Abstract
Purpose
The purpose of the experiment was to compare the effects of nifekalant and amiodarone on the return of spontaneous circulation (ROSC), survival, as well as on the hemodynamic parameters in a swine model of prolonged ventricular fibrillation (VF).
Methods
After 8 min of untreated VF, bolus doses of epinephrine (adrenaline) and either nifekalant, or amiodarone, or saline (n = 10 per group), were administered after randomization. Cardiopulmonary resuscitation (CPR) was commenced immediately after drug administration and defibrillation was attempted 2 min later. CPR was resumed for another 2 min after each defibrillation attempt and the same dose of adrenaline was given every 4th minute during CPR.
Results
Forty-eight hour survival was significantly higher with nifekalant compared to amiodarone (p < 0.001) and saline (p = 0.02), (9/10 vs. 0/10 vs. 3/10, respectively). Systolic aortic pressure, diastolic aortic pressure and coronary perfusion pressure were significantly higher with nifekalant during CPR and immediate post-resuscitation period (p < 0.05). The animals in the amiodarone group had a slower heart rate at the 1st and 45th min post-ROSC (p < 0.001 and p = 0.006, respectively). The number of electric shocks required for terminating VF, time to ROSC and adrenaline dose were significantly higher with amiodarone compared to nifekalant (p < 0.001).
Conclusions
Nifekalant showed a more favorable hemodynamic profile and improved survival compared to amiodarone and saline in this swine model.
Similar content being viewed by others
Introduction
Amiodarone is the recommended anti-arrhythmic drug in the latest guidelines for Cardiopulmonary Resuscitation (CPR) from the European Resuscitation Council and the American Heart Association (AHA) [1, 2]. It may be considered for those who have shock-resistant ventricular tachycardia (VT)/ventricular fibrillation (VF) or VT/VF recurrence in out-of-hospital or in-hospital cardiac arrest [3]. The role of amiodarone in cardiac arrest is supported by two randomized clinical trials showing improved survival to hospital admission compared to placebo or lidocaine [4, 5]. However, there is no convincing evidence that routine use of amiodarone or other drugs during human CPR improves either survival to hospital discharge or neurological outcome [3].
Nifekalant, formerly known as MS-551 [6], is a relatively new anti-arrhythmic agent approved only in Japan for the treatment of life-threatening VF/VT. It is considered a pure class III anti-arrhythmic as it selectively inhibits potassium channels, especially the rapid component of the delayed rectifier potassium current (Ikr), resulting in prolongation of action potential and refractory period of the ventricular myocardium [7, 8]. Nifekalant has been shown to be superior to lidocaine in improving return of spontaneous circulation (ROSC) rates for patients with shock-refractory pulseless VT/VF [7, 9]. It is also reported that it may possess superior pharmacological properties as a rescue drug in life-threatening situations compared to amiodarone. Nifekalant has a rapid action and a shorter half-time, it is easily soluble, which makes it ideal for intravenous administration, it does not have a negative inotropic action and it improves defibrillation efficacy in cases of VT/VF. On the other hand, there is a greater risk of torsade de pointes (TdP) with nifekalant due to significant QT prolongation [10, 11]. In a recent study, the early administration of amiodarone in a porcine model of VF arrest was associated with adverse hemodynamics [12]. To our knowledge, the effect of nifekalant in the same setting has never been studied.
No randomized clinical trials comparing nifekalant and amiodarone are available. In a small non-randomized study, Amino et al. reported borderline superiority of amiodarone over nifekalant for ROSC and short-term survival but not for preservation of brain function in victims of out-of-hospital VF arrest [13]. Taking into consideration that nifekalant is a rapid acting medication with a potential to terminate VF/VT without a shock [7], we conducted an experimental randomized study of VF arrest in piglets to compare hemodynamic effects and outcome data of nifekalant, amiodarone and placebo given during CPR.
