Abstract
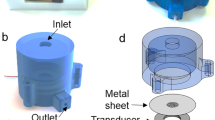
An implantable sensor system for long-term monitoring of blood pressure is realized by taking advantage of the correlation between pulse transit time and blood pressure. The highly integrated implantable sensor module, fabricated using MEMS technologies, uses 8 light emitting diodes (LEDs) and a photodetector on chip level. The sensor is applied to large blood vessels, such as the carotid or femoral arteries, and allows extravascular measurement of highly-resolved photoplethysmograms. In addition, spectrophotometric approaches allow measurement of hemoglobin derivatives. For the calibration of blood pressure measurements, the sensor system has been successfully implemented in animal models.












Similar content being viewed by others
References
J. Allen, Photoplethysmography and its application in clinical physiological measurement. Physiol. Meas. 28(3), 1–39 (2007)
S.J. Barker, J.J. Badal, The measurement of dyshemoglobins and total hemoglobin by pulse oximetry. Curr. Opin. Anaesthesiol. 21(6), 805–810 (2008)
S. Bartsch, D. Ostojic, H. Schmalgemeier, T. Bitter, N. Westerheide, S. Eckert, D. Horstkotte, O. Oldenburg, Validation of continuous blood pressure measurements by pulse transit time: a comparison with invasive measurements in a cardiac intensive care unit. Dtsch. Med. Wochenschr. 135(48), 2406–2412 (2010)
J.M. Bland, D.G. Altman, Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet 346(8982), 1085–1087 (1995)
J.M. Bland, D.G. Altman, Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476), 307–310 (1986)
R. Coifman, D. Donoho, Translation-invariant de-noising. Wavelets Stat., Springer Lect. Notes Stat. 103, 125–150 (1995)
K.R. Coombes, S. Tsavachidis, J.S. Morris, K. Baggerly, M.C. Hung, H.M. Kuerer, Improved peak detection and quantification of mass spectrometry data acquired from surface-enhanced laser desorption and ionization by denoising spectra with the undecimated discrete wavelet transform. Proteomics 5(16), 4107–4117 (2005)
D. Donoho, De-noising by soft-thresholding. IEEE Trans. Inf. Theory. 41(3), 613–627 (1995)
M.J. Drinnan, J. Allen, A. Murray, Relation between heart rate and pulse transit time during paced respiration. Physiol. Meas. 22(3), 425–432 (2001)
P. Einbrodt, Über den Einfluß der Atembewegung auf Herzschlag und Blutdruck. Sber. Akad. Wiss. Wien; Math. Nat. Kl., 2. Abt., 40 (1860)
J. Fiala, R. Gehrke, N. Weber, P. Bingger, H. Zappe, A. Seifert, Implantable optical sensor for continuous monitoring of various hemoglobin derivatives and tissue perfusion. IEEE Sensors 1971–1974 (2009). doi:10.1109/ICSENS.2009.5398324
J. Fiala, P. Bingger, K. Foerster, C. Heilmann, F. Beyersdorf, H. Zappe, A. Seifert, Implantable sensor for blood pressure determination via pulse transit time. IEEE Sensors 1226–1229 (2010). doi:10.1109/ICSENS.2010.5690619
J. Fortin, W. Marte, R. Grüllenberger, A. Hacker, W. Habenbacher, A. Heller, C. Wagner, P. Wach, F. Skrabal, Continuous non-invasive blood pressure monitoring using concentrically interlocking control loops. Comput. Biol. Med. 36(9), 941–957 (2006)
R. Furlan, S. Guzzetti, W. Crivellaro, S. Dassi, M. Tinelli, G. Baselli, S. Cerutti, F. Lombardi, M. Pagani, A. Malliani, Continuous 24-hour assessment of the neural regulation of systemic arterial pressure and RR variabilities in ambulant subjects. Circulation 81(2), 537–547 (1990)
B. Gribbin, A. Steptoe, P. Sleight, Pulse wave velocity as a measure of blood pressure change. Psychophysiology 13(1), 86–90 (1976)
C. Jeleazcov, L. Krajinovic, T. Münster, T. Birkholz, R. Fried, J. Schüttler, J. Fechner, Precision and accuracy of a new device (CNAPTM) for continuous non-invasive arterial pressure monitoring: assessment during general anaesthesia. Br. J. Anaesth. 105(3), 264–272 (2010)
A. Johansson, C. Ahlstrom, T. Lanne, P. Ask, Pulse wave transit time for monitoring respiration rate. Med. Biol. Eng. Comput. 44(6), 471–478 (2006)
