A, Stamenkovic I, Melnick M, Underhill CB, Seed B (1990) CD44 is the principal cell surface receptor for hyaluronate. Cell 61(7):1303–1313
Yeo TK, Nagy JA, Yeo KT, Dvorak HF, Toole BP (1996) Increased hyaluronan at sites of attachment to mesentery by CD44-positive mouse ovarian and breast tumor cells. Am J Pathol 148(6):1733–1740
Harada N, Mizoi T, Kinouchi M, Hoshi K, Ishii S, Shiiba K, Sasaki I, Matsuno S (2001) Introduction of antisense CD44S CDNA down-regulates expression of overall CD44 isoforms and inhibits tumor growth and metastasis in highly metastatic colon carcinoma cells. Int J Cancer 91(1):67–75
Gardner MJ, Catterall JB, Jones LM, Turner GA (1996) Human ovarian tumour cells can bind hyaluronic acid via membrane CD44: a possible step in peritoneal metastasis. Clin Exp Metastasis 14(4):325–334
Catterall JB, Jones LM, Turner GA (1999) Membrane protein glycosylation and CD44 content in the adhesion of human ovarian cancer cells to hyaluronan. Clin Exp Metastasis 17(7):583–591
Li CZ, Liu B, Wen ZQ, Li HY (2008) Inhibition of CD44 expression by small interfering RNA to suppress the growth and metastasis of ovarian cancer cells in vitro and in vivo. Folia Biol (Praha) 54(6):180–186
Strobel T, Swanson L, Cannistra SA (1997) In vivo inhibition of CD44 limits intra-abdominal spread of a human ovarian cancer xenograft in nude mice: a novel role for CD44 in the process of peritoneal implantation. Cancer Res 57(7):1228–1232
Ziprin P, Ridgway PF, Pfistermuller KLM, Peck DH, Darzi AW (2003) ICAM-1 mediated tumor-mesothelial cell adhesion is modulated by IL-6 and TNF-alpha: a potential mechanism by which surgical trauma increases peritoneal metastases. Cell Commun Adhes 10(3):141–154
Cannistra SA, DeFranzo B, Niloff J, Ottensmeir C (1995) Functional heterogeneity of CD44 molecules in ovarian cancer cell lines. Clin Cancer Res 1(3):333–342
Catterall JB, Gardner MJ, Jones LM, Turner GA (1997) Binding of ovarian cancer cells to immobilized hyaluronic acid. Glycoconj J 14(7):867–869
van Grevenstein WMU, Hofland LJ, Jeekel J, van Eijck CHJ (2006) The expression of adhesion molecules and the influence of inflammatory cytokines on the adhesion of human pancreatic carcinoma cells to mesothelial monolayers. Pancreas 32(4):396–402
ten Raa S, van Grevenstein HMU, ten Kate M, Mangundap KM, Hofland LJ, Jeekel H, Sluiter W, van Eijck CHJ (2007) The influence of reactive oxygen species on the adhesion of pancreatic carcinoma cells to the peritoneum. Cell Adhes Migr 1(2):77–83
Yu G, Tang B, Yu PW, Peng ZH, Qian F, Sun G (2010) Systemic and peritoneal inflammatory response after laparoscopic-assisted gastrectomy and the effect of inflammatory cytokines on adhesion of gastric cancer cells to peritoneal mesothelial cells. Surg Endosc 24(11):2860–2870
Chen H, Hao J, Wang L, Li Y (2009) Coexpression of invasive markers (uPA, CD44) and multiple drug-resistance proteins (MDR1, MRP2) is correlated with epithelial ovarian cancer progression. Br J Cancer 101(3):432–440
Berner HS, Davidson B, Berner A, Risberg B, Kristensen GB, Trope CG, Van de Putte G, Nesland JM (2000) Expression of CD44 in effusions of patients diagnosed with serous ovarian carcinoma—diagnostic and prognostic implications. Clin Exp Metastasis 18(2):197–202
Kayastha S, Freedman AN, Piver MS, Mukkamalla J, Romero-Guittierez M, Werness BA (1999) Expression of the hyaluronan receptor, CD44S, in epithelial ovarian cancer is an independent predictor of survival. Clin Cancer Res 5(5):1073–1076