Methods
Animals
The protocol was approved by the Directorate of Veterinary Services of the Prefecture of Athens, Attica, Greece according to Greek legislation regarding ethical and experimental procedures (protocol number 2981/24-5-2012). Thirty female Landrace/Large-White piglets aged 10–15 weeks and weighting 19 ± 2 kg, all from the same breeder (Validakis, Athens, Greece) were studied. All animals were prepared in a standardized fashion in the research facility (ELPEN Experimental-Research Center, Pikermi, Greece) as previously described [14]. Initial sedation was achieved by intramuscular administration of ketamine hydrochloride (10 mg/kg), midazolam (0.5 mg/kg) and atropine (0.05 mg/kg). Anesthesia was induced by an intravenous (iv) propofol bolus (2 mg/kg) via the marginal auricular vein. The pigs were then intubated with a 4.5 mm cuffed endotracheal tube. Animals were mechanically ventilated using volume-controlled mode with a tidal volume of 15 ml/kg and a fractional inspired oxygen (FiO2) of 0.21. End-tidal CO2 (ETCO2) was monitored by in-line waveform capnography (Tonocap TC-200-22-01, Engstrom Division Instrumentarium Corp., Helsinki, Finland), and the respiratory frequency was adjusted to maintain ETCO2 between 35 and 40 mm Hg. A cis-atracurium bolus (0.15 mg/kg) was administered to ascertain animal-ventilator synchrony. Continuous infusion of propofol (≥150 μg/kg/min), was used for anesthesia and fentanyl (4 μg/kg) for analgesia. Cardiac rhythm and heart rate were monitored by electrocardiography (ECG), using leads I, II, III, aVR, aVL and aVF. Pulse oximetry (SpO2) was monitored continuously. The right carotid artery and right internal jugular vein were surgically prepared and catheterized under aseptic conditions. Aortic pressures were measured using a fluid-filled catheter (model 6523, USCI CR, Bart, Papapostolou, Athens, Greece) advanced via the right carotid artery into the thoracic aorta. Mean arterial pressure (MAP) was determined by electronic integration of the aortic blood pressure waveform. A catheter was inserted into the right atrium via the right jugular vein for continuous measurement of right atrial pressures. All catheters were calibrated (zeroed at right atrial level) before use and their correct position was verified by the presence of the typical pressure waveform.
Nifekalant
Nifekalant hydrochloride was purchased by Toronto Research Chemicals Inc. (TRC) in powder form. The appropriate dosage of the drug was diluted in water for injection just before each experiment. Nifekalant hydrochloride was stored at −16 °C in-between the experiments. Toronto Research Chemicals Inc. had absolutely no participation in any part of the experimental protocol or in the interpretation of results.
Experimental Protocol
After surgery the animals were allowed a 30-min stabilization period before baseline data were collected. VF was induced with a 9 V ordinary cadmium battery via a pacing wire forwarded into the right ventricle through the exposed right jugular vein, as previously described [14]. VF was confirmed by ECG and by a sudden drop in MAP to <10 mmHg. Mechanical ventilation and administration of anesthetic medication were discontinued simultaneously with the onset of VF and the animals were left untreated for 8 min. The rationale of using an 8 min non-flow period instead of the previously described 4 min period [15] was to test nifekalant and amiodarone in a different phase of cardiac arrest [16].
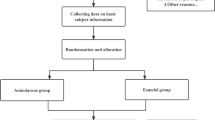
A bolus dose of epinephrine (adrenaline) (0.01 mg/kg) was then administered to all animals, and at the same time, the animals (n = 10 per group) were randomly treated with a bolus dose of nifekalant 2 mg/kg (nifekalant group or N group) or amiodarone (inj. sol. Angoron, Sanofi-Aventis) 5 mg/kg (amiodarone group or A group) or saline, as placebo (control group or C group). All drugs were injected via the marginal auricular vein, followed by a 10 ml saline flush. Randomization was achieved using computer-generated random numbers and sealed envelopes. The researchers were blinded to animal group allocation throughout the study. The drugs were prepared and infused with syringes covered with Sanitas® aluminum foil by an independent person who was not involved in any other part of the study.
CPR was commenced immediately after drug administration. Mechanical ventilation was resumed FiO2 = 0.21 and automatic continuous precordial compressions were initiated (LUCAS, Jolife, Lund, Sweden), at a rate of 100/min following the 2-min cycles [1].
After 2 min of CPR, defibrillation was attempted with a 4 J/kg monophasic shock. CPR was resumed for another 2 min after each defibrillation attempt. Further bolus doses of adrenaline (0.01 mg/kg) were administered every fourth min during CPR. Each experiment continued until ROSC or if asystole/pulseless electrical activity (PEA) occurred for >10 min after CPR initiation. ROSC was defined as the presence of a perfusing cardiac rhythm with MAP of at least 60 mmHg for a minimum of 5 min [14].
