Abstract
Purpose
It has been suggested that home paint exposure increases the risk of childhood acute lymphoblastic leukemia (ALL).
Methods
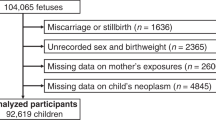
We obtained individual level data from eight case–control studies participating in the Childhood Leukemia International Consortium. All studies had home paint exposure data (sometimes including lacquers and varnishes) for the pregnancy period with additional data for the 1–3-month period before conception in five, the year before conception in two, and the period after birth in four studies, respectively. Cytogenetic subtype data were available for some studies. Data were harmonized to a compatible format. Pooled analyses of individual data were undertaken using unconditional logistic regression.
Results
Based on 3,002 cases and 3,836 controls, the pooled odds ratio (OR) for home paint exposure in the 1–3 months before conception and risk of ALL was 1.54 [95 % confidence interval (CI) 1.28, 1.85], while based on 1,160 cases and 1,641 controls for exposure in the year before conception, it was 1.00 (95 % CI 0.86, 1.17). For exposure during pregnancy, using 4,382 cases and 5,747 controls, the pooled OR was 1.14 (95 % CI 1.04, 1.25), and for exposure after birth, the OR was 1.22 (95 % CI 1.07, 1.39), based on data from 1,962 cases and 2,973 controls. The risk was greater for certain cytogenetic subtypes and if someone other than the parents did the painting.
Conclusions
Home paint exposure shortly before conception, during pregnancy, and/or after birth appeared to increase the risk of childhood ALL. It may be prudent to limit exposure during these periods.
Similar content being viewed by others
Abbreviations
- ALL:
-
Acute lymphoblastic leukemia
- Aus-ALL:
-
Australian Study of Causes of Acute Lymphoblastic Leukaemia in Children
- CI:
-
Confidence interval
- CLIC:
-
Childhood Leukemia International Consortium
- COG:
-
Childhood Oncology Group (Children’s Cancer Group)
- NARECHEM:
-
Nationwide Registration for Childhood Haemotological Malignancies
- NCCLS:
-
Northern California Childhood Leukemia Study (USA)
- NZCCS:
-
New Zealand Childhood Cancer Study
- OR:
-
Odds ratio
- RDD:
-
Random digit dialing
References
International Agency for Research on Cancer (2010) Painting, firefighting, and shiftwork/IARC monographs in the evaluation of carcinogenic risks in humans, vol 98. International Agency for Research on Cancer, Lyon
Metayer C, Milne E, Clavel J et al (2013) The Childhood Leukemia International Consortium. Cancer Epidemiol 37(3):336–347
Bailey HD, Fritschi L, Metayer C et al (2014) Parental occupational paint exposure and risk of childhood leukemia in the offspring: findings from the Childhood Leukemia International Consortium. Cancer Causes Control 25(10):1351–1367
Scelo G, Metayer C, Zhang L et al (2009) Household exposure to paint and petroleum solvents, chromosomal translocations, and the risk of childhood leukemia. Environ Health Perspect 117(1):133–139
Lowengart RA, Peters JM, Cicioni C et al (1987) Childhood leukemia and parents’ occupational and home exposures. J Natl Cancer Inst 79(1):39–46
Bailey HD, Milne E, de Klerk NH et al (2011) Exposure to house painting and the use of floor treatments and the risk of childhood acute lymphoblastic leukemia. Int J Cancer 128(10):2405–2414
Freedman DM, Stewart P, Kleinerman RA et al (2001) Household solvent exposures and childhood acute lymphoblastic leukemia. Am J Public Health 91(4):564–567
Wiemels JL, Cazzaniga G, Daniotti M et al (1999) Prenatal origin of acute lymphoblastic leukaemia in children. Lancet 354(9189):1499–1503
Infante-Rivard C, Siemiatycki J, Lakhani R et al (2005) Maternal exposure to occupational solvents and childhood leukemia. Environ Health Perspect 113(6):787–792
Tibbetts J (2002) Under construction: building a safer industry. Environ Health Perspect 110(3):A134–A141
Australian Paint Approval Scheme (2006) Volatile organic compounds (VOC) limits [internet]. http://www.apas.gov.au/PDFs/D181.pdf
