Abstract
This study investigated the ability of aerosolized bovine lactoferrin (bLF) to protect the lungs from injury induced by chronic hyperoxia. Female CD-1 mice were exposed to hyperoxia (FiO2 = 80 %) for 7 days to induce lung injury and fibrosis. The therapeutic effects of bLF, administered via an aerosol delivery system, on the chronic lung injury induced by this period of hyperoxia were measured by bronchoalveolar lavage, lung histology, cell apoptosis, and inflammatory cytokines in the lung tissues. After exposure to hyperoxia for 7 days, the survival of the mice was significantly decreased to 20 %. The protective effects of bLF against hyperoxia were further confirmed by significant reductions in lung edema, total cell numbers in bronchoalveolar lavage fluid, inflammatory cytokines (IL-1β and IL-6), pulmonary fibrosis, and apoptotic DNA fragmentation. The aerosolized bLF protected the mice from oxygen toxicity and increased the survival fraction to 66.7 % in the hyperoxic model. The results support the use of an aerosol therapy with bLF in intensive care units to reduce oxidative injury in patients with severe hypoxemic respiratory failure or chronic obstructive pulmonary disease.
Similar content being viewed by others
Introduction
Acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) are common causes of morbidity and mortality in intensive care units. ALI is characterized by refractory hypoxemia due to widespread alveolar flooding after an insult due to direct intra-alveolar injury or indirect injury following systemic inflammation. The principal management of ALI includes treatment of the primary diseases, adequate support treatments, and mechanical ventilation with lung-protective strategies (Ware and Matthay 2000). Higher levels of supplemental oxygen are often required to maintain adequate tissue oxygenation.
Exposure to hyperoxia can induce lung injury with pathological changes similar to those observed in ARDS. Acute exposure to high levels of 95–100 % oxygen has been widely used to induce lung injury in animal models of ALI/ARDS (Matute-Bello et al. 2008). Longer-term exposures to moderate levels of hyperoxia (50–85 %) can induce progressive chronic lung pathology with fibrosis (Holm et al. 2005). A report revealed that even moderate hyperoxia (FiO2 50 %) exacerbates ventilator-induced lung injury (VILI) in a rabbit model (Sinclair et al. 2004). In addition, evidence from clinical studies supports the concept that oxidative stress plays an important role in the pathogenesis of ALI and its sequelae, including pulmonary fibrosis, emphysema, and bronchopulmonary dysplasia (Chang et al. 2003; Montuschi et al. 1998, 2000). Methods to protect lungs from oxygen toxicity and the systemic oxidative stress under conditions requiring mechanical ventilation and high FiO2 are important needs in critical care medicine.
Lactoferrin (LF) is an iron-binding glycoprotein found in milk and various external secretions such as saliva, tears, semen, airway secretions, and the granules of neutrophils. The protein, which is approximately 80 kDa, comprises two homologous lobes with one iron-binding site in each lobe. LF has a number of biological functions, including antimicrobial, anticancer, antioxidant, and immunomodulatory effects (Chen et al. 2004; Yen et al. 2009; Chen et al. 2010). It is considered to be an important component of the first line of host defense. LF levels of biological fluids may greatly increase and represent a marker for different kinds of inflammatory diseases (El-Loly and Mahfouz, 2011) noticeable this is in blood, where the LF concentration in serum can be as low as 0.4–2 mg/L under normal conditions but increase up to 200 mg/L in septicemia (Bagby and Bennett 1982; Nakao et al. 1997). Among patients with ARDS, the concentrations of iron and iron-related proteins including LF in bronchoalveolar lavage are significantly increased (Ghio et al. 2003), implying that iron mobilization and decompartmentation are significant in the pathogenesis of ARDS. Strengthening the host defense mechanisms and maintaining iron balance are potential strategies for the treatment of ALI (Lagan et al. 2008). One previous report revealed that the hypotransferrinemic mice are more resistant to hyperoxic lung injury than wild-type mice. Pulmonary LF and ferritin were found to be significantly higher in homozygote hypotransferrinemic mice than in wild-type mice. The protective effects of LF and ferritin against oxidant stress in the lower respiratory tract were suggested to be the result of their capacity to sequester iron (Yang et al. 1999). To our knowledge, there have been no further investigations of the direct effects of LF on hyperoxic lung injury.
An aerosol delivery system for use in the hyperoxic injury model was developed in our previous study to test the effects of an aerosolized antioxidant on mice (Yen et al. 2011a). The present study investigates the hypothesis that aerosolized bovine LF (bLF), targeted to the respiratory tract, has immunomodulatory effects and can protect the lungs against hyperoxic injury. We found that aerosolized bLF attenuates the severity of injury and fibrosis of lungs, reduces proinflammatory cytokines production, and increases the survival of mice exposed to moderate hyperoxia.