Yamamichi K, Uehara Y, Kitamura N, Nakane Y, Hioki K (1998) Increased expression of CD44v6 mRNA significantly correlates with distant metastasis and poor prognosis in gastric cancer. Int J Cancer 79(3):256–262
Sillanpaa S, Anttila MA, Voutilainen K, Tammi RH, Tammi MI, Saarikoski SV, Kosma VM (2003) CD44 expression indicates favorable prognosis in epithelial ovarian cancer. Clin Cancer Res 9(14):5318–5324
Baratti D, Kusamura S, Nonaka D, Langer M, Andreola S, Favaro M, Gavazzi C, Laterza B, Deraco M (2008) Pseudomyxoma peritonei: clinical pathological and biological prognostic factors in patients treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC). Ann Surg Oncol 15(2):526–534
Yamaguchi K, Hirabayashi Y, Shiromizu A, Shiraishi N, Adachi Y, Kitano S (2001) Enhancement of port site metastasis by hyaluronic acid under CO2 pneumoperitoneum in a murine model. Surg Endosc 15(5):504–507
Tan B, Wang JH, Wu QD, Kirwan WO, Redmond HP (2001) Sodium hyaluronate enhances colorectal tumour cell metastatic potential in vitro and in vivo. Br J Surg 88(2):246–250
Jones LM, Gardner MJ, Catterall JB, Turner GA (1995) Hyaluronic acid secreted by mesothelial cells: a natural barrier to ovarian cancer cell adhesion. Clin Exp Metastasis 13(5):373–380
Li SD, Howell SB (2010) CD44-targeted microparticles for delivery of cisplatin to peritoneal metastases. Mol Pharm 7(1):280–290
Banzato A, Bobisse S, Rondina M, Renier D, Bettella F, Esposito G, Quintieri L, Melendez-Alafort L, Mazzi U, Zanovello P, Rosato A (2008) A paclitaxel-hyaluronan bioconjugate targeting ovarian cancer affords a potent in vivo therapeutic activity. Clin Cancer Res 14(11):3598–3606
Serafino A, Zonfrillo M, Andreola F, Psaila R, Mercuri L, Moroni N, Renier D, Campisi M, Secchieri C, Pierimarchi P (2011) CD44-targeting for antitumor drug delivery: a new SN-38-hyaluronan bioconjugate for locoregional treatment of peritoneal carcinomatosis. Curr Cancer Drug Targ 11(5):572–585
Hubbard SC, Burns JW (2002) Effects of a hyaluronan-based membrane (seprafilm) on intraperitoneally disseminated human colon cancer cell growth in a nude mouse model. Dis Colon Rectum 45(3):334–341
Pucciarelli S, Codello L, Rosato A, Del Bianco P, Vecchiato G, Lise M (2003) Effect of antiadhesive agents on peritoneal carcinomatosis in an experimental model. Br J Surg 90(1):66–71
Haverlag R, van Rossen ME, van den Tol MP, Bonthuis F, Marquet RL, Jeekel J (1999) Hyaluronate-based coating solution for prevention of surgical adhesions has no major effect on adhesion and growth of intraperitoneal tumour cells. Eur J Surg 165(8):791–795
Kokenyesi R (2001) Ovarian carcinoma cells synthesize both chondroitin sulfate and heparan sulfate cell surface proteoglycans that mediate cell adhesion to interstitial matrix. J Cell Biochem 83(2):259–270
Jacobi CA, Ordemann J, Bohm B, Zieren HU, Sabat R, Muller JM (1997) Inhibition of peritoneal tumor cell growth and implantation in laparoscopic surgery in a rat model. Am J Surg 174(3):359–363
Paschos KA, Canovas D, Bird NC (2009) The role of cell adhesion molecules in the progression of colorectal cancer and the development of liver metastasis. Cell Signal 21(5):665–674
Gardner MJ, Jones LM, Catterall JB, Turner GA (1995) Expression of cell adhesion molecules on ovarian tumour cell lines and mesothelial cells, in relation to ovarian cancer metastasis. Cancer Lett 91(2):229–234
