Abstract
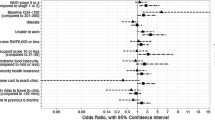
Community-based accompaniment (CBA) has been associated with improved antiretroviral therapy (ART) patient outcomes in Rwanda. In contrast, distance has generally been associated with poor outcomes. However, impact of distance on outcomes under the CBA model is unknown. This retrospective cohort study included 537 adults initiated on ART in 2012 in two rural districts in Rwanda. The primary outcomes at 6 months after ART initiation included overall program status, missed a visit and missed three consecutive visits. The associations between cost surface distance (straight-line distance adjusted for surface features) and outcomes were assessed using logistic regression, controlling for potential confounders. Died/lost-to-follow-up and missed three consecutive visits were not associated with distance. Patients within 0–1 km cost surface distance were significantly more likely to miss a visit, potentially due to stigma of attending clinic within one’s community. These results suggest that CBA may mediate the impact of long distances on outcomes.
Resumen
El Acompañamiento Basado en la Comunidad (ABC) se ha asociado con mejores resultados para pacientes en Ruanda con tratamiento antirretroviral (TARGA). En contraste, la distancia entre una aldea y la clínica donde buscan tratamiento los pacientes generalmente se ha asociado con resultados no favorables. Sin embargo, el impacto que tiene la distancia sobre el resultado de tratamiento bajo el modelo ABC es desconocido. Este estudio retrospectivo de cohorte incluyó a 537 adultos que iniciaron tratamiento TARGA en 2012 en dos distritos rurales de Ruanda. Los indicadores primarios a los seis meses después del inicio de tratamiento TARGA incluyen estado general en el programa: perdida de una visita o perdida de tres visitas consecutivas. Las asociaciones entre la distancia del recorrido del camino (la distancia de una línea recta ajustada por características de la superficie) y resultados de tratamiento se evaluaron mediante regresión logística, controlando los posibles factores de confusión. Factores como fallecido, inubicable y perdida de tres visitas consecutivas no se asociaron con la distancia. Pacientes dentro de 0-1km de distancia del recorrido del camino tenían mayor probabilidad de perder una visita, posiblemente debido al estigma de asistir a la clínica dentro de su comunidad. Estos resultados sugieren que el ABC podría minimizar el impacto que tienen las distancias largas sobre los resultados de tratamiento.



Similar content being viewed by others
References
Ford N, Calmy A, Mills EJ. The first decade of antiretroviral therapy in Africa. Global Health. 2011;7:33.
UNAID. Mdg 6: 15 years, 15 lessons of hope from the AIDS response. http://www.unaids.org/sites/default/files/media_asset/20150714_FS_MDG6_Report_en.pdf. Accessed 15 Nov 2015.
Weiser S, Wolfe W, Bangsberg D, Thior I, Gilbert P, Makhema J, et al. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. J Acquir Immune Defic Syndr. 2003;34:281–94.
Rich ML, Miller AC, Niyigena P, Franke MF, Niyonzima JB, Socci A, et al. Excellent clinical outcomes and high retention in care among adults in a community-based HIV treatment program in rural Rwanda. J Acquir Immune Defic Syndr. 2012;59:35–42.
Jacobs B, Ir P, Bigdeli M, Annear PL, Van Damme W. Addressing access barriers to health services: an analytical framework for selectingappropriate interventions in low-income Asian countries. Health Policy Plan. 2012;27:288–300.
Levesque J, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18.
Lifson AR, Demissie W, Tadesse A, Ketema K, May R, Yakob B, et al. Barriers to retention in care as perceived by persons living with HIV in rural Ethiopia: focus group results and recommended strategies. J Int Assoc Provid AIDS Care. 2012;12:32–8.
Mutasa-Apollo T, Shiraishi RW, Takarinda KC, Dzangare J, Mugurungi O, Murungu J, et al. Patient retention, clinical outcomes and attrition-associated factors of HIV-infected patients enrolled in Zimbabwe’s national antiretroviral therapy programme, 2007-2010. PLoS ONE. 2014;9:2007–10.
Charurat M, Oyegunle M, Benjamin R, Habib A, Eze E, Ele P, et al. Patient retention and adherence to antiretrovirals in a large antiretroviral therapy program in Nigeria: a longitudinal analysis for risk factors. PLoS ONE. 2010;5:1–8.
Carlucci JG, Kamanga A, Sheneberger R, Shepherd BE, Jenkins CA, Spurrier J, et al. Predictors of adherence to antiretroviral therapy in rural Zambia. J Acquir Immune Defic Syndr. 2009;47:615–22.
Karcher H, Omondi A, Odera J, Kunz A, Harms G. Risk factors for treatment denial and loss to follow-up in an antiretroviral treatment cohort in Kenya. Trop Med Int Health. 2007;12:687–94.