After ROSC, the animals were monitored closely while mechanically ventilated under general anesthesia for 6 h, at the pre-arrest ventilator settings. No other interventions (drugs, cardioversion or defibrillation attempts) were made after ROSC. After 6 h, all catheters were removed, the animals were allowed to recover from anesthesia, were extubated and transferred to their observation cages. They remained under observation for 48 h after ROSC and then euthanized with an iv propofol bolus (40 mg), followed by iv thiopental (2 g).
Experimental endpoints were ROSC and 48 h-survival.
Measurements
Hemodynamic variables (heart rate, aortic and right atrial pressures) and ECG were continuously recorded prior to- and during the arrest and the first 6 h post-ROSC. Coronary perfusion pressure (CPP) was calculated as the difference between aortic diastolic pressure and the simultaneously measured right atrial pressure, and was continuously recorded. Arterial blood gases (ABGs) were measured at baseline and 5 min after ROSC. The number of defibrillation attempts required to achieve ROSC, as well as the time to ROSC, was recorded in each experiment. The presence of post-resuscitation VT and TdP was also recorded. A neurological alertness score was performed at 48 h by a veterinarian blinded to intravenous treatment during resuscitation, as previously described [17]. Alertness was scored from 0 (coma) to 100 (fully alert).
Statistical Analysis
Data are expressed as mean ± SD for quantitative variables, and as frequency (%) for qualitative variables. The normality of the distributions was examined using the Kolmogorov-Smirnov test.
Quantitative and qualitative variables were compared between the two groups using independent samples t-test, or the Mann–Whitney test, and Fisher’s exact test respectively. The odds ratios (OR) with 95 % confidence interval for ROSC and survival between groups were calculated.
It was calculated that a sample size of ten evaluable experimental animals per group was required in order to have an 80 % probability of demonstrating a between treatment difference of 30 % in survival with a significance of <5 % (two tailed test).
Between group differences of all variables at each time point were analyzed with ANCOVA covariance model controlling for baseline difference using the value at each time point as dependant variable and baseline measurements as covariates.
All tests are two-sided, statistical significance was set at p < 0.05. All analyses were carried out using the statistical package SPSS vr 17.00 (Statistical Package for the Social Sciences, SPSS Inc., Chicago, Ill., USA).
Results
There were no significant differences in pre-arrest hemodynamics or ABGs between the three groups (Table 1).
There was no difference in systolic aortic pressure (SAP) between groups during the first 2 min of CPR but at the 3rd and the 4th min SAP was significantly higher in the nifekalant group [(N vs A (p < 0.001), N vs C (p = 0.002)]. There was no significant difference in SAP between nifekalant group and control group during the immediate post-resuscitation period. However, SAP was higher with nifekalant compared to amiodarone 1 min (p = 0.018), 15 min (p = 0.005) and 45 min (p < 0.001) after ROSC (Fig. 1a). Diastolic aortic pressure (DAP) was significantly higher in the nifekalant group at the 1st min [N vs A (p = 0.006), N vs C (p = 0.002)], the 3rd min [N vs A (p < 0.001), N vs C (p = 0.001)] and the 4th min of CPR [N vs A (p < 0.001), N vs C (p = 0.002)] and during the immediate post resuscitation period [1st min post-ROSC: N vs A (p = 0.012); 15th min post-ROSC: N vs A (p = 0.001), N vs C (p = 0.009); 45th min post-ROSC: N vs A (p < 0.001)], (Fig. 1b). In accordance with these findings there were significant differences in CPP during CPR between the three treatment groups in favor of nifekalant (Fig. 1c). The heart rate was significantly slower with amiodarone during the early post-resuscitation phase, 1 and 45 min after ROSC (p < 0.001 and p = 0.006, respectively).