Alkhamesi NA, Ziprin P, Pfistermuller K, Peck DH, Darzi AW (2005) ICAM-1 mediated peritoneal carcinomatosis, a target for therapeutic intervention. Clin Exp Metastasis 22(6):449–459
Ziprin P, Alkhamesi NA, Ridgway PF, Peck DH, Darzi AW (2004) Tumour-expressed CD43 (sialophorin) mediates tumour mesothelial cell adhesion. Biol Chem 385(8):755–761
Tanaka H, Yashiro M, Sunami T, Ohira M, Hirakawa Y (2002) Lipid-mediated gene transfection of intercellular adhesion molecule-1 suppresses the peritoneal metastasis of gastric carcinoma. Int J Mol Med 10(5):613–617
Jones EY, Harlos K, Bottomley MJ, Robinson RC, Driscoll PC, Edwards RM, Clements JM, Dudgeon TJ, Stuart DI (1995) Crystal structure of an integrin-binding fragment of vascular cell adhesion molecule-1 at 1.8 A resolution. Nature 373(6514):539–544
Arlt MJE, Novak-Hofer I, Gast D, Gschwend V, Moldenhauer G, Grunberg J, Honer M, Schubiger PA, Altevogt P, Kruger A (2006) Efficient inhibition of intra-peritoneal tumor growth and dissemination of human ovarian carcinoma cells in nude mice by anti-L1-cell adhesion molecule monoclonal antibody treatment. Cancer Res 66(2):936–943
Stoeck A, Schlich S, Issa Y, Gschwend V, Wenger T, Herr I, Marme A, Bourbie S, Altevogt P, Gutwein P (2006) L1 on ovarian carcinoma cells is a binding partner for neuropilin-1 on mesothelial cells. Cancer Lett 239(2):212–226
Kodera Y, Nakanishi H, Ito S, Misawa K, Ito Y, Nakayama G, Koike M, Fujiwara M, Yamamura Y, Nakao A (2009) Expression of L1 cell adhesion molecule is a significant prognostic factor in pT3-stage gastric cancer. Anticancer Res 29(10):4033–4039
Knogler K, Grunberg J, Zimmermann K, Cohrs S, Honer M, Ametamey S, Altevogt P, Fogel M, Schubiger PA, Novak-Hofer I (2007) Copper-67 radioimmunotherapy and growth inhibition by anti-L1-cell adhesion molecule monoclonal antibodies in a therapy model of ovarian cancer metastasis. Clin Cancer Res 13(2 Pt 1):603–611
Asao T, Nagamachi Y, Morinaga N, Shitara Y, Takenoshita S, Yazawa S (1995) Fucosyltransferase of the peritoneum contributed to the adhesion of cancer cells to the mesothelium. Cancer 75(6 Suppl):1539–1544
Schott A, Vogel I, Krueger U, Kalthoff H, Schreiber HW, Schmiegel W, Henne-Bruns D, Kremer B, Juhl H (1998) Isolated tumor cells are frequently detectable in the peritoneal cavity of gastric and colorectal cancer patients and serve as a new prognostic marker. Ann Surg 227(3):372–379
Ikeda Y, Mori M, Kamakura T, Saku M, Sugimachi K (1995) Immunohistochemical expression of sialyl Tn and sialyl Lewis(a) antigens in stromal tissue correlates with peritoneal dissemination in stage IV human gastric cancer. Eur J Surg Oncol 21(2):168–175
Kiguchi K, Iwamori M, Mochizuki Y, Kishikawa T, Tsukazaki K, Saga M, Amemiya A, Nozawa S (1998) Selection of human ovarian carcinoma cells with high dissemination potential by repeated passage of the cells in vivo into nude mice, and involvement of Le(x)-determinant in the dissemination potential. Jpn J Cancer Res 89(9):923–932
Gebauer F, Wicklein D, Stubke K, Nehmann N, Schmidt A, Salamon J, Peldschus K, Nentwich MF, Adam G, Tolstonog G, Bockhorn M, Izbicki JR et al (2013) Selectin binding is essential for peritoneal carcinomatosis in a xenograft model of human pancreatic adenocarcinoma in pfp–/rag2– mice. Gut 62(5):741–750