Alderton LE, Spector LG, Blair CK et al (2006) Child and maternal household chemical exposure and the risk of acute leukemia in children with Down’s syndrome: a report from the Children’s Oncology Group. Am J Epidemiol 164(3):212–221
Greaves M (2006) Infection, immune responses and the aetiology of childhood leukaemia. Nat Rev Cancer 6(3):193–203
Greaves MF, Wiemels J (2003) Origins of chromosome translocations in childhood leukaemia. Nat Rev Cancer 3(9):639–649
Greaves MF, Maia AT, Wiemels JL et al (2003) Leukemia in twins: lessons in natural history. Blood 102(7):2321–2333
Raw GJ, Coward SK, Brown VM et al (2004) Exposure to air pollutants in English homes. J Expo Anal Environ Epidemiol 14(Suppl 1):S85–S94
Tavian M, Biasch K, Sinka L et al (2010) Embryonic origin of human hematopoiesis. Int J Dev Biol 54(6–7):1061–1065
Van De Mark MR, Sandefur KD, Durham KA (2005) Paint. In: Kirk–Othmer encyclopedia of chemical technology, 5th edn. Wiley, New York, pp 54–75
European Commission (2013) Report on the implementation of Directive 2004/42/EC of the European Parliament and of the Council on the limitation of emissions of volatile organic compounds due to the use of organic solvents in certain paints and varnishes and vehicle refinishing products and amending Directive 1999/13/EC. http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:32004L0042
Hertz-Picciotto I, Pastore LM, Beaumont JJ (1996) Timing and patterns of exposures during pregnancy and their implications for study methods. Am J Epidemiol 143(6):597–607
Sorensen M, Andersen AMN, Raaschou-Nielsen O (2010) Non-occupational exposure to paint fumes during pregnancy and fetal growth in a general population. Environ Res 110(4):383–387. doi:10.1016/j.envres.2010.02.011
Schuz J, Spector LG, Ross JA (2003) Bias in studies of parental self-reported occupational exposure and childhood cancer. Am J Epidemiol 158(7):710–716
Acknowledgments
We would like to thank Dr. Maria S Pombo-de-Oliveira, Instituto Nacional de Câncer (INCA) who was one of experts in molecular biology who reviewed the consistency of CLIC cytogenetic data. We would like to thank our dear colleague and friend, Patricia Buffler, who passed away before the submission of this manuscript. She was a founding member and Chair of CLIC as well as the driving force behind the NCCLS. She provided unconditional support to finding the causes of childhood leukemia, and her scientific leadership and guiding forces within CLIC will be remembered. The Aus-ALL consortium conducted the study and the Telethon Kids Institute (formerly Telethon Institute for Child Health Research; TICHR), University of Western Australia, was the coordinating center. Bruce Armstrong (Sydney School of Public Health), Elizabeth Milne (TICHR), Frank van Bockxmeer (Royal Perth Hospital), Michelle Haber (Children’s Cancer Institute Australia), Rodney Scott (University of Newcastle), John Attia (University of Newcastle), Murray Norris (Children’s Cancer Institute Australia), Carol Bower (TICHR), Nicholas de Klerk (TICHR), Lin Fritschi (WA Institute for Medical Research, WAIMR), Ursula Kees (TICHR), Margaret Miller (Edith Cowan University), Judith Thompson (WA Cancer Registry) were the research investigators, and Helen Bailey (TICHR) was the project coordinator. The clinical investigators were: Frank Alvaro (John Hunter Hospital, Newcastle); Catherine Cole (Princess Margaret Hospital for Children, Perth); Luciano Dalla Pozza (Children’s Hospital at Westmead, Sydney); John Daubenton (Royal Hobart Hospital, Hobart); Peter Downie (Monash Medical Centre, Melbourne); Liane Lockwood (Royal Children’s Hospital, Brisbane); Maria Kirby (Women’s and Children’s Hospital, Adelaide); Glenn Marshall (Sydney Children’s Hospital, Sydney); Elizabeth Smibert (Royal Children’s Hospital, Melbourne); Ram Suppiah (previously Mater Children’s Hospital, Brisbane). NARECHEM Greek Pediatric Hematology Oncology Clinicians: Margarita Baka M.D. (Department of Pediatric Hematology–Oncology, “Pan.