Materials and methods
Ethics statement
All animal protocols of this study were conducted in strict agreement with international ethical standards according to the Animal Research: Reporting In Vivo Experiments (ARRIVE) guidelines (Kilkenny et al. 2010) and were approved by the Institutional Animal Care and Use Committee of National Chung Hsing University, Taiwan (Approval ID number: 99-52).
Experimental animals
Female ICR strain (CD-1) mice weighing 20–25 g at 3–4 weeks of age were purchased from BioLASCO Taiwan Inc. (Taipei, Taiwan). The mice were housed in a specific pathogen-free (SPF)-grade animal facility under a 12-h light/12-h dark cycle at a constant temperature (25 ± 1 °C) until 8 weeks of age, when they are used in the experiment. The mice were provided with food and water ad libitum throughout the experiment.
Hyperoxic exposure and aerosol delivery system
The mice were exposed to room air (normoxia control group) or moderate hyperoxic conditions (FiO2 = 80 %) in a 36 × 20 × 20-cm plexiglass chamber with a hole (2 cm in diameter) to allow the continuous flow of 80 % oxygen (1 L/min) and aerosol into the chamber. The oxygen levels were monitored every hour during the light phase of the cycle with an oxygen analyzer (MiniOX I, MSA Canada Inc., Toronto, ON, Canada). Two ultrasonic nebulizers (SUMO V15, V-Kool Taiwan Inc., Taipei, Taiwan) were used to aerosolize the study drugs. The nebulizers were connected to the oxygen delivery system (Yen et al. 2011a).
Experimental protocol
The aim of the experiment was to test the hypothesis that aerosolized bLF could function as an anti-inflammatory protein in the airways and reduce lung injury and subsequent fibrosis after 7 days of exposure to moderate hyperoxia (FiO2 = 80 %). The mice were divided into three groups: (1) living in normoxic conditions as a normal control group; (2) exposure to hyperoxia and inhalation exposure to phosphate-buffered saline (PBS) as a sham-treated group; (3) exposure to hyperoxia and inhalation exposure to bLF dissolved in PBS (0.0514 mg/mL, bLF purchased from Sigma, St. Louis, MO, USA) as the treated group. At least six mice were included in each group. The bLF solution was freshly prepared every day. The bLF dissolved in 70 mL of PBS or 70 mL of PBS alone was delivered by this aerosol system during a period of 10 h each day. Approximately 25 % of each solution (by weight) was left in the system after the 10 h of aerosolization. The health of mice was monitored twice daily at 7:00 am and 18:00 pm throughout the experimental period. Symptoms were recorded by two independently observers. Survival was also monitored twice daily, and at least six mice from each group were humanely sacrificed at 168 h for the further experimental examinations. Anesthetized mice (intraperitoneal injection of 100 mg/kg ketamine and 5 mg/kg xylacine) were sacrificed by cervical dislocation by experienced researcher, which performed it humanely and effectively.
Bronchoalveolar lavage
The trachea was exposed with a midline incision and cannulated with a modified 21-gauge needle. The bronchoalveolar lavage fluid (BALF) was obtained by four instillations of 1.0 mL of PBS per time. At least 0.5 mL was recovered after each lavage. The BALF was mixed and centrifuged at 500×g for 10 min at 4 °C. The cell pellets were resuspended in 1 mL PBS, and cell counts were performed (Simonson et al. 1997). The supernatant was assayed for total protein using a bicinchoninic acid (BCA) protein assay (Pierce, Rockford, IL, USA).
Immunohistochemical (IHC) staining of bLF
The lung tissues were fixed with paraformaldehyde and embedded in O.C.T. compound (Tissue-TekR; Sakura, Japan), then frozen and microdissected for Immunohistochemical (IHC) analysis (Chen et al. 2008a; Tung et al. 2011). Briefly, 5 μm sections were placed on slides and incubated with rabbit anti-bLF polyclonal first antibody (1:200 dilution; EMD Millipore, Billerica, MA, USA) and biotin-labeled anti-rabbit IgG antibody (1:2,000 dilution; Abcam, Cambridge, MA, USA). The Vectastain ABC kit (Vector Laboratories, Burlingame, CA, USA) was used for bLF staining (Chen et al. 2008b; Yen et al. 2011b).
Pathological histology examination
After sacrificing the mice, the left lobes of the lungs were dissected and inflated with 0.6 mL of 10 % formalin for histological study. Paraffin sections prepared from the lungs were stained with hematoxylin and eosin for evaluation. We assessed the degree of alveolar congestion, hemorrhage, and leukocyte infiltration and the thickness of the alveolar wall (Tung et al. 2011). The lung histopathological images were scored by two individual pathologists. The quantity of the collagen fibers in the lung tissue sections was evaluated using Masson staining as described previously (Chen et al. 2012).