Reda A, Biadgilign S. Determinants of adherence to antiretroviral therapy among HIV-infected patients in Africa. AIDS Res Treat. 2012. doi:10.1155/2012/574656.
Van Dijk JH, Sutcliffe CG, Munsanje B, Hamangaba F, Thuma PE, Moss WJ. Barriers to the care of HIV-infected children in rural Zambia: a cross-sectional analysis. BMC Infect Dis. 2009;9:169.
Duff P, Kipp W, Wild TC, Rubaale T, Okech-Ojony J. Barriers to accessing highly active antiretroviral therapy by HIV-positive women attending an antenatal clinic in a regional hospital in western Uganda. J Int AIDS Soc. 2010;13:37.
Weiser S, Wolfe W, Bangsberg D, Thior I, Gilbert P. Barriers to antiretroviral adherence for patients living with HIV. Clin Sci. 2003;34:281–8.
Miller CM, Ketlhapile M, Rybasack-Smith H, Rosen S. Why are antiretroviral treatment patients lost to follow-up? A qualitative study from South Africa. Trop Med Int Health. 2010;15(Suppl 1):48–54.
Lankowski AJ, Siedner MJ, Bangsberg DR, Tsai AC. Impact of geographic and transportation-related barriers on HIV outcomes in sub-Saharan Africa: a systematic review. AIDS Behav. 2014;18:1199–223.
Bangsberg DR, Tsai AC. Impact of geographic and transportation-related barriers on HIV outcomes in sub-Saharan Africa: a systematic review. AIDS Behav. 2014;18:1199.
Amuron B, Namara G, Birungi J, Nabiryo C, Levin J, Grosskurth H, et al. Mortality and loss-to-follow-up during the pre-treatment period in an antiretroviral therapy programme under normal health service conditions in Uganda. BMC Public Health. 2009;9:290.
Parkes-Ratanshi R, Bufumbo L, Nyanzi-Wakholi B, Levin J, Grosskurth H, Lalloo DG, et al. Barriers to starting ART and how they can be overcome: individual and operational factors associated with early and late start of treatment. Trop Med Int Health. 2010;15:1347–56.
McGuire M, Munyenyembe T, Szumilin E, Heinzelmann A, Le Paih M, Bouithy N, et al. Vital status of pre-ART and ART patients defaulting from care in rural Malawi. Trop Med Int Health. 2010;15:55–62.
Bedelu M, Ford N, Hilderbrand K, Reuter H. Implementing antiretroviral therapy in rural communities: the Lusikisiki model of decentralized HIV/AIDS care. Infect Dis. 2007;196:464–8.
National Institute of Statistics of Rwanda. Fourth population and housing census. Kigali, Rwanda: National Institute of Statistics of Rwanda; 2012.
Rwanda Ministry of Health. Rwanda health financing policy. Kigali, Rwanda: Rwanda Ministry of Health; 2009.
Binagwaho A, Farmer PE, Nsanzimana S, Karema C, Gasana M, de Dieu Ngirabega J, et al. Rwanda 20 years on: investing in life. Lancet. 2014;6736:1–7.
WHO. Rwanda statistics summary (2002–present). http://apps.who.int/gho/data/node.country.country-RWA?lang=en. Accessed 25 May 2015.
Nuwagaba-Biribonwoha H, Jakubowski A, Mugisha V, Basinga P, Asiimwe A, Nash D, et al. Low risk of attrition among adults on antiretroviral therapy in the Rwandan national program: a retrospective cohort analysis of 6, 12, and 18 month outcomes. BMC Public Health. 2014;14:889.
Rwanda Ministry of Health. TRACNet: key indicators. http://www.moh.gov.rw/index.php?id=3. Accessed 12 May 2015.
Rwanda Ministry of Health. National community health policy. Kigali, Rwanda: Rwanda Ministry of Health; 2008.
Rwanda Ministry of Health. National guidelines for comprehensive care of people living with HIV in Rwanda. Kigali, Rwanda: Rwanda Ministry of Health; 2011.
Franke MF, Kaigamba F, Socci AR, Hakizamungu M, Patel A, Bagiruwigize E, et al. Improved retention associated with community-based accompaniment for antiretroviral therapy delivery in rural Rwanda. Clin Infect Dis. 2013;56:319–26.
Thomson DR, Rich ML, Kaigamba F, Socci AR, Hakizamungu M, Bagiruwigize E, et al. Community-based accompaniment and psychosocial health outcomes in HIV-infected adults in Rwanda: a prospective study. AIDS Behav. 2014;18:368–80.
Gupta N, Munyaburanga C, Mutagoma M, Niyigena JW, Kayigamba F, Franke MF, et al. Community-based accompaniment mitigates predictors of negative outcomes for adults on antiretroviral therapy in rural Rwanda. AIDS Behav. 2015;19:1–8.