P.M. Kearney, M. Whelton, K. Reynolds, P. Muntner, P.K. Whelton, J. He, Global burden of hypertension: analysis of worldwide data. Lancet 365(9455), 217–223 (2005)
K. Kotani, K. Takamasu, Y. Jimbo, Y. Yamamoto, Postural-induced phase shift of respiratory sinus arrhythmia and blood pressure variations: insight from respiratory-phase domain analysis. Am. J. Physiol. Heart Circ. Physiol. 294(3), H1481–H1489 (2008)
W.H. Kullmann, Y. Zhao, T. Bischof, Hemodynamic modeling strategy for non-invasive online monitoring of arterial blood pressure based on pulse transit time detection. Biomed. Tech. 55(1), 1–4 (2010)
M. Masè, W. Mattei, R. Cucino, L. Faes, G. Nollo, Feasibility of cuff-free measurement of systolic and diastolic arterial blood pressure. J. Electrocardiol. 44(2), 201–207 (2011)
M.G. Mohaupt, J. Schmidli, F.C. Luft, Management of uncontrollable hypertension with a carotid sinus stimulation device. Hypertension 50(5), 825–828 (2007)
W.W. Nichols, M.F. O’Rourke, C. Vlachopoulos, McDonald’s Blood Flow in Arteries: Theoretical, Experimental and Clinical Principles, 6th edn. (Hodder Arnold, New York 2011)
P.A. Obrist, K.C. Light, J.A. McCubbin, J.S. Hutcheson, J.L. Hoffer, Pulse transit time: relationship to blood pressure and myocardial performance. Psychophysiology 16(3), 292–301 (1979)
R. Payne, C. Symeonides, Pulse transit time measured from the ECG: an unreliable marker of beat-to-beat blood pressure. J. Appl. Physiol. 100, 136–141 (2006)
J. Peñaz, Photoelectric measurement of blood pressure, volume and flow in the finger. Digest of the 10th International Conference on Medical and Biological Engineering, pp. 162–164. (Dresden 1973)
J. Peñaz, A. Voigt, W. Teichmann, Beitrag zur fortlaufenden indirekten Blutdruckmessung. Z. Gesamte. Inn. Med. 31, 1030–1033 (1976)
D.J. Pitson, A. Sandell, R. van den Hout, J.R. Stradling, Use of pulse transit time as a measure of inspiratory effort in patients with obstructive sleep apnoea. Eur. Respir. J. 8(10), 1669–1674 (1995)
J. Potkay, Long term, implantable blood pressure monitoring systems. Biomedical Microdevices 10(3), 379–392 (2008)
A. Reisner, P.A. Shaltis, D.B. McCombie, H. Asada, Utility of the photoplethysmogram in circulatory monitoring. Anesthesiology 108(5), 950–958 (2008)
W.A. Riley, R.W. Barnes, G.W. Evans, G.L. Burke, Ultrasonic measurement of the elastic modulus of the common carotid artery. The Atherosclerosis Risk in Communities (ARIC) Study. Stroke 23(7), 952–956 (1992)
D. Sommermeyer, M. Schwaibold, B. Schöller, L. Grote, J. Hedner, A. Bolz, Cardiovascular risk: analysis of the photoplethysmographic pulse wave signal. Biomed. Tech. 55(1), 85–88 (2010)
A. Steptoe, H. Smulyan, B. Gribbin, Pulse wave velocity and blood pressure change: calibration and applications. Psychophysiology 13(5), 488–493 (1976)
J Thomas (1955) A method for continuously indicating blood pressure. J. Physiol. (Lond.) 129(3), 75–76
N.C. Tsai, C.Y. Sue, Review of MEMS-based drug delivery and dosing systems. Sensor. Actuat. A-Phys. 134(2), 555–564 (2007)
M.Y.M. Wong, C.C.Y. Poon, Y.T. Zhang, An evaluation of the cuffless blood pressure estimation based on pulse transit time technique: a half year study on normotensive subjects. Cardiovasc. Eng. 9(1), 32–38 (2009)
Y. Zhao, M. Yamamoto, M. Munakata, M. Nakao, N. Katayama, Investigation of the time delay between variations in heart rate and blood pressure. Med. Biol. Eng. Comput. 37(3), 344–347 (1999)
Acknowledgements
The authors thank Peter Liebetraut for his measurements analyzing the material properties of silicones. This work was financially supported by the Baden-Württemberg Stiftung.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fiala, J., Bingger, P., Ruh, D. et al. An implantable optical blood pressure sensor based on pulse transit time. Biomed Microdevices 15, 73–81 (2013). https://doi.org/10.1007/s10544-012-9689-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10544-012-9689-9