Aubert M, Panicot-Dubois L, Crotte C, Sbarra V, Lombardo D, Sadoulet MO, Mas E (2000) Peritoneal colonization by human pancreatic cancer cells is inhibited by antisense FUT3 sequence. Int J Cancer 88(4):558–565
Gaspar MJ, Arribas I, Coca MC, Diez-Alonso M (2001) Prognostic value of carcinoembryonic antigen, CA 19-9 and CA 72-4 in gastric carcinoma. Tumour Biol 22(5):318–322
Kochi M, Fujii M, Kanamori N, Kaiga T, Kawakami T, Aizaki K, Kasahara M, Mochizuki F, Kasakura Y, Yamagata M (2000) Evaluation of serum CEA and CA19-9 levels as prognostic factors in patients with gastric cancer. Gastric Cancer 3(4):177–186
Nakamori S, Furukawa H, Hiratsuka M, Iwanaga T, Imaoka S, Ishikawa O, Kabuto T, Sasaki Y, Kameyama M, Ishiguro S, Irimura T (1997) Expression of carbohydrate antigen sialyl Le(a): a new functional prognostic factor in gastric cancer. J Clin Oncol 15(2):816–825
Nakagoe T, Sawai T, Tsuji T, Jibiki MA, Nanashima A, Yamaguchi H, Yasutake T, Ayabe H, Arisawa K, Ishikawa H (2002) Difference in prognostic value between sialyl Lewis(a) and sialyl Lewis(x) antigen levels in the preoperative serum of gastric cancer patients. J Clin Gastroenterol 34(4):408–415
Ikeda Y, Oomori H, Koyanagi N, Mori M, Kamakura T, Minagawa S, Tateishi H, Sugimachi K (1995) Prognostic value of combination assays for CEA and CA 19-9 in gastric cancer. Oncology 52(6):483–486
Nakata B, Hirakawa YS, Chung K, Kato Y, Yamashita Y, Maeda K, Onoda O, Sawada T, Sowa M (1998) Serum CA 125 level as a predictor of peritoneal dissemination in patients with gastric carcinoma. Cancer 83(12):2488–2492
Hwang GI, Yoo CH, Sohn BH, Shin JH, Park YL, Kim HD, Kim YS, Han WK, Pae WK (2004) Predictive value of preoperative serum CEA, CA19-9 and CA125 levels for peritoneal metastasis in patients with gastric carcinoma. Cancer Res Treat 36(3):178–181
Yamamoto M, Baba H, Kakeji Y, Endo K, Ikeda Y, Toh Y, Kohnoe S, Okamura T, Maehara Y (2004) Prognostic significance of tumor markers in peritoneal lavage in advanced gastric cancer. Oncology 67(1):19–26
Yang SH, Lin JK, Lai CR, Chen CC, Li AF-Y, Liang WY, Jiang JK (2004) Risk factors for peritoneal dissemination of colorectal cancer. J Surg Oncol 87(4):167–173
Park IJ, Choi GS, Jun SH (2009) Prognostic value of serum tumor antigen CA19-9 after curative resection of colorectal cancer. Anticancer Res 29(10):4303–4308
Li Y, Yang Y, Lu M, Shen L (2011) Predictive value of serum CEA, CA19-9 and CA72.4 in early diagnosis of recurrence after radical resection of gastric cancer. Hepatogastroenterology 58(112):2166–2170
Takahashi Y, Takeuchi T, Sakamoto J, Touge T, Mai M, Ohkura H, Kodaira S, Okajima K, Nakazato H (2003) The usefulness of CEA and/or CA19-9 in monitoring for recurrence in gastric cancer patients: a prospective clinical study. Gastric Cancer 6(3):142–145
Marrelli D, Pinto E, De SA, Farnetani M, Garosi L, Roviello F (2001) Clinical utility of CEA, CA 19-9, and CA 72-4 in the follow-up of patients with resectable gastric cancer. Am J Surg 181(1):16–19
Kufe DW (2009) Mucins in cancer: function, prognosis and therapy. Nat Rev Cancer 9(12):874–885
Rump A, Morikawa Y, Tanaka M, Minami S, Umesaki N, Takeuchi M, Miyajima A (2004) Binding of ovarian cancer antigen CA125/MUC16 to mesothelin mediates cell adhesion. J Biol Chem 279(10):9190–9198