&Agl. Kyriakou” Children’s Hospital, Athens), Maria Moschovi M.D., Sophia Polychronopoulou M.D. (Departments of Pediatric Hematology–Oncology, “A. Sophia” Children’s Hospital, Athens); Emmanuel Hatzipantelis M.D., Ph.D (Pediatric Hematology Oncology Unit, 2nd Pediatric Department of Aristotle University, AHEPA General Hospital, Thessaloniki); Maria Kourti M.D. (Pediatric Oncology Department, Hippokration Hospital, Thessaloniki); Eftychia Stiakaki M.D. (Department of Pediatric Hematology-Oncology, University Hospital of Heraklion, Heraklion); Ioannis Matsoukis M.D. (Department of Hygiene, Epidemiology and Medical Statistics, Athens University Medical School, 11527 Athens); Nick Dessypris, M.Sc., Ph.D and Evanthia Bouka, M.PH: Department of Hygiene, Epidemiology and Medical Statistics, Athens University Medical School, 11527 Athens, Greece. The New Zealand Childhood Cancer Study was coordinated at the University of Otago, where the study team included JD Dockerty, GP Herbison (who helped prepare data for this pooled analysis), DCG Skegg, and JM Elwood. The names of the interviewers, secretaries, research assistants, clinicians, pathologists, and cancer registry staff who contributed are listed in earlier publications from the NZ study. COG: The E15 cohort of the Children’s Oncology Group was identified by CCG (Children’s Cancer Group) principle and affiliate member institutions. Further information can be found on the web site: http://www.curesearch.org/. The NCCLS thanks the families for their participation and the clinical investigators at the following collaborating hospitals for help in recruiting patients: University of California Davis Medical Center (Dr. J. Ducore), University of California San Francisco (Drs. M. Loh and K. Matthay), Children’s Hospital of Central California (Dr. V. Crouse), Lucile Packard Children’s Hospital (Dr. G. Dahl), Children’s Hospital Oakland (Dr. J. Feusner), Kaiser Permanente Roseville (former Sacramento; Drs. K. Jolly and V. Kiley), Kaiser Permanente Santa Clara (Drs. C. Russo, A. Wong, and D. Taggart), Kaiser Permanente San Francisco (Dr. K. Leung), and Kaiser Permanente Oakland (Drs. D. Kronish and S. Month). Finally, the NCCLS thanks the entire study staff and former University of California, Berkeley Survey Research Center for their effort and dedication. The French authors would like to thank all of the Société Française de lutte contre les Cancers de l’Enfant et de l’Adolescent (SFCE) principal investigators: André Baruchel (Hôpital Saint-Louis/Hôpital Robert Debré, Paris), Claire Berger (Centre Hospitalier Universitaire, Saint-Etienne), Christophe Bergeron (Centre Léon Bérard, Lyon), Jean-Louis Bernard (Hôpital La Timone, Marseille), Yves Bertrand (Hôpital Debrousse, Lyon), Pierre Bordigoni (Centre Hospitalier Universitaire, Nancy), Patrick Boutard (Centre Hospitalier Régional Universitaire, Caen), Gérard Couillault (Hôpital d’Enfants, Dijon), Christophe Piguet (Centre Hospitalier Régional Universitaire, Limoges), Anne-Sophie Defachelles (Centre Oscar Lambret, Lille), François Demeocq (Hôpital Hôtel-Dieu, Clermont-Ferrand), Alain Fischer (Hôpital des Enfants Malades, Paris), Virginie Gandemer (Centre Hospitalier Universitaire – Hôpital Sud, Rennes), Dominique Valteau-Couanet (Institut Gustave Roussy, Villejuif), Jean-Pierre Lamagnere (Centre Gatien de Clocheville, Tours), Françoise Lapierre (Centre Hospitalier Universitaire Jean Bernard, Poitiers), Guy Leverger (Hôpital Armand-Trousseau, Paris), Patrick Lutz (Hôpital de Hautepierre, Strasbourg), Geneviève Margueritte (Hôpital Arnaud de Villeneuve, Montpellier), Françoise Mechinaud (Hôpital Mère et Enfants, Nantes), Gérard Michel (Hôpital La Timone, Marseille), Frédéric Millot (Centre Hospitalier Universitaire Jean Bernard, Poitiers), Martine Münzer (American Memorial Hospital, Reims), Brigitte Nelken (Hôpital Jeanne de Flandre, Lille), Hélène Pacquement (Institut Curie, Paris), Brigitte Pautard (Centre Hospitalier Universitaire, Amiens), Stéphane