Cytokines assay by real-time RT-PCR
Total RNA from the lung tissues from normoxic and hyperoxic mice was isolated using TRIzol reagent (Invitrogen, Carlsbad, CA, USA). One microgram of total RNA was reverse-transcribed with MuLV reverse transcriptase, and the cDNA was analyzed by real-time PCR using intron-spanning primers as listed in Table 1. Real-time RT-PCR was performed using SYBR Green in a Rotor-Gene™ 6000 (Corbett Life Science, Sydney, Australia). To evaluate gene expression, real-time RT-PCR was performed on three genes (IL-1β, IL-6, and TNF-α) using cDNA from the lung tissues. The β-actin gene was used as an internal control (Tung et al. 2011; Wen et al. 2013).
Apoptosis analysis of lung tissue
Genomic DNA from the lung tissues was extracted and directly analyzed by 1.5 % agarose gel electrophoresis for the oligonucleosomal ladders of fragmented DNA in apoptotic tissues (Ioannou and Chen 1996). A terminal deoxynucleotidyl transferase (TdT) dUTP nick end labeling (TUNEL) assay was performed using the Fluorescein FragEL DNA Fragmentation Detection Kit according to the manufacturer’s (EMD Chemicals Inc., Gibbstown, NJ, USA) instructions. Briefly, 5 μm lung sections were placed on slides and treated with proteinase K (2 μg/mL) at room temperature for 5 min. After the addition of 100 μL of TdT equilibration buffer for 30 min, the sections were incubated with 60 μL of TdT Labeling Reaction Mix at 37 °C for 1 h. The slides were then washed with Tris-buffered saline (TBS), and the stained cells were imaged using microscopy as described previously (Chen et al. 2012).
Statistical analysis
All experimental results were expressed as the mean ± standard error (SE). The significance of the differences was calculated using the General Linear Model (GLM) procedure by Statistics Analysis System (SAS) as described previously (Chen et al. 2003). Differences with p < 0.05 (*) or p < 0.01 (**) were considered to be statistically significant.
Results
Animal model for hyperoxia-induced lung injury and mortality evaluation
Long-term exposure to hyperoxia can induce lung injury with similar pathological changes to those observed in clinical ARDS patients. In this study, we used exposure to a moderate level of hyperoxia (80 %) for 1 week to induce progressive chronic lung pathology with fibrosis in mice. The supplemented oxygen levels were very stable (79.5–81.5 %, Fig. 1a) when monitored with an oxygen analyzer every hour during the light phase of the exposures. When the CD-1 mice (n = 12) were exposed to the hyperoxic conditions (FiO2 = 80 %), mortality reached 2/3 (66.7 %) at day 6 and 4/5 (80.0 %) at day 7 (Fig. 1b). The survival rate of the normal group (normoxia condition) was 100 % after 7 days of exposure. The treatment with aerosolized bLF increased the survival rate to 70.0 % at 168 h of hyperoxia exposure (Fig. 1b), which was significantly higher than that in the control group exposure to PBS by inhalation after 168 h of hyperoxia exposure (20.0 %, p < 0.01).
Establishment of moderate hyperoxia (FiO2 = 80 %)-induced lung injury and survival fraction. a The plot of oxygen levels (FiO2) in hyperoxia chambers mimicking clinical conditions requiring mechanical ventilation and high levels of oxygen supplementation. The oxygen concentration (%) was measured using an oxygen analyzer every hour during the light phase of the environmental cycle. b The effect of aerosolized bLF on survival after 168 h of hyperoxia. PBS inhalation was used as the hyperoxia-induced lung injury control group. Mice housed in the normoxia condition were used as a normal control group. The survival of the bLF-treated and untreated mice after exposure to hyperoxic conditions (n = 12) were monitored daily
The efficiency of aerosolized bLF protein in mice lung tissue
An ultrasonic nebulizer connected to the oxygen delivery system was used for the aerosolization of the bLF protein drug. To evaluate the efficiency of aerosolized bLF in this system, a total of 3.6 mg bLF dissolved in 70 mL PBS was delivered by this aerosol system, and approximately 78 % of the bLF protein was detected in the cage after 10 h of aerosolization (Supplementary Fig. S1). Therefore, this is an effective protein aerosolization system. To assess the efficiency of this aerosol system and the distribution of bLF in the lungs after aerosolization, IHC staining for bLF was performed (n = 6) as shown in Fig. 2. In the bLF-treated group, bLF was present diffusely in lungs, including epithelium of airway, alveolar space, and even interstitium (Fig. 2c) compared with the control group exposure to aerosolized PBS (Fig. 2b). The results demonstrated that the aerosolized bLF can penetrate and deposit in the lung parenchyma. Because the polyclonal antibodies to bLF crossreacted with endogenous LF, a low background of LF was found in the epithelium of the bronchi and bronchioles of the lungs of the normoxia and PBS control groups (Fig. 2a, b).