a Systolic aortic pressure throughout the study time-points in nifekalant (Group N), amiodarone (Group A) and saline (Group C) treated animals. The values are presented as Adjusted Mean Difference (95%CI). *p < 0.001 vs Group A, 136 (72–199), p = 0.002 vs Group C, 121 (41–201); †p < 0.001 vs Group A, 118 (64–173), p = 0.002 vs Group C, 105 (35–174); ‡p = 0.018 vs Group A, 58 (9–107); §p = 0.005 vs Group A, 46 (13–80); ǁp < 0.001 vs Group A, 63 (33–93); #p = 0.027 vs Group A, 40 (4–76) b Diastolic aortic pressure throughout the study time-points in nifekalant (Group N), amiodarone (Group A) and saline (Group C) treated animals. The values are presented as Adjusted Mean Difference (95%CI). *p = 0.006 vs Group A, 23 (6–40), p = 0.002 vs Group C, 29 (10–48); †p < 0.001 vs Group A, 102 (64–140), p = 0.001 vs C, 70 (28–112); ‡p < 0.001 vs Group A, 101 (70–132), p = 0.002 vs Group C, 70 (35–104); §p = 0.012 vs Group A, 51 (10–92); ǁp = 0.001 vs Group A, 46 (20–73), p = 0.009 vs Group C, 41 (9–73); #p < 0.001 vs Group A, 70 (51–90); **p = 0.001 vs Group A, 45 (22–68) c Coronary perfusion pressure throughout the study time-points in nifekalant (Group N), amiodarone (Group A) and saline (Group C) treated animals. The values are presented as Adjusted Mean Difference (95%CI). *p = 0.03 vs Group A, 26 (2–49); †p < 0.001 vs Group A, 114 (69–160), p = 0.005 vs Group C, 59 (16–102); ‡p = 0.005 vs Group A, 55 (15–96); §p < 0.001 vs Group A, 100 (63–137), p = 0.002 vs Group C, 49 (15–84); ǁp = 0.003 vs Group A, 51 (18–83); #p = 0.039 vs Group A, 52 (2–101); **p = 0.018 vs Group A, 46 (7–84); ¥p < 0.001 vs Group A, 150 (68–231); ¶p = 0.001 vs Group A, 123 (66–180)
There was no significant difference in the rate of ROSC between nifekalant, amiodarone and control animals (10 out of 10 vs 6 out of 10 vs 8 out of 10 respectively, N vs A: p = 0.087, OR = 6.00, 95%CI 0.53–68.64; N vs C: p = 0.474, OR = 2.25, 95%CI 0.17–29.78). However, nifekalant was superior to amiodarone concerning the number of electric shocks required to terminate VF, time to ROSC (duration of CPR) and adrenaline dose (Table 2). Amiodarone showed arithmetical but not significant superiority in preventing VT occurrence during the early post-resuscitation period compared to nifekalant (0 out of 6 vs 5 out of 10 animals with VT after ROSC respectively, p = 0.093, OR = 5.00, 95%CI 0.52–69.75), however VT run in nifekalant animals was self-limiting so it did not have an impact on 48 h survival.
The 48 h survival rates were significantly higher with nifekalant compared to amiodarone and control (9 out 10 vs 0 out of 10 vs 3 out of 10 respectively, N vs A: p < 0.001, OR = 71.00, 95%CI 4.36–800.42; N vs C: p = 0.02, OR = 21.00, 95%CI 1.80–248.103), while there was no difference between the amiodarone and the control group (p = 0.211, OR = 0.26, 95%CI 0.02–3.06). Interestingly, all deaths occurred in the three groups during the early post-resuscitation period, i.e., within the first 6 h after ROSC, due to hemodynamic instability. Neurological outcome at 48 h was excellent (100 points) for all the nifekalant animals while in the control group two animals had excellent and one average (50 points) neurological scores.
Discussion
The present study shows superiority of nifekalant compared to amiodarone on 48 h survival rates and on multiple hemodynamic parameters during CPR and in the immediate post-resuscitation period. To our knowledge this has not been reported before. A relevant animal study [15] failed to show significant differences between nifekalant and amiodarone on ROSC and 24 h survival rates in a swine model of VF arrest with a non-flow period of 4 min. This phenomenal discrepancy in the results of the two studies might actually represent a very interesting finding consistent with the pathophysiology of VF arrest. According to the 3-phase time-sensitive model VF includes a) an electrical phase, which extends from the time of cardiac arrest to approximately 4 min following the arrest; b) a circulatory phase, from approximately 4 to approximately 10 min after cardiac arrest; and c) a metabolic phase, extending beyond 10 min after cardiac arrest [16]. Time-critical interventions with regard to the phase of VF can affect the outcome. During the electrical phase rapid defibrillation predominates as the most effective treatment, while in the circulatory phase other interventions such as high quality CPR to augment CPP and drugs to improve defibrillation efficacy may have a significant role [18]. Therefore, it seems that in our prolonged (8 min) VF model improved defibrillation efficacy due to nifekalant’s action conferred a significant survival benefit compared to amiodarone, while in the 4 min VF model this effect was blunted by the fact that during the electrical phase the probability of successful defibrillation is already very high.