Gubbels JAA, Belisle J, Onda M, Rancourt C, Migneault M, Ho M, Bera TK, Connor J, Sathyanarayana BK, Lee B, Pastan I, Patankar MS (2006) Mesothelin-MUC16 binding is a high affinity, N-glycan dependent interaction that facilitates peritoneal metastasis of ovarian tumors. Mol Cancer 5(1):50
Scholler N, Garvik B, Hayden-Ledbetter M, Kline T, Urban N (2007) Development of a CA125-mesothelin cell adhesion assay as a screening tool for biologics discovery. Cancer Lett 247(1):130–136
Bergan L, Gross JA, Nevin B, Urban N, Scholler N (2007) Development and in vitro validation of anti-mesothelin biobodies that prevent CA125/mesothelin-dependent cell attachment. Cancer Lett 255(2):263–274
Theriault C, Pinard M, Comamala M, Migneault M, Beaudin J, Matte I, Boivin M, Piche A, Rancourt C (2011) MUC16 (CA125) regulates epithelial ovarian cancer cell growth, tumorigenesis and metastasis. Gynecol Oncol 121(3):434–443
Emoto S, Ishigami H, Yamashita H, Yamaguchi H, Kaisaki S, Kitayama J (2012) Clinical significance of CA125 and CA72-4 in gastric cancer with peritoneal dissemination. Gastric Cancer 15(2):154–161
Fujimura T, Kinami S, Ninomiya I, Kitagawa H, Fushida S, Nishimura G, Kayahara M, Shimizu K, Ohta T, Miwa K (2002) Diagnostic laparoscopy, serum CA125, and peritoneal metastasis in gastric cancer. Endoscopy 34(7):569–574
Yamamoto M, Baba H, Toh Y, Okamura T, Maehara Y (2007) Peritoneal lavage CEA/CA125 is a prognostic factor for gastric cancer patients. J Cancer Res Clin Oncol 133(7):471–476
Wang L, Ma J, Liu F, Yu Q, Chu G, Perkins AC, Li Y (2007) Expression of MUC1 in primary and metastatic human epithelial ovarian cancer and its therapeutic significance. Gynecol Oncol 105(3):695–702
van Elssen CH, Frings PW, Bot FJ, van de Vijver KK, Huls MB, Meek B, Hupperets P, Germeraad WT, Bos GM (2010) Expression of aberrantly glycosylated mucin-1 in ovarian cancer. Histopathology 57(4):597–606
Nakanishi H, Kodera Y, Yamamura Y, Kuzuya K, Nakanishi T, Ezaki T, Tatematsu M (1999) Molecular diagnostic detection of free cancer cells in the peritoneal cavity of patients with gastrointestinal and gynecologic malignancies. Cancer Chemother Pharmacol 43(Suppl):S32–S36
Wang L, Chen H, Pourgholami MH, Beretov J, Hao J, Chao H, Perkins AC, Kearsley JH, Li Y (2011) Anti-MUC1 monoclonal antibody (C595) and docetaxel markedly reduce tumor burden and ascites, and prolong survival in an in vivo ovarian cancer model. PLoS ONE 6(9):e24405
Oei ALM, Moreno M, Verheijen RHM, Sweep FCGJ, Thomas CMG, Massuger LFAG, von Mensdorff-Pouilly S (2008) Induction of IgG antibodies to MUC1 and survival in patients with epithelial ovarian cancer. Int J Cancer 123(8):1848–1853
Patriarca C, Macchi RM, Marschner AK, Mellstedt H (2012) Epithelial cell adhesion molecule expression (CD326) in cancer: a short review. Cancer Treat Rev 38(1):68–75
Imano M, Itoh T, Satou T, Yasuda A, Nishiki K, Kato H, Shiraishi O, Peng Y, Shinkai M, Tsubaki M, Yasuda T, Imamoto H et al (2012) High expression of epithelial cellular adhesion molecule in peritoneal metastasis of gastric cancer. Targ Oncol 8(4):231–235
Schlereth B, Fichtner I, Lorenczewski G, Kleindienst P, Brischwein K, da Silva A, Kufer P, Lutterbuese R, Junghahn I, Kasimir-Bauer S, Wimberger P, Kimmig R et al (2005) Eradication of tumors from a human colon cancer cell line and from ovarian cancer metastases in immunodeficient mice by a single-chain Ep-CAM-/CD3-bispecific antibody construct. Cancer Res 65(7):2882–2889