Partners In Health. Program management guide. Boston: PIH Rep; 2011.
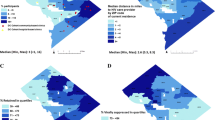
Munyaneza F, Hirschhorn LR, Amoroso CL, Nyirazinyoye L, Birru E, Mugunga JC, et al. Leveraging community health worker system to map a mountainous rural district in low resource setting: a low-cost approach to expand use of geographic information systems for public health. Int J Health Geogr. 2014;13:49.
Foltête JC, Berthier KCJ. Cost distance defined by a topological function of landscape. Ecol Model. 2008;210:104–14.
Meyerson A., Munagala K, Plotkin S. Cost-distance: two metric network design. In: Proceedings of 41st annual symposium on foundation of computer science, Los Angeles, USA; 2000.
Brennan AT, Maskew M, Sanne I, Fox MP. The importance of clinic attendance in the first six months on antiretroviral treatment: a retrospective analysis at a large public sector HIV clinic in South Africa. J Int AIDS Soc. 2010;13:49.
Van Lettow M, Åkesson A, Martiniuk ALC, Ramsay A, Chan AK, Anderson ST, et al. Six-month mortality among HIV-infected adults presenting for antiretroviral therapy with unexplained weight loss, chronic fever or chronic diarrhea in Malawi. PLoS ONE. 2012;7:1–8.
Hirschhorn LR, Poles G, Li M, Siril H, Mhalu A, Hawkins C, et al. Factors associated with different patterns of non-adherence to HIV care in Dar es Salaam, Tanzania. J Int Assoc Provid AIDS Care. 2014;23:333–6.
Farmer P, Léandre F, Mukherjee JS, Claude MS, Nevil P, Smith-Fawzi MC, et al. Community-based approaches to HIV treatment in resource-poor settings. Lancet. 2001;358:404–9.
Unge C, Johansson A, Zachariah R, Some D, Van Engelgem I, Ekstrom AM. Reasons for unsatisfactory acceptance of antiretroviral treatment in the urban Kibera slum, Kenya. AIDS Care. 2008;20:146–9.
Treves-kagan S, Steward WT, Ntswane L, Haller R, Gilvydis JM, Gulati H, et al. Why increasing availability of ART is not enough: a rapid, community-based study on how HIV-related stigma impacts engagement to care in rural South Africa. BMC Public Health. 2016;16:87.
Tene G, Lahuerta M, Teasdale C, Mugisha V, Kayonde L, Muhayimpundu R, et al. High retention among HIV-infected children in Rwanda during scale-up and decentralization of HIV care and treatment programs, 2004 to 2010. Pediatr Infect Dis J. 2013;32:e341–7.
Okwaraji YB, Cousens S, Berhane Y, Mulholland K, Edmond K. Effect of geographical access to health facilities on child mortality in rural Ethiopia: a community based cross sectional study. PLoS ONE. 2012;7:1–8.
Acknowledgement
We gratefully acknowledge the financial support from the Doris Duke Charitable Foundation’s African Health Initiative, through PHIT Partnership funding for implementation of this study and for a Master’s degree scholarship at the University of Rwanda, College of Medicine and Health Sciences, School of Public Health. We would like to thank PIH/IMB and the RMoH leadership of Rwinkwavu and Kirehe Hospital affiliated Hospitals for technical and administrative support. BHG received support from the Global Health Research Core at Harvard Medical School. We thank Dr. Felix Rwabukwisi Cyanamatare, Peter Niyigena, and Jean Paul Umugisha who provided ideas on the methods, and Jackline Odhiambo who provided support in editing the manuscript.
Funding
This work was supported by the Doris Duke Charitable Foundation, Grant Number 2009057. BHG received support from the Global Health Research Core at Harvard Medical School.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
All authors declare that they have no competing interests.
Ethical approval
This study was reviewed and approved by the institutional review board of the University of Rwanda, College of Medicine and Health Sciences, School of Public Health in Kigali, Rwanda (007/UR/CMHS/SPH/2014), and the Institutional Review Board at Brigham and Women’s Hospital in Boston, Massachusetts (2012P000249/BWH). Patients’ names and their program identifiers were not extracted from the EMR system to ensure confidentiality.
Additional information
Lisa R. Hirschhorn and Bethany L. Hedt-Gauthier contributed equally to this article.
Rights and permissions
About this article
Cite this article
Munyaneza, F., Ntaganira, J., Nyirazinyoye, L. et al. Community-Based Accompaniment and the Impact of Distance for HIV Patients Newly Initiated on Antiretroviral Therapy: Early Outcomes and Clinic Visit Adherence in Rural Rwanda. AIDS Behav 22, 77–85 (2018). https://doi.org/10.1007/s10461-016-1658-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1658-5