There is a single report of arithmetical superiority of amiodarone over nifekalant in terms of ROSC and survival to hospital discharge in humans with out-of-hospital VF arrest [13]. A recently published non-randomized study reported equal effectiveness of nifekalant and amiodarone for ROSC and survival to hospital discharge in patients with shock-resistant VF [19]. It is interesting that in both human studies of nifekalant vs. amiodarone, as in our study, the subjects that received nifekalant achieved ROSC more quickly.
Nifekalant or amiodarone administration alone did not terminate VF. However, nifekalant but not amiodarone improved defibrillation efficacy as indicated by the number of shocks required to restore a perfusing rhythm. All the animals in the nifekalant group achieved ROSC after the 1st shock. This finding is consistent with previous reports of improved defibrillation efficacy with nifekalant using either defibrillation threshold [20] or time to ROSC after drug administration [13, 19] as an indirect measure. Verification of this data is of great clinical importance as nifekalant may be a potent anti-arrhythmic, ideal for the conversion of shock-resistant VF to an organized rhythm. Furthermore, earlier conversion of VF to sinus rhythm has a beneficial effect on the neurological outcome of survivors [13, 19]. In the present study all the nifekalant animals that survived to 48 h had an intact neurological function.
In terms of hemodynamic parameters it seems that nifekalant, unlike amiodarone, has favorable effects on aortic pressures and CPP. Amiodarone’s adverse hemodynamic effects during CPR and immediate post-resuscitation period are consistent with a previous animal study on VF arrest [12]. This could possibly be attributed to amiodarone’s α-blocking action antagonizing the α-stimulation of adrenaline. On the other hand nifekalant, as a pure potassium channel blocker, lacks these adverse pharmacological actions [4, 12, 21, 22]. However, in the present study amiodarone prevented ventricular tachyarrhythmias in the immediate post-resuscitation period, while 5 out of the 10 nifekalant animals had an episode of VT after ROSC. In the nifekalant group VT occurred very early (during the first minutes after ROSC), was self-limiting and did not lead to hemodynamic compromise. This might be due to nifekalant’s rapid onset of action and short half-life which is associated with only transient adverse reactions [15]. No TdP was observed in animals treated with nifekalant.
Another interesting finding of the present study is that amiodarone not only failed to improve 48 h survival compared to control, but it also had an unfavorable effect on hemodynamic parameters such as CPP during CPR and SAP and heart rate during the immediate post-resuscitation period [12]. CPP is considered the only key predictor of successful resuscitation [23–25] and short term survival [26–28]. Reduced CPP with amiodarone was associated with worse defibrillation efficacy, arithmetically lower rates of ROSC and significantly lower survival rates in this swine model. It seems that amiodarone administration, via α-blocking action, antagonizes the positive effect of adrenaline on CPP. Furthermore, hypotension and bradycardia after ROSC was common in the animals that received amiodarone and was associated with early post-resuscitation death in this group [29].
Nifekalant hydrochloride was approved in Japan, in June 1999, for the treatment of life-threatening VT and VF in humans [30]. It represents an easily soluble and very stable molecule, with rapid onset of action, suitable for intravenous administration in emergency settings. These properties in combination with its slight effects on hemodynamic status can be beneficial in the treatment of sustained VT or VF in the setting of an acute coronary syndrome [8]. The recommended dose for intravenous administration in humans is 0.15–0.3 mg/kg [7]. Regarding the pharmacokinetics, only the unchanged form is active. The initial rapid fall in plasma nifekalant concentration is observed within 15 min following a single intravenous injection, the elimination half-life is 1.5 h and the volume of distribution is 0.14 L/kg. The urinary excretion ratio for the unchanged form is approximately 30 %. The remaining nifekalant undergoes glucuronate conjugation in the liver [7, 31]. These properties along with its excellent pharmacokinetic profile make it a potentially good alternative to amiodarone in the treatment of VF/pulseless VT cardiac arrest.