The distribution of aerosolized bLF in lung tissue assessed by immunohistochemical (IHC) staining after 168 h of hyperoxia. a Image representative of the normoxia control group. b Image representative of the PBS-inhalation untreated control group. Only a few regions of endogenous LF can be detected in the bronchial epithelia as shown in the 400X magnification images (bottom panel) of normoxia and hyperoxia with PBS inhalation. c Image representative of the aerosolized bovine lactoferrin (bLF) group. The exogenous bLF can be strongly detected in the bronchial epithelia, alveoli, and lung parenchyma as indicated in the brown stain signals. Scale bar 200 μm
Anti-inflammatory effect of bLF against hyperoxia-induced lung injury
Histopathological examination of lungs (n = 6) was performed after 168 h of hyperoxia for inflammation analysis. Pulmonary edema and alveolar infiltration of neutrophils were evident in the aerosolized PBS control group (Fig. 3b) but not in the normal lung tissues under normoxia condition (Fig. 3a). The mice from the group that received aerosolized bLF exhibited less neutrophil infiltration and lung edema (Fig. 3c). The total cell count in the BAL fluid, a marker of lung injury, was also significantly lower in the bLF-treated groups compared with the PBS control group (p < 0.01; Fig. 3d).
Effects of aerosolized bLF on lung morphology and neutrophil infiltration in BALF after 168 h of hyperoxia. Lung sections were stained for histology with H&E. The control group of mice exposed to normal oxygen conditions (Normoxia) is shown in the left panels (a). Middle panels (b) and right panels (c) represent the hyperoxia groups (FiO2 = 80 %) treated with PBS or bLF, respectively (n = 6 in each group). Scale bar 200 μm. d Pulmonary leukocyte infiltration was measured as the total cell counts in BALF. *p < 0.05 versus normoxia group; # p < 0.05 versus. hyperoxia/PBS control group
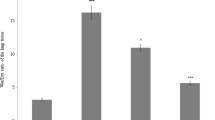
To further evaluate the anti-inflammatory effects of bLF, quantitative real-time RT-PCR was used to measure the levels of inflammatory cytokine expression in the lung tissues of the mice (n = 6; Fig. 4). The inflammatory cytokines (IL-1β, IL-6, and TNF-α) were all elevated in lung tissues in response to the exposure to hyperoxia compared with normoxia (p < 0.01, p < 0.05, and p < 0.05, respectively). The treatment with bLF significantly decreased the levels of IL-1β (Fig. 4a) and IL-6 (Fig. 4b) compared with PBS treatment (p < 0.05), but no significant difference in TNF-α was observed (Fig. 4c).
Effects of aerosolized bLF on inflammatory cytokine mRNA expression levels in the lungs after 168 h of hyperoxia. IL-1β (a), IL-6 (b), and TNF-α (c) mRNA expression levels were measured at day 7 using quantitative RT-PCR from the following three groups: normoxia mice, hyperoxia-exposed mice treated with PBS, and hyperoxia-exposed mice treated with bLF. *p < 0.05 or **p < 0.01 vs. normoxia group; # p < 0.05 versus hyperoxia/PBS control group
Anti-apoptotic effect of bLF in hyperoxia-induced lung injury
Apoptotic DNA fragmentation is a key feature of programmed cell death and is characterized by cytoplasmic condensation, plasma membrane blebbing and nuclear pycnosis. This process leads to nuclear DNA breakdown into multiples of ∼200 bp oligonucleosomal size fragments (arrows in Fig. 5a). The mice exposed to hyperoxia had significantly higher percentages of apoptotic DNA fragmentation than the mice exposed to normoxia (29.1 ± 4.6 vs. 5.6 ± 1.3 %, p < 0.05; Fig. 5b). The mice that received bLF had significantly decreased apoptotic DNA damage relative to the mice that received PBS under the hyperoxia condition (p < 0.05; n = 6; Fig. 5a, b).
Effects of aerosolized bLF on apoptotic DNA damage and cell apoptosis in the lungs after 168 h of hyperoxia. a DNA apoptotic fragmentation was measured using agarose gel electrophoresis. L.M. low molecular weight DNA marker (100-bp DNA ladder); H.M. high molecular weight DNA marker (λ/HindIII). b Quantification of apoptotic DNA fragmentation (%) by densitometry (Kodak 1D software). c The determination of apoptosis was performed by TUNEL assay: apoptotic cells are indicated by the brown staining. d TUNEL-positive pulmonary apoptotic cells were quantified in 10 different fields of each slide. *p < 0.05 or **p < 0.01 versus normoxia group; # p < 0.05 versus hyperoxia/PBS control group. Scale bar 200 μm
The TUNEL assay was used to determine whether bLF influences the apoptosis of the lung cells in the hyperoxia model (Fig. 5c). The mice exposed to hyperoxia had significantly higher numbers of TUNEL-positive cells than the mice exposed to room air (58.3 ± 7.8 cells/field vs. 9.5 ± 0.7 cells/field, p < 0.01). The mice that received bLF had significantly fewer TUNEL-positive cells than the mice that received PBS only under hyperoxia (n = 6; Fig. 5d).