Ducassou (Hôpital Pellegrin Tripode, Bordeaux), Alain Pierre-Kahn (Hôpital Enfants Malades, Paris), Emmanuel Plouvier (Centre Hospitalier Régional, Besançon), Xavier Rialland (Centre Hospitalier Universitaire, Angers), Alain Robert (Hôpital des Enfants, Toulouse), Hervé Rubie (Hôpital des Enfants, Toulouse), Stéphanie Haouy (Hôpital Arnaud de Villeneuve, Montpellier), Christine Soler (Fondation Lenval, Nice), and Jean-Pierre Vannier (Hôpital Charles Nicolle, Rouen). The Canada Québec Study was conducted in the province over a 20-year period in all university-affiliated pediatric center hospitals designated to diagnose and treat pediatric cancers, under the direction of Claire Infante-Rivard. Main support collaborators were Alexandre Cusson, Marcelle Petitclerc, and Denyse Hamer. We thank all families for their generous participation. The authors declare that they have no conflict of interest. The work reported in this paper by Helen Bailey was undertaken mostly during the tenure of a Postdoctoral Fellowship from the International Agency for Research on Cancer (IARC), partially supported by the European Commission FP7 Marie Curie Actions—People—Co-funding of regional, national, and international programmes (COFUND), with additional support by the Environment and Radiation Section of IARC. The CLIC administration, annual meetings, and pooled analyses are partially supported by the National Cancer Institute, NCI, USA (Grant R03 CA132172), National Institute of Environmental Health Sciences, NIEHS, USA (Grants P01 ES018172, R01 ES009137, R13 ES021145, R13 ES022868, R13 ES024632 and R13 ES021145-01), the Environmental Protection Agency, EPA, USEPA, USA (Grant RD83451101), the Children with Cancer, CwC, UK (Award No. 2010/097), and Alex’s Lemonade Stand Foundation (Grant 20140461). Aus-ALL was supported by the Australian National Health and Medical Research Council (Grant ID 254539). The Canadian study was funded by the National Cancer Institute of Canada; Grant numbers: #014113, #010735-CERN #RFA0405; the Medical Research Council of Canada; Grant number: MOP 37951; the Fonds de la recherche en santé du Québec; Grant number: #981141; the Bureau of Chronic Disease Epidemiology, Canada; Health and Welfare Canada; the Leukemia Research Fund of Canada; and the National Health and Research Development Program, Ottawa. France: ADELE Grant sponsors: INSERM, the French Ministère de l’Environnement, the Association pour la Recherche contre le Cancer, the Fondation de France, the Fondation Jeanne Liot, the Fondation Weisbrem-Berenson, the Ligue Contre le Cancer du Val de Marne, the Ligue Nationale Contre le Cancer. NARECHEM is supported in part by the National and Kapodistrian University, Athens, Greece. The New Zealand Childhood Cancer Study was funded by the Health Research Council of NZ, the NZ Lottery Grants Board, the Otago Medical School (Faculty Bequest Funds), the Cancer Society of NZ, the Otago Medical Research Foundation, and the A. B. de Lautour Charitable Trust. The Northern California Childhood Leukemia Study (NCCLS) is supported by the National Institutes of Health (NIH), USA (Grants P01 ES018172, R01 ES09137, and P42-ES004705), Environmental Protection Agency (USEPA), USA (Grant RD83451101), and the CHILDREN with CANCER (CwC), UK (former Children with Leukaemia), for data collection. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, USEPA, or the CwC. COG: The E15 cohort of the Children’s Oncology Group was funded by National Institutes of Health (NIH), USA (Grants R01CA049450 (E14) and R01CA048051 (E15)), and the Children’s Cancer Research Fund, Minneapolis, MN.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bailey, H.D., Metayer, C., Milne, E. et al. Home paint exposures and risk of childhood acute lymphoblastic leukemia: findings from the Childhood Leukemia International Consortium. Cancer Causes Control 26, 1257–1270 (2015). https://doi.org/10.1007/s10552-015-0618-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-015-0618-0