Limitations
The sample size was relatively small, albeit adequately powered to demonstrate large differences on 48 h survival. It should be noted that this was a study of pre-shock drug administration, not treatment of refractory VF and therefore it did not intend to assess the foundation for the current CPR guidelines [1, 2]. In the present study no vasoactive drugs were offered to animals with ROSC. This could have an impact on 48 h survival rates mostly in the amiodarone animals that tended to be more hypotensive during the immediate post-resuscitation period compared to nifekalant and control animals. Furthermore, CPR was ceased with the occurrence of asystole/PEA later than 10 min after CPR initiation in animals that did not achieve ROSC (four amiodarone and two control animals). However, the likelihood of ROSC and 48 h survival in these animals was already dismal. The presence of post-resuscitation TdP was recorded as an indirect indicator of clinically significant QT prolongation. Less significant QT changes were not measured. Although we have used previously published doses of nifekalant and amiodarone [15], there are no dose-finding studies supporting the idea that these are the optimal doses for piglets with VF to influence survival. Finally, we should emphasize that this was an experimental animal study, thus extrapolation of our findings to humans should be done with caution.
Conclusions
Early administration of nifekalant in the course of resuscitation improved 48 h survival, defibrillation efficacy and several hemodynamic parameters during CPR and in the immediate post-resuscitation period compared to amiodarone and control. The results of this study indicate that nifekalant might represent a safe and efficient alternative for the treatment of malignant ventricular tachyarrhythmias. Therefore, we underline the need for randomized controlled trials in humans to evaluate its effectiveness compared to amiodarone which is currently recommended as first line therapy for shock-resistant VF/pulseless VT [1, 2].
References
Deakin CD, Nolan JP, Soar J, et al. European resuscitation council guidelines for resuscitation. Section 4. Adult advanced life support. Resuscitation. 2010;81:1305–52.
Neumar RW, Otto CW, Link MS, et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:729–67.
Deakin CD, Morrison LJ, Morley PT, et al. Part 8: advanced life support. 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2010;81:93–174.
Kudenchuk PJ, Cobb LA, Copass MK, et al. Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricular fibrillation. N Engl J Med. 1999;341:871–8.
Dorian P, Cass D, Schwartz B, Cooper R, Gelaznikas R, Barr A. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. N Engl J Med. 2002;346:884–90.
Ishii M, Kamiya J, Hashimoto K. Cellular electrophysiological effects of MS-551, a new class III antiarrhythmic agent. Drug Dev Res. 1995;35:61–8.
Shiga T, Tanaka K, Kato R, et al. Nifekalant versus lidocaine for in-hospital shock-resistant ventricular fibrillation or tachycardia. Resuscitation. 2010;81:47–52.
Yusu S, Ikeda T, Mera H, et al. Effects of intravenous nifekalant as a life saving drug for severe ventricular tachyarrhythmias complicating acute coronary syndrome. Circ J. 2009;73:2021–8.
Tahara Y, Kimura K, Kosuge M, et al. Comparison of nifekalant and lidocaine for the treatment of shock-refractory ventricular fibrillation. Circ J. 2006;70:442–6.
Nagao K. Nifekalant hydrochloride for patients with cardiac arrest caused by shockable rhythm. Circ J. 2010;74:2308–13.
Pantazopoulos IN, Troupis GT, Pantazopoulos CN, Xanthos TT. Nifekalant in the treatment of life-threatening ventricular tachyarrhythmias. World J Cardiol. 2011;3:169–76.
Karlis G, Iacovidou N, Lelovas P, et al. Effects of early amiodarone administration during and immediately after cardiopulmonary resuscitation in a swine model. Acta Anaesthesiol Scand. 2014;58:114–22.
Amino M, Yoshioka K, Opthof T, et al. Comparative study of nifekalant versus amiodarone for shock-resistant ventricular fibrillation in out-of-hospital cardiopulmonary arrest patients. J Cardiovasc Pharmacol. 2010;55:391–8.
Xanthos T, Lelovas P, Vlachos I, et al. Cardiopulmonary arrest and resuscitation in Landrace/Large White swine: a research model. Lab Anim. 2007;41:353–62.