Anti-fibrotic effect of bLF against hyperoxia-induced lung injury
To assess the progressive lung fibrosis induced by long-term exposures to moderate levels of hyperoxia, lung tissues (n = 6) were examined using Masson trichrome staining. The normal lung images under normoxia condition are shown in Fig. 6a. The results showed that mice received PBS only for 7 days post-hyperoxia exposure (Fig. 6b) had significantly more severe fibrosis than the mice that received the bLF treatment (Fig. 6c).
Examination of fibrosis status using Masson trichrome stain in the lungs after 168 h of hyperoxia. Lung tissues from the mice under the normoxia condition (a), hyperoxia-exposed, PBS-inhalation group (b), or hyperoxia-exposed, bLF-treated group (c) were stained with Masson trichrome dye. The fibrotic tissues in the interstitia, peribronchiolar and perivascular areas are indicated by blue trichrome staining in the hyperoxia-exposed, PBS-inhalation group. Scale bar 200 μm
Discussion
There were two major findings in this report. First, aerosolized LF protects mice against the chronic lung injury caused by moderate hyperoxia (FiO2 = 80 %) and attenuates the subsequent fibrosis. The LF aerosol therapy reduces the severity of lung injury as demonstrated by the attenuation of the inflammation, decreased levels of apoptosis and pro-inflammatory cytokine expression in the lungs, and even increased survival rates of the mice subjected to hyperoxia. Second, aerosol therapy targeting the respiratory tract could be an effective and safe administration route for LF, an important antimicrobial, antioxidant, and immunomodulatory protein in airways. The aerosolized LF can penetrate and deposit in the lung parenchyma, as demonstrated by the IHC staining of LF.
LF has host-protecting properties due to its immunomodulatory action and also acts as a promoter of the immune system. LF promotes the maturation of T cell precursors into competent T helper cells and stimulates the differentiation of immature B cells into functional antigen presenting cells (Actor et al. 2009). In our recent studies, a high dose of porcine LF led to a significant increase in antibody concentration in a chicken model (Hung et al. 2010a). LF at either low or high doses enhances the expression of interferon-γ and IL-12, driving T lymphocytes toward Th1 rather than Th2 cells, and enhances the immunity against microbial agents (Hung et al. 2010b).
Many studies including this report confirm the anti-inflammatory effect of LF. Intra-articular injection of human LF (hLF) into mice with collagen-induced or septic arthritis reduces joint inflammation (Guillen et al. 2000). In particular, oral administration of bLf decreases serum IL-6 in anemic pregnant women (Paesano et al. 2009; 2010a, b; 2012). Topical administration of hLF prior to sensitization reduces allergen-induced Langerhans cell migration and cutaneous inflammation in humans (Griffiths et al. 2001). We have previously demonstrated that oral administration of LF decrease the severity of lung inflammation in infectious model (Yen et al. 2009). This study further revealed that aerosolized LF directly attenuates the inflammation in lungs after hyperoxic exposure, at least partially by decreasing the production of pro-inflammatory cytokines.
The mechanism of the anti-inflammatory effects of LF is still complex and not well understood at present. One potential mechanism is through the sequestration of “free” iron at inflammatory site, thus preventing the Fenton reaction, which results in iron-catalyzed formation of damaging free radicals that trigger more inflammatory responses (Brock 2002; Kruzel et al. 2007). The other anti-inflammatory effect of LF may involve the inhibition of the production of pro-inflammatory cytokines, including TNF-α, IL-1β, and IL-6 (Ward et al. 2005; Haversen et al. 2002; Kruzel et al. 2002). Our report revealed that aerosolized bLF had inhibitory effects on IL-1β and IL-6, but no significant effect on TNF-α. TNF-α is a very early pro-inflammatory cytokine, so it may not be easy to detect the change of TNF-α after 7 days of exposure to hyperoxic. The inhibitory effect on the cytokines may be a result of LF translocation to the nucleus, where it prevents NF-κB activation (Ando et al. 2010), or via receptor-mediated signaling pathways. Recent studies have implied that the immunomodulatory effects of LF are associated with the Toll-like receptor (TLR) pathway (Ando et al. 2010; Puddu et al. 2011; Curran et al. 2006). Toll-like receptor 4 (TLR4) was found not only to be the principal receptor for bacterial lipopolysaccharide (LPS) but also to be activated by non-infectious stimuli including hyperoxia (Xiang et al. 2010; Jiang et al. 2006).
Aerosol therapy with LF could be a novel therapeutic modality for oxidative lung injury. Reactive oxygen species (ROS) have been implicated in the pathogenesis of various forms of lung injury, so therapeutic agents that can supplement or substitute for endogenous antioxidants that are depleted or overwhelmed during the disease process is a promising strategy of treatment for lung injury (Asikainen and White 2005). An ideal antioxidant therapeutic proteins or peptide, either natural or synthetic, should have good bioavailability and efficiency in scavenging ROS, and it should effectively penetrate the lungs. The agents should be stable, non-toxic, and nonimmunogenic and should preferably not interfere the normal antimicrobial mechanisms which ROS are involved. Our results demonstrated that aerosolized LF could integrate into the lung parenchyma and attenuate lung injury, apoptosis, and the subsequent fibrosis and even reduce mortality without evident systemic side effects. In particular, LF is a natural immune promoter and antimicrobial protein that could avoid the immunosuppressive effects of antioxidant treatments.