Strohlein MA, Lordick F, Ruttinger D, Grutzner KU, Schemanski OC, Jager M, Lindhofer H, Hennig M, Jauch KW, Peschel C, Heiss MM (2011) Immunotherapy of peritoneal carcinomatosis with the antibody catumaxomab in colon, gastric, or pancreatic cancer: an open-label, multicenter, phase I/II trial. Onkologie 34(3):101–108
Rossi Del Monte S, Ranieri D, Mazzetta F, Kazemi Nava A, Raffa S, Torrisi MR, Ziparo V (2012) Free peritoneal tumor cells detection in gastric and colorectal cancer patients. J Surg Oncol 106(1):17–23
Kim M, Rooper L, Xie J, Kajdacsy-Balla AA, Barbolina MV (2012) Fractalkine receptor CX(3)CR1 is expressed in epithelial ovarian carcinoma cells and required for motility and adhesion to peritoneal mesothelial cells. Mol Cancer Res 10(1):11–24
Kajiyama H, Shibata K, Terauchi M, Ino K, Nawa A, Kikkawa F (2008) Involvement of SDF-1alpha/CXCR4 axis in the enhanced peritoneal metastasis of epithelial ovarian carcinoma. Int J Cancer 122(1):91–99
Li Z, Miao Z, Jin G, Li X, Li H, Lv Z, Xu HM (2012) betaig-h3 supports gastric cancer cell adhesion, migration and proliferation in peritoneal carcinomatosis. Mol Med Rep 6(3):558–564
Ween MP, Lokman NA, Hoffmann P, Rodgers RJ, Ricciardelli C, Oehler MK (2011) Transforming growth factor-beta-induced protein secreted by peritoneal cancer cells increases the metastatic potential of ovarian cancer cells. Int J Cancer 128:1570–1584
Trzpis M, McLaughlin PM, de Leij LM, Harmsen MC (2007) Epithelial cell adhesion molecule: more than a carcinoma marker and adhesion molecule. Am J Pathol 171(2):386–395
Maetzel D, Denzel S, Mack B, Canis M, Went P, Benk M, Kieu C, Papior P, Baeuerle PA, Munz M, Gires O (2009) Nuclear signalling by tumour-associated antigen EpCAM. Nat Cell Biol 11(2):162–171
Gosens MJ, van Kempen LC, van de Velde CJ, van Krieken JH, Nagtegaal ID (2007) Loss of membranous Ep-CAM in budding colorectal carcinoma cells. Mod Pathol 20(2):221–232
Verghese S, Burness M, Xu H, Beresnev T, Pingpank J, Alexander HR (2007) Site-specific gene expression profiles and novel molecular prognositc factors in patients with lower gastrointestinal adenocarcinoma diffusely metastatic to liver or peritoneum. Ann Surg Oncol 14(12):3460–3471
Ransohoff DF (2004) Rules of evidence for cancer molecular-marker discovery and validation. Nat Rev Cancer 4(4):309–314
Davidson B, Goldberg I, Reich R, Tell L, Dong HP, Trope CG, Risberg B, Kopolovic J (2003) AlphaV- and beta1-integrin subunits are commonly expressed in malignant effusions from ovarian carcinoma patients. Gynecol Oncol 90(2):248–257
Nishimura S, Chung YS, Yashiro M, Inoue T, Sowa M (1996) CD44H plays an important role in peritoneal dissemination of scirrhous gastric cancer cells. Jpn J Cancer Res 87(12):1235–1244
Grzesiak JJ, Tran Cao HS, Burton DW, Kaushal S, Vargas F, Clopton P, Snyder CS, Deftos LJ, Hoffman RM, Bouvet M (2011) Knockdown of the beta(1) integrin subunit reduces primary tumor growth and inhibits pancreatic cancer metastasis. Int J Cancer 129(12):2905–2915
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(6): e1000097. doi:10.1371/journal.pmed1000097
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Sluiter, N., de Cuba, E., Kwakman, R. et al. Adhesion molecules in peritoneal dissemination: function, prognostic relevance and therapeutic options. Clin Exp Metastasis 33, 401–416 (2016). https://doi.org/10.1007/s10585-016-9791-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-016-9791-0