Ji XF, Li CS, Wang S, Yang L, Cong LH. Comparison of the efficacy of nifekalant and amiodarone in a porcine model of cardiac arrest. Resuscitation. 2010;81:1031–6.
Weisfeldt ML, Becker LB. Resuscitation after cardiac arrest: a 3-phase time-sensitive model. JAMA. 2002;288:3035–8.
Xanthos T, Bassiakou E, Koudouna E, et al. Combination pharmacotherapy in the treatment of experimental cardiac arrest. Am J Emerg Med. 2009;27:651–9.
Gilmore CM, Rea TD, Becker LJ, Eisenberg MS. Three-phase model of cardiac arrest: time-dependent benefit of bystander cardiopulmonary resuscitation. Am J Cardiol. 2006;98:497–9.
Harayama N, Nihei SI, Nagata K, et al. Comparison of nifekalant and amiodarone for resuscitation of out-of-hospital cardiopulmonary arrest resulting from shock-resistant ventricular fibrillation. J Anesth. 2014;28:587–92.
Murakawa Y, Yamashita T, Kanese Y, Omata M. Can a class III antiarrhythmic drug improve electrical defibrillation efficacy during ventricular fibrillation? J Am Coll Cardiol. 1997;29:688–92.
Santangeli P, Di Biase L, Burkhardt JD, et al. Examining the safety of amiodarone. Expert Opin Drug Saf. 2012;11:191–214.
Ohashi J, Yasuda S, Miyazaki S, et al. Prevention of life-threatening ventricular tachyarrhythmia by a novel and pure class-III agent, nifekalant hydrochloride. J Cardiovasc Pharmacol. 2006;48:274–9.
Xanthos T, Iacovidou N, Pantazopoulos I, et al. Ischaemia-modified albumin predicts the outcome of cardiopulmonary resuscitation: an experimental study. Resuscitation. 2010;81:591–5.
Sanders AB, Ogle M, Ewy GA. Coronary perfusion pressure during cardiopulmonary resuscitation. Am J Emerg Med. 1985;3:11–4.
Sanders AB, Kern KB, Atlas M, Bragg S, Ewy GA. Importance of the duration of inadequate coronary perfusion pressure on resuscitation from cardiac arrest. J Am Coll Cardiol. 1985;6:113–8.
Niemann JT, Rosborough JP, Niskanen RA, Alferness C, Criley JM. Mechanical “cough” cardiopulmonary resuscitation during cardiac arrest in dogs. Am J Cardiol. 1985;55:199–204.
Feneley MP, Maier GW, Kern KB, et al. Influence of compression rate on initial success of resuscitation and 24-hour survival after prolonged manual cardiopulmonary resuscitation in dogs. Circulation. 1988;77:240–50.
Kern KB, Sanders AB, Badylak SF, et al. Long-term survival with open-chest cardiac massage after ineffective closed-chest compression in a canine preparation. Circulation. 1987;75:498–503.
Dragancea I, Rundgren M, Englund E, Friberg H, Cronberg T. The influence of induced hypothermia and delayed prognostication on the mode of death after cardiac arrest. Resuscitation. 2013;84:337–42.
Oyabe A, Sano H. Pharmacological and clinical profile of nifekalant (shinbit injection), a class III antiarrhythmic drug. Nihon Yakurigaku Zasshi. 2002;119:103–9.
Myoishi M, Yasuda S, Miyazaki S, et al. Intravenous administration of nifekalant hydrochloride for the prevention of ischemia-induced ventricular tachyarrhythmia in patients with renal failure undergoing hemodialysis. Circ J. 2003;67:898–900.
Acknowledgments
The authors would like to thank Experimental-Research Center ELPEN Pharmaceuticals (ERCE) for their constant technical assistance during this project.
Conflict of Interest
George Karlis has received a research scholarship from ERCE. The other authors report no conflict of interest.
Ethical Approval
All applicable international, national, and institutional guidelines for the care and use of animals were followed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karlis, G., Iacovidou, N., Lelovas, P. et al. Nifekalant Versus Amiodarone in the Treatment of Cardiac Arrest: an Experimental Study in a Swine Model of Prolonged Ventricular Fibrillation. Cardiovasc Drugs Ther 29, 425–431 (2015). https://doi.org/10.1007/s10557-015-6604-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-015-6604-7