The delivery of aerosol drugs to the respiratory tract has some advantages, including rapid onset, smaller required doses, and a local pulmonary effect with fewer systemic side effects. The procedure is painless and relatively convenient (Yen et al. 2011a). Aerosol therapy can avoid the first-pass effect (metabolism by the liver when the drug is taken orally and absorbed into the portal system), thus ensuring that there is a prolonged effect of the drug on the respiratory system. In this study, we targeted the airways and alveoli by the administration of LF to investigate the protective effect of LF against external insults. Thermal denaturation temperature (Tm) data reveals that bovine LF is the most stable with a Tm of 90 ± 1 °C at pH 7.0. The Tm is reduced gradually when the pH is gradually decreased or increased (Sreedhara et al. 2010). The pH of airway surface mucosa is approximately 6.85. To maximize the bioavailability of bLF in our aerosol delivery system, we used PBS, pH 7.0, as the solvent and kept the aerosol temperature not higher than 25 °C.
In conclusion, we have successfully established an aerosol therapeutic system for bovine LF. Aerosolized LF protected the lungs against oxygen toxicity and reduced mortality in a moderate hyperoxic model. The results of this study are encouraging. The aerosol therapy with LF could be used clinically for reducing oxygen toxicity in patients undergoing mechanical ventilation, attenuating lung injury induced by oxidants.
References
Actor JK, Hwang SA, Kruzel ML (2009) Lactoferrin as a natural immune modulator. Curr Pharm Des 15:1956–1973
Ando K, Hasegawa K, Shindo K, Furusawa T, Fujino T, Kikugawa K, Nakano H, Takeuchi O, Akira S, Akiyama T, Gohda J, Inoue J, Hayakawa M (2010) Human lactoferrin activates NF-kappaB through the toll-like receptor 4 pathway while it interferes with the lipopolysaccharide-stimulated TLR4 signaling. FEBS J 277:2051–2066
Asikainen TM, White CW (2005) Antioxidant therapy for lung injury. In: Notter RH, Finkelstein JN, Holm BA (eds) Lung injury: mechanisms, pathophsiology, and therapy. Tayler & Francis Group Press, NY, pp 665–703
Bagby GC Jr, Bennett RM (1982) Feedback regulation of granulopoiesis: polymerization of lactoferrin abrogates its ability to inhibit CSA production. Blood 60:108–112
Brock JH (2002) The physiology of lactoferrin. Biochem Cell Biol 80:1–6
Chang LY, Subramaniam M, Yoder BA, Day BJ, Ellison MC, Sunday ME, Crapo JD (2003) A catalytic antioxidant attenuates alveolar structural remodeling in bronchopulmonary dysplasia. Am J Respir Crit Care Med 167:57–64
Chen CM, Chen HL, Hsiau TH, Hsiau AH, Shi H, Brock GJ, Wei SH, Caldwell CW, Yan PS, Huang TH (2003) Methylation target array for rapid analysis of CpG island hypermethylation in multiple tissue genomes. Am J Pathol 163:37–45
Chen HL, Lai YW, Yen CC, Lin YY, Lu CY, Yang SH, Tsai TC, Lin YJ, Lin CW, Chen CM (2004) Production of recombinant porcine lactoferrin exhibiting antibacterial activity in methylotrophic yeast, Pichia pastoris. J Mol Microbiol Biotechnol 8:141–149
Chen HL, Wang LC, Chang CH, Yen CC, Cheng WT, Wu SC, Hung CM, Kuo MF, Chen CM (2008a) Recombinant porcine lactoferrin expressed in the milk of transgenic mice protects neonatal mice from a lethal challenge with enterovirus type 71. Vaccine 26:891–898
Chen YJ, Wu CY, Shen JL, Chu SY, Chen CK, Chang YT, Chen CM (2008b) Psoriasis independently associated with hyperleptinemia contributing to metabolic syndrome. Arch Dermatol 144:1571–1575
Chen HL, Lai YW, Chen CS, Chu TW, Lin W, Yen CC, Lin MF, Tu MY, Chen CM (2010) Probiotic lactobacillus casei expressing human lactoferrin elevates antibacterial activity in the gastrointestinal tract. Biometals 23:543–554
Chen JY, Chen HL, Cheng JC, Lin HJ, Tung YT, Lin CF, Chen CM (2012) A Chinese herbal medicine, Gexia-Zhuyu Tang (GZT), prevents dimethylnitrosamine- induced liver fibrosis through inhibition of hepatic stellate cells proliferation. J Ethnopharmacol 142:811–818
Curran CS, Demick KP, Mansfield JM (2006) Lactoferrin activates macrophages via TLR4-dependent and -independent signaling pathways. Cell Immunol 242:23–30
El-Loly MM, Mahfouz MB (2011) Lactoferrin in relation to biological functions and applications: a review. Int J Dairy Sci 6:79–111
