Abstract
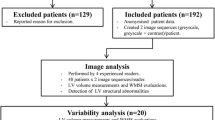
Contrast enhanced echocardiography (CEE) is a technique for the improvement of suboptimal echocardiographic studies. While commonly performed at selected institutions, its value has only been shown qualitatively, and to this point no study has been directed at establishing a quantitative improvement in image quality compared with non-contrast enhanced echocardiography (non-CEE). The purpose of this study was to quantitatively measure the effect of contrast on the quality of images obtained during non-CEE versus CEE. Thirty consecutive patients underwent CEE. In all subjects a non-CEE was obtained prior to administering any contrast, allowing for a direct comparison and an internal control group. Sharpness of the septal, apical and lateral myocardial walls in the apical 4-chamber view was calculated with and without contrast. Three signal intensity levels were obtained for each wall then averaged to compare the images with and without contrast for a statistically significant difference in sharpness. Quantitative analysis showed a significant difference in sharpness between CEE and non-CEE in the left ventricular septal myocardial wall, p < 0.01. A more drastic significant increase in image sharpness was observed between non-CEE and CEE in the apical and lateral left ventricular myocardial walls, both p < 0.000001. CEE significantly increases the sharpness at all left ventricular myocardial walls thus allowing higher quality images with presumably more accurate diagnosis of regional wall motion abnormalities, left ventricular endocardial border detection, left ventricular dimensions, ejection fraction and apical pathology.



Similar content being viewed by others
References
Pearlman JD et al (1988) Limits of normal left ventricular dimensions in growth and development: analysis of dimensions and variance in the two-dimensional echocardiograms of 268 normal healthy subjects. J Am Coll Cardiol 12(6):1432–1441
Pearlman AS et al (2007) Evolving trends in the use of echocardiographyA study of medicare beneficiaries. J Am Coll Cardiol 49(23):2283–2291
Crouse LJ et al (1993) Opacification and border delineation improvement in patients with suboptimal endocardial border definition in routine echocardiography: results of the phase III Albunex multicenter trial. J Am Coll Cardiol 22(5):1494–1500
Yong Y et al (2002) Diagnostic accuracy and cost-effectiveness of contrast echocardiography on evaluation of cardiac function in technically very difficult patients in the intensive care unit. Am J Cardiol 89(6):711–718
Seward JB et al (1977) Peripheral venous contrast echocardiography. Am J Cardiol 39(2):202–212
Cohen JL et al (1998) Improved left ventricular endocardial border delineation and opacification with OPTISON (FS069), a new echocardiographic contrast agent results of a phase III multicenter trial. J Am Coll Cardiol 32(3):746–752
Abdelmoneim SS et al (2009) Safety of contrast agent use during stress echocardiographyA 4-year experience from a single-center cohort study of 26,774 patients. JACC Cardiovasc Imaging 2(9):1048–1056
Platts DG et al (2013) The safety profile of Perflutren microsphere contrast echocardiography during rest and stress imaging: results from an Australian multicentre cohort. Heart Lung Circ 22(12):996–1002
Aggeli C et al (2012) Ultrasound contrast agents: updated data on safety profile. Curr Pharm Des 18(15):2253–2258
Weiss RJ et al (2012) CaRES (Contrast Echocardiography Registry for Safety Surveillance): a prospective multicenter study to evaluate the safety of the ultrasound contrast agent Definity in clinical practice. J Am Soc Echocardiogr 25(7):790–795
Yu EH et al (2003) Determination of left ventricular ejection fraction using intravenous contrast and a semiautomated border detection algorithm. J Am Soc Echocardiogr 16(1):22–28
Weinsaft JW et al (2009) Contrast-enhanced anatomic imaging as compared to contrast-enhanced tissue characterization for detection of left ventricular thrombus. JACC Cardiovasc Imaging 2(8):969–979
Kurt M et al (2009) Impact of contrast echocardiography on evaluation of ventricular function and clinical management in a large prospective cohort. J Am Coll Cardiol 53(9):802–810
Plana JC et al (2008) A randomized cross-over study for evaluation of the effect of image optimization with contrast on the diagnostic accuracy of dobutamine echocardiography in coronary artery disease. The OPTIMIZE trial. JACC Cardiovasc Imaging 1(2):145–152
Feinstein SB (2011) Update-clinical value of contrast-enhanced ultrasound. US Cardiol 8(2):98–101
Herzog CA (2008) Incidence of adverse events associated with use of perflutren contrast agents for echocardiography. JAMA, J Am Med Assoc 299(17):2023–2025
Dickstein K et al (2008) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008 the task force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 29(19):2388–2442
Groves EM et al (2007) Quantitative analysis of ECG-gated high-resolution contrast-enhanced MR angiography of the thoracic aorta. Am J Roentgenol 188(2):522–528
Carr JC et al (2002) High-resolution breath-hold contrast-enhanced MR angiography of the entire carotid circulation. Am J Roentgenol 178(3):543–549
Hundley WG et al (1998) Administration of an intravenous perfluorocarbon contrast agent improves echocardiographic determination of left ventricular volumes and ejection fraction: comparison with cine magnetic resonance imaging. J Am Coll Cardiol 32(5):1426–1432
Hoffmann R et al (2006) Analysis of regional left ventricular function by cine ventriculography, cardiac magnetic resonance imaging, and unenhanced and contrast-enhanced echocardiographyA multicenter comparison of methods. J Am Coll Cardiol 47(1):121–128
Demos TC et al (2004) Venous anomalies of the thorax. Am J Roentgenol 182(5):1139–1150
Walker S et al (2013) Cost-effectiveness of cardiovascular magnetic resonance in the diagnosis of coronary heart disease: an economic evaluation using data from the CE-MARC study. Heart 99(12):873–881
Sharples L et al (2007) Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial. Gray Pub, Tunbridge Wells, Kent
Thomson HL et al (2001) Contrast echocardiography improves the accuracy and reproducibility of left ventricular remodeling measurements a prospective, randomly assigned, blinded study. J Am Coll Cardiol 38(3):867–875
Mulvagh SL et al (2008) American Society of echocardiography consensus statement on the clinical applications of ultrasonic contrast agents in echocardiography. J Am Soc Echocardiogr 21(11):1179–1201
Acknowledgments
We would like to thank the outstanding staff of echocardiographers in our institution, in particular Bryan Gen Kuong.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Glassy, M.S., Groves, E.M. Analysis of the quantitative improvements in resting echocardiographic image sharpness through the use of contrast enhanced echocardiography. Int J Cardiovasc Imaging 30, 867–873 (2014). https://doi.org/10.1007/s10554-014-0401-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-014-0401-4