Ghio AJ, Carter JD, Richards JH, Richer LD, Grissom CK, Elstad MR (2003) Iron and iron-related proteins in the lower respiratory tract of patients with acute respiratory distress syndrome. Crit Care Med 31:395–400
Griffiths CE, Cumberbatch M, Tucker SC, Dearman RJ, Andrew S, Headon DR, Kimber I (2001) Exogenous topical lactoferrin inhibits allergen-induced Langerhans cell migration and cutaneous inflammation in humans. Br J Dermatol 144:715–725
Guillen C, McInnes IB, Vaughan D, Speekenbrink AB, Brock JH (2000) The effects of local administration of lactoferrin on inflammation in murine autoimmune and infectious arthritis. Arthritis Rheum 43:2073–2080
Haversen L, Ohlsson BG, Hahn-Zoric M, Hanson LA, Mattsby-Baltzer I (2002) Lactoferrin down-regulates the LPS-induced cytokine production in monocytic cells via NF-kappa B. Cell Immunol 220:83–95
Holm BA, Chess PR, Notter RH (2005) Cell and animal models of lung injury. In: Notter RH, Finkelstein JN, Holm BA (eds) Lung injury: mechanisms, pathophsiology, and therapy. Tayler & Francis Group Press, NY, pp 366–370
Hung CM, Wu SC, Yen CC, Lin MF, Lai YW, Tung YT, Chen HL, Chen CM (2010a) Porcine lactoferrin as feedstuff additive elevates avian immunity and potentiates vaccination. Biometals 23:579–587
Hung CM, Yeh CC, Chen HL, Lai CW, Kuo MF, Yeh MH, Lin W, Tu MY, Cheng HC, Chen CM (2010b) Porcine lactoferrin administration enhances peripheral lymphocyte proliferation and assists infectious bursal disease vaccination in native chickens. Vaccine 28:2895–2902
Ioannou YA, Chen FW (1996) Quantitation of DNA fragmentation in apoptosis. Nucl Acids Res 24:992–993
Jiang D, Liang J, Li Y, Noble PW (2006) The role of Toll-like receptors in non-infectious lung injury. Cell Res 16:693–701
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG (2010) Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol 8:e1000412
Kruzel ML, Harari Y, Mailman D, Actor JK, Zimecki M (2002) Differential effects of prophylactic, concurrent and therapeutic lactoferrin treatment on LPS-induced inflammatory responses in mice. Clin Exp Immunol 130:25–31
Kruzel ML, Actor JK, Boldogh I, Zimecki M (2007) Lactoferrin in health and disease. Postepy Hig Med Dosw (Online) 61:261–267
Lagan AL, Melley DD, Evans TW, Quinlan GJ (2008) Pathogenesis of the systemic inflammatory syndrome and acute lung injury: role of iron mobilization and decompartmentalization. Am J Physiol Lung Cell Mol Physiol 294:161–174
Matute-Bello G, Frevert CW, Martin TR (2008) Animal models of acute lung injury. Am J Physiol Lung Cell Mol Physiol 295:L379–L399
Montuschi P, Ciabattoni G, Paredi P, Pantelidis P, du Bois RM, Kharitonov SA, Barnes PJ (1998) 8-isoprostane as a biomarker of oxidative stress in interstitial lung diseases. Am J Respir Crit Care Med 158:1524–1527
Montuschi P, Collins JV, Ciabattoni G, Lazzeri N, Corradi M, Kharitonov SA, Barnes PJ (2000) Exhaled 8-isoprostane as an in vivo biomarker of lung oxidative stress in patients with COPD and healthy smokers. Am J Respir Crit Care Med 162:1175–1177
Nakao K, Imoto I, Gabazza EC, Yamauchi K, Yamazaki N, Taguchi Y, Shibata T, Takaji S, Ikemura N, Misaki M (1997) Gastric juice levels of lactoferrin and Helicobacter pylori infection. Scand J Gastroenterol 32:530–534
Paesano R, Pietropaoli M, Gessani S, Valenti P (2009) The influence of lactoferrin, orally administered, on systemic iron homeostasis in pregnant women suffering of iron deficiency and iron deficiency anaemia. Biochimie 91:44–51
Paesano R, Berlutti F, Pietropaoli M, Goolsbee W, Pacifici E, Valenti P (2010a) Lactoferrin efficacy versus ferrous sulfate in curing iron disorders in pregnant and non-pregnant women. Int J Immunopathol Pharmacol 23:577–587
Paesano R, Berlutti F, Pietropaoli M, Pantanella F, Pacifici E, Goolsbee W, Valenti P (2010b) Lactoferrin efficacy versus ferrous sulfate in curing iron deficiency and iron deficiency anemia in pregnant women. Biometals 23:411–417
Paesano R, Pietropaoli M, Berlutti F, Valenti P (2012) Bovine lactoferrin in preventing preterm delivery associated with sterile inflammation. Biochem Cell Biol 90:468–475
Puddu P, Latorre D, Carollo M, Catizone A, Ricci G, Valenti P, Gessani S (2011) Bovine lactoferrin counteracts Toll-like receptor mediated activation signals in antigen presenting cells. PLoS One 6:e22504
Simonson SG, Welty-Wolf KE, Huang YC, Taylor DE, Kantrow SP, Carraway MS, Crapo JD, Piantadosi CA (1997) Aerosolized manganese sod decreases hyperoxic pulmonary injury in primates. I. Physiology and biochemistry. J Appl Physiol 83:550–558
Sinclair SE, Altemeier WA, Matute-Bello G, Chi EY (2004) Augmented lung injury due to interaction between hyperoxia and mechanical ventilation. Crit Care Med 32:2496–2501
Sreedhara A, Flengsrud R, Langsrud T, Kaul P, Prakash V, Vegarud GE (2010) Structural characteristic, pH and thermal stabilities of apo and holo forms of caprine and bovine lactoferrins. Biometals 23:1159–1170
Tung YT, Chen HL, Lai CW, Shen CJ, Lai YW, Chen CM (2011) Curcumin reduces pulmonary tumorigenesis in vascular endothelial growth factor (VEGF)-overexpressing transgenic mice. Mol Nutr Food Res 55:1036–1043
Ward PP, Paz E, Conneely OM (2005) Multifunctional roles of lactoferrin: a critical overview. Cell Mol Life Sci 62:2540–2548
Ware LB, Matthay MA (2000) The acute respiratory distress syndrome. N Engl J Med 342:1334–1349
Wen ST, Chen W, Chen HL, Lai CW, Yen CC, Lee KH, Wu SC, Chen CM (2013) Amniotic fluid stem cells from EGFP transgenic mice attenuate hyperoxia-induced acute lung injury. PLoS One 8:e75383
Xiang M, Fan J, Fan J (2010) Association of Toll-like receptor signaling and reactive oxygen species: a potential therapeutic target for posttrauma acute lung injury. Mediators Inflamm 2010:916425
Yang F, Coalson JJ, Bobb HH, Carter JD, Banu J, Ghio AJ (1999) Resistance of hypotransferrinemic mice to hyperoxia-induced lung injury. Am J Physiol 277:L1214–L1223
Yen CC, Lin CY, Chong KY, Tsai TC, Shen CJ, Lin MF, Su CY, Chen HL, Chen CM (2009) Lactoferrin as a natural regimen for selective decontamination of the digestive tract: recombinant porcine lactoferrin expressed in the milk of transgenic mice protects neonates from pathogenic challenge in the gastrointestinal tract. J Infect Dis 199:590–598
Yen CC, Lai YW, Chen HL, Lai CW, Lin CY, Chen W, Kuan YP, Hsu WH, Chen CM (2011a) Aerosolized human extracellular superoxide dismutase prevents hyperoxia-induced lung injury. PLoS One 6:e26870
Yen CC, Shen CJ, Hsu WH, Chang YH, Lin HT, Chen HL, Chen CM (2011b) Lactoferrin: an iron-binding antimicrobial protein against Escherichia coli infection. Biometals 24:585–594
Acknowledgments
The authors would like to thank Prof. Jiung-Wang Liao for his help with the pathology analysis and our colleagues (Drs. Yu-Tang Tung, and Cheng-Wei Lai) in the Molecular Embryology & DNA Methylation Laboratory for their help with discussions and technical issues. We also would like to thank the Biostatic Center of China Medical University for assistance with the statistical analysis. This research was supported by grant NSC-95-2313-B-005-012 from the National Science Council, grant COA-97-6.2.1-U1(9) from the Council of Agriculture, and the Ministry of Education, Taiwan, Republic of China, under the aiming top university plan (ATU-101-S-0508).
Author information
Authors and Affiliations
Corresponding author
Additional information
Hsiao-Ling Chen, Chih-Ching Yen and Shih-Ming Wang have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10534_2014_9750_MOESM1_ESM.tif
Supplemental Figure S1. Image of the ultrasonic nebulizer system to aerosolize bLF for the murine model of hyperoxia-induced lung injury and measurement of its efficiency for nebulization of bLF. An ultrasonic nebulizer was connected to the oxygen delivery system to aerosolize the bLF protein drug. The efficiency of aerosolized bLF in this system was measured. A total of 3.6 mg bLF dissolved in 70 mL PBS was delivered by this aerosol system and approximately 78 % of bLF protein was detected in the cage after 10 h of aerosolization. (TIFF 407 kb)
Rights and permissions
About this article
Cite this article
Chen, HL., Yen, CC., Wang, SM. et al. Aerosolized bovine lactoferrin reduces lung injury and fibrosis in mice exposed to hyperoxia. Biometals 27, 1057–1068 (2014). https://doi.org/10.1007/s10534-014-9750-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10534-014-9750-7